Abstract
Background
The discrepancy between demand and supply for liver transplants (LT) has led to an increased transplantation of organs from extended criteria donors (ECD).
Methods
In this single center retrospective analysis of 122 cadaveric LT recipients, we investigated predictors of postreperfusion syndrome (PRS) including transplant liver quality categorized by both histological assessment of steatosis and subjective visual assessment by the transplanting surgeon using multivariable regression analysis. Furthermore, we describe the relevance of PRS during the intraoperative and postoperative course of LT recipients.
Results
53.3% (n = 65) of the patients suffered from PRS. Risk factors for PRS were visually assessed organ quality of the liver grafts (acceptable: OR 12.2 [95% CI 2.43–61.59], P = 0.002; poor: OR 13.4 [95% CI 1.48–121.1], P = 0.02) as well as intraoperative norepinephrine dosage before reperfusion (OR 2.2 [95% CI 1.26–3.86] per 0.1 μg kg− 1 min− 1, P = 0.01). In contrast, histological assessment of the graft was not associated with PRS. LT recipients suffering from PRS were hemodynamically more instable after reperfusion compared to recipients not suffering from PRS. They had lower mean arterial pressures until the end of surgery (P < 0.001), received more epinephrine and norepinephrine before reperfusion (P = 0.02 and P < 0.001, respectively) as well as higher rates of continuous infusion of norepinephrine (P < 0.001) and vasopressin (P = 0.02) after reperfusion. Postoperative peak AST was significantly higher (P = 0.001) in LT recipients with PRS. LT recipients with intraoperative PRS had more postoperative adverse cardiac events (P = 0.05) and suffered more often from postoperative delirium (P = 0.04).
Conclusions
Patients receiving ECD liver grafts are especially prone to PRS. Anesthesiologists should keep these newly described risk factors in mind when preparing for reperfusion in patients receiving high-risk organs.
Similar content being viewed by others
Background
According to the Organ Procurement and Transplantation Network of the United States (US) Department of Health and Human Services, the numbers of liver transplantations (LT) in the US have constantly been rising since the beginning of LT [1]: In 2016, a total of 7841 LTs were performed in the US. By contrast, the numbers of LTs in Germany and in the Eurotransplant region have been decreasing since a peak in 2010 [2, 3]. The decreasing organ donations combined with the persisting high morbidity and mortality of patients on the waiting list has led to a discrepancy between organ supply and demand [2, 4] and therefore to the more frequent acceptance extended criteria donors (ECD) to the pool of eligible donors [5, 6].
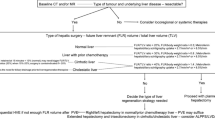
The most critical intraoperative moment for the anesthesiologist during LT is the reperfusion of the liver graft. An immediate and severe complication following reperfusion is hemodynamic instability, the so called post-reperfusion syndrome (PRS). PRS is defined as a decrease of mean arterial pressure (MAP) of more than 30% during the first 5 min after reperfusion and continuing for at least 1 min [7,8,9,10,11,12]. PRS occurs in around 10–60% of LT recipients [8, 9, 13]. Several risk factors for PRS have been described: Older donor age, higher donor risk index, longer cold ischemic time (CIT), severity of the recipient’s liver disease, operation time and technique, hemodynamics at time of reperfusion, and steatosis of the graft organ [8, 13,14,15,16,17,18,19,20]. The mechanisms of PRS appear to be complex and not fully understood [10, Predictors of postreperfusion syndrome In order to identify predictors of PRS we conducted a binary logistic regression analysis with PRS as dependent variable introducing known risk factors for PRS in the model (Table 2). Only visually assessed acceptable (OR 12.2 [95% CI 2.43–61.59], P = 0.002) or poor (OR 13.4 [95% CI 1.48–121.1], P = 0.02) quality of the donor organ and norepinephrine dosage before reperfusion (OR 2.2 [95% CI 1.26–3.86] per 0.1 μg kg− 1 min− 1, P = 0.01) predicted the occurrence of PRS. Interestingly, the histological assessment