Abstract
Purpose
To report the initial institute experience in terms of dosimetric and technical aspects in stereotactic body radiation therapy (SBRT) delivered using flattening filter free (FFF) beam in patients with liver lesions.
Methods and Materials
From October 2010 to September 2011, 55 consecutive patients with 73 primary or metastatic hepatic lesions were treated with SBRT on TrueBeam using FFF beam and RapidArc technique. Clinical target volume (CTV) was defined on multi-phase CT scans, PET/CT, MRI, and 4D-CT. Dose prescription was 75 Gy in 3 fractions to planning target volume (PTV). Constraints for organs at risk were: 700 cc of liver free from the 15 Gy isodose, Dmax < 21 Gy for stomach and duodenum, Dmax < 30 Gy for heart, D0.1 cc < 18 Gy for spinal cord, V15 Gy < 35% for kidneys. The dose was downscaled in cases of not full achievement of dose constraints. Daily cone beam CT (CBCT) was performed.
Results
Forty-three patients with a single lesion, nine with two lesions and three with three lesions were treated with this protocol. Target and organs at risk objectives were met for all patients. Mean delivery time was 2.8 ± 1.0 min. Pre-treatment plan verification resulted in a Gamma Agreement Index of 98.6 ± 0.8%. Mean on-line co-registration shift of the daily CBCT to the simulation CT were: -0.08, 0.05 and -0.02 cm with standard deviations of 0.33, 0.39 and 0.55 cm in, vertical, longitudinal and lateral directions respectively.
Conclusions
SBRT for liver targets delivered by means of FFF resulted to be feasible with short beam on time.
Similar content being viewed by others
Introduction
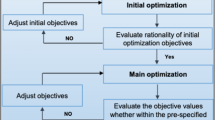
Stereotactic body radiation therapy (SBRT) has proved its efficacy in several patient populations with primary and metastatic limited tumours [Treatment delivery All plans were designed and optimised with RA technique using the optimizer PROIII for a Varian TrueBeam equipped with a Millennium multi-leaf collimator (MLC) with a leaf width of 5 mm at the isocentre. RA plans were designed using full (i.e. 360°) or partial (i.e. around 200°) multiple arcs according in order to achieve the best dose distributions. Specifically, partial arcs were used in cases of (1) lesion located far from the median axis (i.e. more than 10 cm) to do not collide the gantry with the couch induced by laterality of the couch, and (2) lesion very close to serial OARs (i.e. heart, gastro-intestinal organs) to best protect them. Where possible, coplanar arcs were employed to fasten the delivery time, otherwise, non coplanar arcs arrangements were used with two perpendicular couch positions. In particular, the non-coplanar approach was adopted in multi-lesions cases only. All dose distributions were computed with the Analytical Anisotropic Algorithm (AAA) (version 10.0.28) implemented in the Eclipse planning system with a calculation grid resolution of at maximum 2.0 mm. Treatment was delivered in 3 consecutive working days, with the patient kee** a 3-hour fast to avoid gross displacement of stomach. Treatment delivery included stereotactic frame localization in the first session aiming to a preliminary isocentre positioning followed by image guidance with on-line couch adjustment at each fraction by means of cone beam CT (CBCT). Couch repositioning was operated after automatic matching of CBCT images to reference planning CT, followed by manual refining. The shift values were analyzed for all patients and random (σ) and systematic (Σ) population errors were calculated according to Van Herk approach [30]. In two cases the delivery was performed in respiratory gated modality. This approach allows the radiation beam to be turned off when respiratory movements place the target outside of the predetermined positioning parameters, and to resume the radiation when the target falls back within the accepted alignment. In particular, the respiration path was revealed with RPM system (Varian) and internal markers, previously detected on the simulation CT. The markers were detected by instantaneous kV-portal images acquired before each beam-on phase. On each of these kV-portal images, a circular region of interest (ROI) of 5 mm radius defined the theoretical marker's position for each projection; the radiation oncologist could then verify the instantaneous marker's positions to be inside the ROI, highlighting possible internal organ motions. Before treatment, each plan was verified to assess dosimetric agreement between computed and delivered dose distributions. This quality assurance process was performed with two independent quality assurance systems (MatriXX and Gafchromic). The results of these measurements were scored in terms of the Gamma Agreement Index (GAI) based on the γ of Low analysis [31] with thresholds: Distance to Agreement = 3 mm, ΔDose = 3%. Technical parameters of delivery were scored in terms of number of arcs, total number of monitor units (MU), monitor units per Gy (MU/Gy), total beam on time, total treatment time (the time in which the patient is in the bunker), and isocenter shift. Dosimetric quality of treatments was measured on the basis of dose volume histogram (DVH) analysis. For CTV and PTV the following data were reported: target coverage (mean, D1%, D95%, V95%, V107%) and conformity for PTV. Conformity index (CI95%) was defined as the ratio between the volume of patient irradiated at 95% of the prescribed dose and the target volume. For OARs, the mean dose, the maximum dose (Dxcm3) and appropriate values of VxGy (volume receiving at least x Gy) were scored. The data were reported separately for patients with 1 lesion and with 2-3 lesions. The Kolmogorov-Smirnoff test was applied to the data to evaluate if the data were normally distributed.Data analysis and statistics
Results
Forty-three patients with a single lesion, nine with two lesions and three with three lesions were treated in this protocol, for a total of 73 isocenters. Figure 1 shows examples of dose distributions for three representative patients. Similar results were obtained in all patients. PTV and organs at risk are outlined as solid lines in the images. Table 1 reports the summary of dosimetric results.