of donor organ’s steatosis was not a good predictor for PRS. This was not due to collinearity of the variables: the visual and histological assessment differed significantly (p < 0.001) and agreed poorly (cohen’s kappa 0.31, Table 3). For example, 21 of 122 donor organs were staged as acceptable or poor by visual inspection but classified as stage 1 steatosis by histological assessment. LT recipients with PRS were hemodynamically more unstable after reperfusion until the end of surgery compared to patients without PRS (Fig. 2): Recipients with PRS had lower MAPs after reperfusion (P < 0.001; Fig. 2a) and accordingly received higher infusion of continuous norepinephrine (P < 0.001, Fig. 2b) and vasopressin (P < 0.001; Fig. 2c) compared to patients without PRS. Heart rate and continuous epinephrine infusion after reperfusion did not differ in LT recipients with and without PRS (Fig. 2d and e). At the time of reperfusion of the liver transplant, recipients with PRS received higher boli of norepinephrine (1.5 ± 1.6 vs. 0.3 ± 0.4 μg kg− 1, P = < 0.001) and epinephrine (0.3 ± 0.5 vs. 0.1 ± 0.2 μg kg− 1; P = 0.01; Fig. 2f). Hemodynamics. Intraoperative hemodynamics of 122 liver transplant (LT) recipients, 65 with postreperfusion syndrome (PRS, black circles), 57 without postoperative PRS (white circles). LT recipients with PRS were hemodynamically more unstable compared to patients without PRS. Mean arterial pressure after reperfusion was lower (a), accordingly, norepinephrine (b) and vasopressin infusion (c) were higher in LT recipients with PRS compared to recipients without PRS. Heart rate (d) and epinephrine infusion (e) did not differ. At the time of reperfusion, LT recipients with PRS received greater boli of norepinephrine and epinephrine (f). P-values: repeated measures ANOVA; *: post-hoc t-test; mean and standard deviation Furthermore, LT recipients with PRS received more extensive hemotherapy intraoperatively: Compared to patients without PRS, LT recipients with PRS received more platelet concentrates (1.6 ± 1.8 vs. 1.1 ± 1.5 units; P = 0.04; more fibrinogen (3.0 ± 3.2 vs. 1.7 ± 1.2 g; P = 0.01) and more PCC (1313 ± 1610 vs. 579 ± 1133 IU; P = 0.01; Table 4). There was no significant difference in the amount of RBC and FFP administered as well as in other intraoperative postreperfusion adverse events (Table 4). LT recipients with PRS demonstrated a more severe organ damage after transplantation: During the first three postoperative days, AST was higher in patients with PRS (P = 0.02; Fig. 3a), as was ALT, but without statistical significance (P = 0.40; Fig. 3b). LT recipients with and without PRS did not differ in bile retention, as postoperative serum bilirubin concentrations were similar (Fig. 3c). Recipients with PRS postoperatively had poorer organ function as hemostasis was poorer compared to recipients without PRS (P = 0.01; Fig. 3d). The inflammation marker procalcitonin as well as the kidney function marker serum creatinine did not differ in LT recipients with and without PRS (Fig. 3e and f). Clinical chemistry. Postoperative clinical chemistry of 122 liver transplant (LT) recipients, 65 with postreperfusion syndrome (PRS, black circles), 57 without postoperative PRS (white circles). LT recipients with PRS suffered from greater postoperative transplant damage and poorer transplant function during the postoperative course: Aspartat transferase blood concentration was higher (a) and blood hemostasis was poorer (d) compared to LT recipients without postreperfusion syndrome (alanine transferase was higher but did not reach significance, (b) LT recipients with and without PRS did not differ in gall retention (c). Inflammation marker procalcitonin (e) and kidney function marker creatinine (f) were peaking higher during the postoperative course in LT recipients with PRS compared to recipients without PRS but did not reach statistical significance. P-values: repeated measures ANOVA; *: post-hoc t-test; mean and standard deviation Regarding postoperative adverse events, LT recipients with PRS suffered more often from postoperative delirium (8/65 vs. 1/57, 12.3% vs. 1.8%; P = 0.04) and major cardiovascular events (11/65 vs. 3/57, 16.9% vs. 5.3%; P = 0.05; Table 5). LT recipients with PRS also tended to have a longer ICU LOS (11.7 ± 17.0 vs. 9.7 ± 15.7; P = 0.09; Table 5). A Kaplan-Meier survival analysis for LT recipient survival (Fig. 4a) and graft survival (Fig. 4b) did not show significant differences. Survival. Kaplan-Meier survival analysis of 122 liver transplant (LT) recipients, 65 with postreperfusion syndrome (PRS; solid line) and 57 with PRS (broken line). Survival analyses were conducted for LT recipient survival (a) as well as graft survival (retransplantation or recipient death; (b) PRS: postreperfusion syndromePostreperfusion syndrome and the intraoperative course after reperfusion
Postreperfusion syndrome and the postoperative course after transplantation
Discussion
In this single center retrospective analysis of 122 LT recipients, we found that approximately half of the patients suffered from PRS (53.3%). Multivariable regression analysis identified two predictors of PRS: Only visually assessed acceptable (OR 12.2, P = 0.002) and poor (OR 13.4, P = 0.02) donor organ quality by the transplanting surgeon and intraoperative norepinephrine infusion rate before reperfusion of the liver transplant (OR 2.2 per 0.1 μg/kg/min, p = 0.01) were associated with the occurrence of PRS. LT recipients suffering from PRS were hemodynamically more instable after reperfusion compared to recipients not suffering from PRS. They had lower MAPs from reperfusion until the end of surgery (P < 0.001). Hence, they received more epinephrine and norepinephrine before reperfusion (P < 0.001 and P = 0.01, respectively) and higher rates of continuous infusion of norepinephrine (P < 0.001) and vasopressin (P = 0.02) after reperfusion of the transplant. Moreover, LT recipients with intraoperative PRS had a more complicated postoperative course compared to recipients without intraoperative PRS: They had more adverse cardiac events (P = 0.05) and suffered more often from postoperative delirium (P = 0.04).
All 122 LT recipients were operated at the same center with the same technique (venovenous/portalvenous bypass) and with uniform anesthesiologic management, guided by a SOP that included instructions for the management of PRS. No changes in operating technique or anesthesiologic management were made during the study period, leading to a homogenous single center study sample. Nevertheless, this study has several weaknesses. Due to the retrospective design of the analyses, data quality could be impaired. Histological data for our analyses was limited to steatosis assessment. Analyses of hemodynamics from hand-written anesthesia protocols are often suspected to present “sugar-coated” hemodynamic values. Although we cannot rule out that this was the case, our data present clinically and empirically plausible hemodynamics. At worst, hemodynamic stability is overestimated and the effects shown are even more pronounced. The fact that this was a single center analysis combined with the uncommon but consistent use of intraoperative venovenous/portalvenous bypass limits the external validity of our results.
Although rather on the top end of the range, PRS incidence of 53% in our sample concurs with several other studies [8, 10, 12, 17, 19]. The pathophysiology of PRS is complex and not entirely understood. The abrupt influx of cold, hyperkalemic and acidic blood into the circulation, air or thrombotic embolization and the release of vasoactive substances from the graft liver contribute to PRS [29,30,31]. The rationale for using a venovenous/portalvenous bypass during the anhepatic phase at our center is to ensure maximum safety of the procedure [24]. The combination of a femoro-brachial and porto-axillary bypass reduces lower limb and mesenterial congestion and therefore reduces the abrupt influx of hyperkalemic and acidic blood into systemic circulation at the time of reperfusion. Nevertheless, the use of a bypass during LT surgery remains controversial [13, 32, 33]. The PRS effect seen in our study is therefore likely to be predominantly caused by vasoactive substances released from the graft. With that in mind, PRS incidence does appear rather high.