The Kolmogorov-Smirnoff test revealed the data were normal distributed, thus the mean and standard deviation were used to present the results. In seven patients (i.e. 12% of cases) a 20% dose downscaling was necessary to comply with the liver constraint (V15 Gy free > 700 cm3). In all cases the maximum dose resulted satisfactory with negligible PTV volumes exceeding 107%. Planning objectives for organs at risk were largely met in most of the cases for both groups of patients. The always resulted > 700 cc as requested by the constraints, with mean and SD values of 965 ± 141 cc and 1283 ± 706 cc for single and multi lesion patients respectively. The higher V15 Gy free liver value for multi lesion patients was due to the larger liver volumes of this cohort of patients; the high mean and SD values are ascribable to a single case in which the total liver volume was 3320 cc (excluding the case, the mean value decreases to 1039 ± 157 cc).
Pre-treatment quality assurance measurements resulted satisfactory with a minimum deviation between groups of less than 3% and no statistically significant differences (98.7 ± 1.1% and 97.9 ± 1.1% for single and multi lesion patients respectively). In all cases GAI exceeded the acceptance threshold of 95%. Figure 2 shows an example of GAI analysis for a 2 lesions case using both Gafchromic and MatriXX.
Patients with 1 lesion were all treated with 2 full or partial arcs while patients with 2-3 lesions were treated with 2 to 6 arcs (2.7 ± 1.5). The total MUs employed were 5241 ± 1238 for single lesion plans and 7550 ± 3594 for the others, resulting in beam on time respectively of 2.3 ± 0.5 min and 3.2 ± 1.5 min, with global range of 1.9-6.2 min (this last case was a three lesion with six arcs plan). The overall treatment time, including positioning, imaging, repositioning, and delivery time, was 16.2 ± 1.7 min for the first fraction, lowering to 12.4 ± 1.5 min for the subsequent ones. Average MU/Gy resulted in the order of 200-250, slightly increasing for multi-lesion patients (≈300), confirming the intrinsic efficiency of RA technique also in terms of machine output factor.
Figure 3 shows a CBCT matching with the simulation CT for a patient with a single liver lesion. An analysis of the corrections applied by means of a daily CBCT was performed including all the 219 CBCT acquired for these patients, in order to assess any systematic error due to an inaccurate patient positioning. The mean displacements found were -0.08, 0.05 and -0.02 cm with standard deviations (SD) of 0.33, 0.39 and 0.55 cm in vertical, longitudinal and lateral directions respectively. The random (σ) and systematic (Σ) population errors, as defined in [30] were calculated with the following results: σ = 0.25-0.26-0.34 cm, Σ = 0.20-0.25-0.46 cm.
Discussion and Conclusions
The use of SBRT for the irradiation of primary and metastatic tumours in several anatomical sites is becoming a standard of treatment. SBRT has emerged as a possible non invasive approach for local ablation in some series of selected cancer patients. In particular, in abdominal sites SBRT for patients with either organ-confined primary tumours or oligo-metastatic disease may play a major role for improving survival in a clinically significant subset of cancer patients. Although in most cases the radiation sterilization of a metastatic lesion is not expected to lead to definitive cure, it could be effective in delaying further chemotherapy or at least this may contribute to better quality of life and local control.
The high dose per fraction of SBRT induces a huge amount of MU is required to cover the target and sparing the neighbour organs at risk, with a consequent increase of the beam on time with respect to the standard RT of 2 Gy/day. In this context, the recent introduction of volumetric modulated arc therapy, e.g. RapidArc, has shown to reduce the total monitor units and thus the treatment time in comparison with intensity modulated RT (IMRT) without compromising the target coverage as shown in many anatomical regions.
In this paper we considered the first 55 consecutive patients that underwent SBRT on both primary and metastatic hepatic targets, using FFF beams. In particular 43 patients presented a single lesion, 9 two lesions and 3 presented three lesions. Removal of the flattening filter gives the possibility to deliver treatments with higher dose rates, up to a factor 4 at 10 MV, and with a much higher dose per pulse. The different physical characteristics of the FFF beams (e.g. the different beam profile) are under investigation by the scientific community [18–23] and first preliminary clinical data are in progress [25].
In a previous report we analyzed a cohort of patients treated with RapidArc technique for abdominal lesions, including abdominal lymph-nodes, pancreas, and liver metastases [16]. All plans were optimized using flattened beams. In particular, comparing the results obtained for the liver metastases cohort in [16] and the data reported in this study it appears that, though for all patients 95% of the PTV volume received at least 67% of the prescription dose, more patients could receive higher mean doses to the PTV with FFF beams: mean dose to PTV was 67 Gy in [16] and around 73 Gy in the present study, PTV V95% passed from 40% to 81%, of course the higher doses to the target implies higher doses to OARs (e.g. liver V15Gy passed from 257 to 384 cc) but the constraints were always respected, the mean GAI value improved passing from 97.8% to 98.7%. On this topic, in a recent paper, we specifically compared FFF and FF beams from a dosimetric prospective, demonstrating by a theorical point of view FFF beam to be adequate in abdominal SBRT for lesions from small to medium sizes (i.e. up to 200-300 cc), with adeguate healthy tissue sparing and PTV coverage with respect to flattened beams [32]. The only significant variation between the two cohorts was the beam on time. In the previous study, where only single hepatic metastases were considered, around 9 minutes were necessary to deliver the treatment while in the present group of patients the beam on time was reduced to around 2.3 minutes (considering only the single-lesion patients), with a cut of time of more than 350%, decreasing patient's discomfort and reducing intra-fraction uncertainties. In both series the instantaneous delivery dose rate was almost always at the maximum value, 600 MU/min for FF beams and 2400 MU/min for FFF, hence the beam on time reduction. Furthermore the data reported in the present study showed that plans for with multi-lesion patients are dosimetrically comparable with the single lesion ones.
In our Institution, image-guidance by means of CBCT, implemented in the therapeutic radiation device, is daily used to better define and correct setup of each patient before each fraction of the treatment. The analysis of the daily displacements, in particular the mean values very close to 0, show the efficiency of our set-up method; however, the calculation of Σ and σ and of the relative margins, shows the absolute necessity of daily repositioning by means of CBCT; the efficiency of the set-up alone with abdominal compression and stereotactic body frame is not sufficient to apply margins of 5-8 mm in the anterior-posterior and lateral axes. Daily Image guidance has therefore allowed the minimizing of the set-up margins from CTV to PTV, reducing the normal tissue surrounding the target close to healthy organs in critical sites, such as in abdomen. At this purpose, Eccles et al. from Princess Margaret Hospital showed, in case of daily CBCT linked with abdominal compression, the maximum changes in tumour center of mass to be lower than 5 mm in 94% patients, with mean displacement of 1.4 mm, 2.1, and 1.0 mm in, respectively, LR, AP, CC directions [25].
In conclusion, we reported our practice in the treatment of liver metastases on the first 55 patients using FFF beams, prescribing 75 Gy in 3 fractions at PTV. In the majority of cases the beam on time was lower than 3 minutes, strongly reducing the treatment time in comparison with flattened filter beams, without compromising the target coverage and organs at risk sparing.