A possible explanation for this contradiction may be the fact that we used an extended definition for PRS. PRS is commonly defined as a decrease in MAP of more than 30% from the baseline value for more than one minute during the first five minutes after reperfusion [7, 8, 10,11,12]. We extended the definition for PRS for mainly two reasons. First, the treatment of PRS seeks to preserve hemodynamic stability. At the time of reperfusion, anesthesiologists expect a certain degree of hemodynamic instability and preemptively treat a (soon to be) falling MAP with catecholamines [11], either as bolus or by increasing continuous infusion of the very same. Since this preemptive treatment conceals the occurrence of by-definition-PRS, we added (i) the administration of an intravenous bolus of norepinephrine > 2 μg kg (BW) -1 as well as (ii) the increase of continuous norepinephrine infusion of ≥0.1 μg kg BW− 1 within the first 5 min after reperfusion as new criteria to the definition. Second, our clinical empiricism and the literature have presented cases of prolonged vasodilation after reperfusion [34,35,36]. We thus included (iii) an increase of continuous norepinephrine infusion up to 30 min after reperfusion and (iv) the initiation of continuous vasopressin infusion after reperfusion as additional criteria for PRS. This altered definition impedes comparability with other studies and may overestimate PRS incidence compared to the commonly used definition. However, our data appear clinically plausible and concur with description of hemodynamic recovery after PRS by other authors [17].
In this study, multivariable regression modelling identified one donor related and one recipient related predictor of PRS: graft quality – visually assessed by the transplanting surgeon – and cumulative intraoperative norepinephrine dosage before reperfusion of the liver graft. The variety of risk factors and risk prediction models described in different studies suggests that PRS may occur in an unpredictable manner or may be highly subjective to center-specific effects [8, 13,14,15,16,17,18,19,20, 22]. The most frequent reported risk factors for PRS are longer CIT [15, 16, 18, 20] and intraoperative hemodynamics prior to reperfusion [14, 15, 17, 20], followed by graft steatosis [8, 16], operation time and technique [15, 18], severity of recipient’s liver disease [8, 19], and donor age [13, 17]. One single center study retrospective analysis was unable to identify even a single risk factor in a retrospective analysis of a sample of 261 LT recipients [37]. Our findings that graft quality and hemodymic impairment prior to reperfusion are risk factors for PRS concur with several similar studies. However, it remains cryptic why the multitude of these observational studies generate such a diversity of findings when it comes to predicting postreperfusion syndrome. Prospective multi-center trials, the creation of an LT register or meta-analyses investigating the prediction of PRS could help to shed light on this matter in the future.
The increasing number of liver transplantations has led to an increased demand of donor organs [1] and to the growing use of organs from extended criteria donors (ECD) [23]. A common quality marker for organs is fatty change, or steatosis. Steatosis has indeed been linked to the occurrence of PRS [8, 16]. Studies have shown that transplantation of liver grafts with moderate to severe steatosis can very well be conducted without sacrificing recipient survival but in particular, that increased efforts are needed when dealing with these organs [26, 38]. However, macroscopic assessment of the organ may not be qualified to assess steatosis: Rey and colleagues have examined 36 livers of organ donors which were explanted but not allocated. The authors found that macroscopic appearance and coloring compared to histopathologic evaluation for steatosis unveiled discrepancies: Most of the graft livers with histopathologically confirmed mild degree of steatosis macroscopically appeared yellow, thus of false poor quality and could have been transplanted. In our analyses, microscopic steatosis evaluation was a worse predictor for PRS than the visual evaluation of the transplanting surgeon. This may be the case because surgeons likely assess the organ not only by its color, but also by general appearance, organ consistency, and size. It may even be the case that information of the recipient’s medical history and the knowledge that the organ was already rejected once by another center or had a long CIT additionally influenced the assessment. Therefore, the multitude of information may have enabled the surgeon to predict PRS better than any single variable (recipient status, CIT, steatosis, etc.).
We also found intraoperative norepinephrine infusion rate before reperfusion to be a predictor of PRS. This also concurs with other studies that have identified markers of hemodynamic instability prior to reperfusion as predictors of PRS. One possible explanation for norepinephrine infusion or hemodynamic instability is hypovolemia. This would also concur with other studies that have shown lower central venous pressure at time of dissection [14] or at time of reperfusion [17] as well as a higher requirement for transfusion units [15] to be predictors of PRS. A second possible explanation is vasodilatation or vasplegia which has been linked to end stage liver disease [39, 40]. Case reports have described vasoplegic syndrome to occur during liver transplantation [31, 41]. However, differentiation between the two can sometimes be complicated as both appear alike [34]. A third possible explanation may be that these patients already had a compromised cardiac function. E.g., Xu and colleagues could link left ventricular diastolic dysfunction to the occurrence of PRS in a cohort of 330 Chinese LT recipients [20]. Unfortunately, our data did not contain systematic and detailed cardiac function assessment of the recipients and the literature lacks systematic investigation of its impact on the occurrence of PRS. Moreover, it has been suggested by several authors that PRS could be only a sign of an underlying problem. It could be that anhepatic hypovolemia, vasoplegia and/or impaired cardiac function demask as PRS intraoperatively. On top of it, patients receiving a LT from ECD appear especially susceptible to severe PRS. In this light, these patients should especially be optimized regarding hemodynamics and acid-base balance when awaiting reperfusion.
Similar to the prediction of PRS, data on the effect of PRS on LT recipients’ outcome is inconclusive. In particular, the impact of PRS on hard clinical endpoints such as primary graft nonfunction with requirement for retransplantation and mortality is unresolved. E.g., some studies show an effect of PRS on mortality [15, 18,19,20] and others did not [13, 17]. In fact, we were not able to show a significant association of PRS with primary non-function (4.6 vs. 1.8%) and mortality (15.4% vs. 12.3%) in this study population. This is most likely due to the small sample size, again underscoring the need for multicenter registries. Regarding post-transplantation morbidity, we could demonstrate in our sample that the occurrence of PRS was associated with a higher frequency of postoperative delirium (12.3% vs. 1.8%) and major cardiovascular events (16.9% vs. 5.3%). While other studies have demonstrated early allograft dysfunction [42, 43], ICU length of stay [43] and the need for postoperative renal dysfunction [19, 20] we could not substantiate these associations in our study sample.
Conclusions
The data of this study demonstrated that both the visual assessment of the liver graft by the transplanting surgeon as well as the intraoperative recipients need for catecholamines before reperfusion of the graft were predictors for PRS at our center. Besides the known risk factors for PRS, anesthesiologists should keep these newly described risk factors in mind when preparing for reperfusion. As the impact of PRS on short- and long-term hard clinical endpoint remains inconclusive, further investigations and possibly multicenter prospective registries could ultimately resolve the impact of PRS on LT recipients’ outcome.
Abbreviations
- ALT:
-
Alanine transferase
- AST:
-
Aspartat transferase
- CIT:
-
Cold ischemia time
- ECD:
-
Extended criteria donors
- FFP:
-
Fresh frozen plasma
- INR:
-
International normalized ratio
- labMELD:
-
Laboratory Model of end stage liver disease
- LT:
-
Liver transplantation
- MAP:
-
Mean arterial pressure
- MELD:
-
Model of end stage liver disease
- min:
-
Minute(s)
- NE:
-
Norepinephrine
- OR:
-
Odds ratio
- PC:
-
Platelet concentrate
- PCC:
-
Prothrombin complex concentrate
- POD:
-
Postoperative day
- PoHT:
-
Portal hypertension
- PRS:
-
Postreperfusion syndrome
- PSC:
-
Primary biliary cirrhosis
- RBC:
-
Red blood cell concentrate
- SOP:
-
Standard operating procedure
- TEM:
-
Thrombelastometry
- US:
-
United States
- WIT:
-
Warm ischemia time
References
Tranplants by Donor Type [https://optn.transplant.hrsa.gov/data/view-data-reports/national-data/]. Accessed 10 May 2017.