References
Timmerman RD, Kavanagh BD, Cho LC, Papiez L, **ng L: Stereotactic body radiation therapy in multiple organ sites. J Clin Oncol 2007, 25: 947-952. 10.1200/JCO.2006.09.7469
Macdermed DM, Weichselbaum RR, Salama JK: A rationale for the targeted treatment of oligometastases with radiotherapy. J Surg Oncol 2008, 98: 202-206. 10.1002/jso.21102
Schefter TE, Kavanagh BD, Timmerman RD, Cardenes HR, Baron A, Gaspar LE: A phase I trial of stereotactic body radiation therapy (SBRT) for liver metastases. Int J Radiation Oncol Biol Phys 2005, 62: 1371-1378. 10.1016/j.ijrobp.2005.01.002
Katz AW, Carey-Sampson M, Muhs AG, Milano MT, Schell MC, Okunieff P: Hypofractionated stereotactic body radiation therapy (SBRT) for limited hepatic metastases. Int J Radiation Oncology Biol Phys 2007, 67: 793-798. 10.1016/j.ijrobp.2006.10.025
Scorsetti M, Fogliata A, Castiglioni S, et al.: Early clinical experience with volumetric modulated arc therapy in head and neck cancer patients. Radiation Oncology 2010, 5: 93. 10.1186/1748-717X-5-93
Scorsetti M, Navarria P, Alongi F, et al.: Large volume unresectable locally advanced non-small cell lung cancer: acute toxicity and initial outcome results with rapid arc. Radiation Oncology 2010, 5: 94. 10.1186/1748-717X-5-94
Scorsetti M, Bignardi M, Clivio A, et al.: Volumetric modulation arc radiotherapy compared with static gantry intensity-modulated radiotherapy for malignant pleural mesothelioma tumor: a feasibility study. Int J Radiat Oncol Biol Phys 2010, 77: 942-949. 10.1016/j.ijrobp.2009.09.053
Fogliata A, Bergstrom S, Cafaro I, et al.: Cranio-spinal irradiation with volumetric modulated arc therapy: a multi-institutional treatment experience. Radiotherapy and Oncology 2011, 99: 79-85. 10.1016/j.radonc.2011.01.023
Mancosu P, Cozzi L, Fogliata A, et al.: Collimator angle influence on dose distribution optimization for vertebral metastases using volumetric modulated arc therapy. Med Phys 2010, 37: 4133-4137. 10.1118/1.3462560
Mancosu P, Navarria P, Bignardi M, et al.: Re-irradiation of metastatic spinal cord compression: a feasibility study by volumetric-modulated arc radiotherapy for in-field recurrence creating a dosimetric hole on the central canal. Radiotherapy and Oncology 2010, 94: 67-70. 10.1016/j.radonc.2009.11.010
Fogliata A, Cozzi L, Clivio A, et al.: Preclinical assessment of volumetric modulated arc therapy for total marrow irradiation. Int J Radiat Oncol Biol Phys 2011, 80: 628-636. 10.1016/j.ijrobp.2010.11.028
Mancosu P, Navarria P, Castagna L, et al.: Anatomy driven optimisation strategy for total marrow irradiation with a volumetric modulated arc therapy technique. JACMP 2011, in press.
Scorsetti M, Mancosu P, Navarria P, et al.: Stereotactic body radiation therapy (SBRT) for adrenal metastases: a feasibility study of advanced techniques with modulated photons and protons. Strahlenther Onkol 2011, 187: 238-244. 10.1007/s00066-011-2207-9
Bignardi M, Cozzi L, Fogliata A, Lattuada P, Mancosu P, Navarria P, et al.: Critical appraisal of volumetric modulated arc therapy in stereotactic body radiation therapy for metastases to abdominal lymph nodes. Int J Radiat Oncol Biol Phys 2009, 75: 1570-1577. 10.1016/j.ijrobp.2009.05.035
Bignardi M, Navarria P, Mancosu P, Cozzi L, Fogliata A, Tozzi A, et al.: Clinical outcome of hypofractionated stereotactic radiotherapy for abdominal lymph node metastases. Int J Radiati Oncol Biol Phys Vol 2010, in press.
Scorsetti M, Bignardi M, ALongi F, Fogliata A, Mancosu P, Navarria P, Castiglioni S, Pentimalli S, Tozzi A, Cozzi L: Stereotactic body radiation therapy for abdominal targets using volumetric intensity modulated arc therapy with RapidArc: feasibility and clinical preliminary results. Acta Oncol 2011,50(4):528-38. 10.3109/0284186X.2011.558522
Hrbacek J, Lang S, Klöck S: Comissioning of photon beams of a flattening filter-free linear accelerator and the accuracy of beam modelling using an anisotropic analytical algorithm. Int J Radiat Oncol Biol Phys, in press.