Tacke F, Kroy DC, Barreiros AP, Neumann UP. Liver transplantation in Germany. Liver Transpl. 2016;22(8):1136–42.
Annual Report 2015 [http://www.eurotransplant.org/cms/mediaobject.php?file=AR_ET_20153.pdf]. Accessed 8 May 2017.
Schlitt HJ, Loss M, Scherer MN, Becker T, Jauch KW, Nashan B, Schmidt H, Settmacher U, Rogiers X, Neuhaus P, et al. Current developments in liver transplantation in Germany: MELD-based organ allocation and incentives for transplant centres. Z Gastroenterol. 2011;49(1):30–8.
Pezzati D, Ghinolfi D, De Simone P, Balzano E, Filipponi F. Strategies to optimize the use of marginal donors in liver transplantation. World J Hepatol. 2015;7(26):2636–47.
Routh D, Sharma S, Naidu CS, Rao PP, Sharma AK, Ranjan P. Comparison of outcomes in ideal donor and extended criteria donor in deceased donor liver transplant: a prospective study. Int J Surg. 2014;12(8):774–7.
Aggarwal S, Kang Y, Freeman JA, Fortunato FL, Pinsky MR. Postreperfusion syndrome: cardiovascular collapse following hepatic reperfusion during liver transplantation. Transplant Proc. 1987;19(4 Suppl 3):54–5.
Chung IS, Kim HY, Shin YH, Ko JS, Gwak MS, Sim WS, Kim GS, Lee S-K. Incidence and predictors of post-reperfusion syndrome in living donor liver transplantation. Clin Transpl. 2012;26(4):539–43.
Hilmi I, Horton CN, Planinsic RM, Sakai T, Nicolau-Raducu R, Damian D, Gligor S, Marcos A. The impact of postreperfusion syndrome on short-term patient and liver allograft outcome in patients undergoing orthotopic liver transplantation. Liver Transpl. 2008;14(4):504–8.
Lee J, Yoo YJ, Lee JM, Park YJ, Ryu HG. Sevoflurane versus Desflurane on the incidence of Postreperfusion syndrome during living donor liver transplantation: a randomized controlled trial. Transplantation. 2016;100(3):600–6.
Ryu H-G, Jung C-W, Lee H-C, Cho Y-J. Epinephrine and phenylephrine pretreatments for preventing postreperfusion syndrome during adult liver transplantation. Liver Transpl. 2012;18(12):1430–9.
Ryu HG, Jung CW, Lee CS, Lee J. Nafamostat mesilate attenuates Postreperfusion syndrome during liver transplantation. Am J Transplant. 2011;11(5):977–83.
Nanashima A, Pillay P, Crawford M, Nakasuji M, Verran DJ, Painter D. Analysis of postrevascularization syndrome after orthotopic liver transplantation: the experience of an Australian liver transplantation center. J Hepato-Biliary-Pancreat Surg. 2001;8(6):557–63.
Ayanoglu HO, Ulukaya S, Tokat Y. Causes of postreperfusion syndrome in living or cadaveric donor liver transplantations. Transplant Proc. 2003;35(4):1442–4.
Bukowicka B, Akar RA, Olszewska A, Smoter P, Krawczyk M. The occurrence of postreperfusion syndrome in orthotopic liver transplantation and its significance in terms of complications and short-term survival. Ann Transplant. 2011;16(2):26–30.
Chui AK, Shi L, Tanaka K, Rao AR, Wang LS, Bookallil M, Mayr M, Chiu E, Verran DJ, Mears D, et al. Postreperfusion syndrome in orthotopic liver transplantation. Transplant Proc. 2000;32(7):2116–7.
Fukazawa K, Yamada Y, Gologorsky E, Arheart KL, Pretto EAJ. Hemodynamic recovery following postreperfusion syndrome in liver transplantation. J Cardiothorac Vasc Anesth. 2014;28(4):1006–14.
Paugam-Burtz C, Kavafyan J, Merckx P, Dahmani S, Sommacale D, Ramsay M, Belghiti J, Mantz J. Postreperfusion syndrome during liver transplantation for cirrhosis: outcome and predictors. Liver Transpl. 2009;15(5):522–9.
Siniscalchi A, Dante A, Spedicato S, Riganello L, Zanoni A, Cimatti M, Pierucci E, Bernardi E, Miklosova Z, Moretti C, et al. Hyperdynamic circulation in acute liver failure: reperfusion syndrome and outcome following liver transplantation. Transplant Proc. 2010;42(4):1197–9.
Xu ZD, Xu HT, Yuan HB, Zhang H, Ji RH, Zou Z, Fu ZR, Shi XY. Postreperfusion syndrome during orthotopic liver transplantation: a single-center experience. Hepatobiliary Pancreat Dis Int. 2012;11(1):34–9.
DiNorcia J, Lee MK, Harlander-Locke MP, **a V, Kaldas FM, Zarrinpar A, Farmer DG, Yersiz H, Hiatt JR, Busuttil RW, et al. Damage control as a strategy to manage Postreperfusion hemodynamic instability and coagulopathy in liver transplant. JAMA Surg. 2015;150(11):1066–72.
Jeong SM. Postreperfusion syndrome during liver transplantation. Korean J Anesthesiol. 2015;68(6):527–39.
Pareja E, Cortes M, Hervas D, Mir J, Valdivieso A, Castell JV, Lahoz A. A score model for the continuous grading of early allograft dysfunction severity. Liver Transpl. 2015;21(1):38–46.
Mossdorf A, Ulmer F, Junge K, Heidenhain C, Hein M, Temizel I, Neumann UP, Schoning W, Schmeding M. Bypass during liver transplantation: anachronism or revival? Liver transplantation using a combined Venovenous/portal venous bypass-experiences with 163 liver transplants in a newly established liver transplantation program. Gastroenterol Res Pract. 2015;2015:967951.
Gorlinger K. Coagulation management during liver transplantation. Hamostaseologie. 2006;26(3 Suppl 1):S64–76.
Angele MK, Rentsch M, Hartl WH, Wittmann B, Graeb C, Jauch KW, Loehe F. Effect of graft steatosis on liver function and organ survival after liver transplantation. Am J Surg. 2008;195(2):214–20.
Adam R, Reynes M, Johann M, Morino M, Astarcioglu I, Kafetzis I, Castaing D, Bismuth H. The outcome of steatotic grafts in liver transplantation. Transplant Proc. 1991;23(1 Pt 2):1538–40.
Kamath PS, Wiesner RH, Malinchoc M, Kremers W, Therneau TM, Kosberg CL, D'Amico G, Dickson ER, Kim WR. A model to predict survival in patients with end-stage liver disease. Hepatology. 2001;33(2):464–70.
Zalunardo MP, Schlapfer M, Beck-Schimmer B, Seifert B, Spahn DR, Bettex D. Impact of cytokine release on ventricular function after hepatic reperfusion: a prospective observational echocardiographic study with tissue Doppler imaging. BMC Anesthesiol. 2015;15:107.
Nakasuji M, Bookallil MJ. Pathophysiological mechanisms of postrevascularization hyperkalemia in orthotopic liver transplantation. Anesth Analg. 2000;91(6):1351–5.
Bezinover D, Kadry Z, Uemura T, Sharghi M, Mastro AM, Sosnoski DM, Dalal P, Janicki PK. Association between plasma cyclic guanosine monophosphate levels and hemodynamic instability during liver transplantation. Liver Transpl. 2013;19(2):191–8.
Acosta F, Rodriguez MA, Sansano T, Contreras RF, Reche M, Roques V, Beltran R, Robles R, Bueno FS, Ramirez P, et al. Influence of surgical technique on postreperfusion syndrome during liver transplantation. Transplant Proc. 1999;31(6):2380–1.