Vassiliev ON, Titt U, Pönisch F, Kry SF, Mohan R, Gillin MT: Dosimetric properties of photon beams from a flattening filter free clinical accelerator. Phys Med Biol 2006, 51: 1907-17. 10.1088/0031-9155/51/7/019
Kry SF, Howell RM, Titt U, Salehpour M, Mohan R, Vassiliev ON: Energy spectra, sources, and shielding considerations for neutrons generated by a flattening filter-free Clinac. Med Phys 2008,35(5):1906-11. 10.1118/1.2905029
Pönisch F, Titt U, Vassiliev ON, Kry SF, Mohan R: Properties of unflattened photon beams shaped by a multileaf collimator. Med Phys 2006,33(6):1738-46. 10.1118/1.2201149
Vassiliev ON, Titt U, Kry SF, Pönisch F, Gillin MT, Mohan R: Monte Carlo study of photon fields from a flattening filter-free clinical accelerator. Med Phys 2006,33(4):820-7. 10.1118/1.2174720
Georg D, Knöös T, McClean B: Current status and future perspective of flattening filter free photon beams. Med Phys 2011,38(3):1280-93. 10.1118/1.3554643
Kragl G, Baier F, Lutz S, Albrich D, Dalaryd M, Kroupa B, Wiezorek T, Knöös T, Georg D: Flattening filter free beams in SBRT and IMRT: dosimetric assessment of peripheral doses. Z Med Phys 2010, in press.
Vassiliev ON, Kry SF, Chang JY, Balter PA, Titt U, Mohan R: Stereotactic radiotherapy for lung cancer using a flattening filter free Clinac. J Appl Clin Med Phys 2009,10(1):2880..
Scorsetti M, Alongi F, Castiglioni S, Clivio A, Fogliata A, Lobefalo F, Mancosu P, Navarria P, Palumbo V, Pellegrini C, Pentimalli S, Reggiori G, Ascolese AM, Roggio A, Arcangeli S, Tozzi A, Vanetti E, Cozzi L: Feasibility and early clinical assessment of flattening filter free (FFF) based stereotactic body radiotherapy (SBRT) treatments. Radiat Oncol 2011, 6: 113. 10.1186/1748-717X-6-113
Eccles CL, Dawson L, Moseley JL, Brock KK: Intrafraction liver shape variability and impact on GTV position during liver stereotactic radiotherapy using abdominal compression. Int J Radiat Oncol Biol Phys 2011,80(3):938-946. 10.1016/j.ijrobp.2010.08.003
Reggiori G, Mancosu P, Tozzi A, et al.: Cone beam CT pre- and post-daily treatment for assessing geometrical and dosimetric intrafraction variability during radiotherapy of prostate cancer. J Appl Clin Med Phys 2010, 12: 3371.
RAS-trial radiofrequency ablation versus stereotactic body radiation therapy for colorectal liver metastases: a randomized trial Available at: http://www.livertumor.dk/RAS-trial.html
Milano MT, Constine LS, Okunieff P: Normal tissue toxicity after small field hypofractionated stereotactic body radiation. Radiation Oncology 2008, 3: 36. 10.1186/1748-717X-3-36
Van Herk M, Remeijer P, Rasch C, Lebesque JV: The probability of correct target dosage: dose-population histograms for deriving treatment margins in radiotherapy. Int J Radiat Oncol Biol Phys 2000,47(4):1121-35. 10.1016/S0360-3016(00)00518-6
Low DA, Harms WB, Mutic S, Purdy JA: A technique for quantitative evaluation of dose distributions. Med Phys 1998, 25: 656-661. 10.1118/1.598248
Reggiori G, Mancosu P, Castiglioni S, et al.: Can volumetric modulated arc therapy with flattening filter free beams play a role in stereotactic body radiotherapy for liver lesions? Med Phys 2012, in press.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
Dr. L. Cozzi is Head of Research at Oncology Institute of Southern Switzerland and acts as a Scientific Advisor to Varian Medical Systems. Other authors have no conflict of interest.
Authors' contributions
GR, MC, CP, SA, FL, AT, AF and LC carried out the data and participated in the data evaluation. PM, SC and GR drafted the manuscript. PM, SC and GR participated in the design of the study. FA, AF, PN and LC performed the statistical analysis. SC, FA, SA, AT, PN and MS carried out the patients record evaluation and followed patients and treatments. The definitive supervision of the paper was done by PM and MS. All authors read and approved the final manuscript.
Authors’ original submitted files for images
Below are the links to the authors’ original submitted files for images.
Rights and permissions
This article is published under license to BioMed Central Ltd. This is an Open Access article distributed under the terms of the Creative Commons Attribution License (http://creativecommons.org/licenses/by/2.0), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
About this article
Cite this article
Mancosu, P., Castiglioni, S., Reggiori, G. et al. Stereotactic body radiation therapy for liver tumours using flattening filter free beam: dosimetric and technical considerations. Radiat Oncol 7, 16 (2012). https://doi.org/10.1186/1748-717X-7-16
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/1748-717X-7-16