Jugan E, Albaladejo P, Jayais P, Ecoffey C. The failure of venovenous bypass to prevent graft liver postreperfusion syndrome. Transplantation. 1992;54(1):81–4.
de Armas LC, Castillo YA: Is it possible to distinguish between vasoplegic syndrome and postreperfusion syndrome during liver graft reperfusion? Anesth Analg 2010, 110(3):969–970; author reply 970-961.
Cao Z, Gao Y, Tao G. Vasoplegic syndrome during liver transplantation. Anesth Analg. 2009;108(6):1941–3.
Bezinover D, Kadry Z, McCullough P, McQuillan PM, Uemura T, Welker K, Mastro AM, Janicki PK. Release of cytokines and hemodynamic instability during the reperfusion of a liver graft. Liver Transpl. 2011;17(3):324–30.
Kiseleva EA, Ushakova IA, Kim EF, Matveev GP, Biriulina N, Vabishchevich AV. To the issue of postreperfusion syndrome predictors in orthotopic liver transplantation (OLT). Anesteziol Reanimatol. 2012;2:31–5.
McCormack L, Petrowsky H, Jochum W, Mullhaupt B, Weber M, Clavien P-A. Use of severely steatotic grafts in liver transplantation: a matched case-control study. Ann Surg. 2007;246(6):940–6. discussion 946-948
Berzigotti A, Erice E, Gilabert R, Reverter E, Abraldes JG, Garcia-Pagan JC, Bosch J. Cardiovascular risk factors and systemic endothelial function in patients with cirrhosis. Am J Gastroenterol. 2013;108(1):75–82.
Wagener G, Kovalevskaya G, Minhaz M, Mattis F, Emond JC, Landry DW. Vasopressin deficiency and vasodilatory state in end-stage liver disease. J Cardiothorac Vasc Anesth. 2011;25(4):665–70.
Khosravi MB, Milani S, Ghaffaripour S, Sahmeddini A, Eghbal MH, Malek-Hosseini SA. Very high dose epinephrine for the treatment of Vasoplegic syndrome during liver transplantation. Int J Organ Transplant Med. 2013;4(1):32–4.
Reich DL, Wood RK Jr, Emre S, Bodian CA, Hossain S, Krol M, Feierman D. Association of intraoperative hypotension and pulmonary hypertension with adverse outcomes after orthotopic liver transplantation. J Cardiothorac Vasc Anesth. 2003;17(6):699–702.
Hilmi IA, Damian D, Al-Khafaji A, Sakai T, Donaldson J, Winger DG, Kellum JA. Acute kidney injury after orthotopic liver transplantation using living donor versus deceased donor grafts: a propensity score-matched analysis. Liver Transpl. 2015;21(9):1179–85.
Acknowledgements
This analysis was conducted in the course of the doctoral thesis of AR at the Medical Faculty of the RWTH Aachen, Germany.
Funding
The study did not receive external funding and was conducted on departmental funds only.
Availability of data and materials
The datasets generated and/or analysed during the current study are not publicly available due German Data Protection Laws but are available from the corresponding author on reasonable request after approval of the local ethics committee and data safety board.
Author information
Authors and Affiliations
Contributions
AR, AA, MH designed the research, AR participated in acquisition of the data, FK, AR, MH conducted data analysis. FK drafted the manuscript, AR and MH participated in writing of the manuscript, all authors interpreted the data and revised the manuscript critically for important intellectual content, approved the final version to be published and agreed to be accountable for all aspects of the work.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The local ethics committee (University Hospital RWTH Aachen, EK 291/13) approved the analysis and waived the requirement of informed consent.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Kork, F., Rimek, A., Andert, A. et al. Visual quality assessment of the liver graft by the transplanting surgeon predicts postreperfusion syndrome after liver transplantation: a retrospective cohort study. BMC Anesthesiol 18, 29 (2018). https://doi.org/10.1186/s12871-018-0493-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12871-018-0493-9