Abstract
China has experienced noticeable changes in climate over the past 100 years and the potential impact climate change has on transmission of mosquito-borne infectious diseases poses a risk to Chinese populations. The aims of this paper are to summarize what is known about the impact of climate change on the incidence and prevalence of malaria, dengue fever and Japanese encephalitis in China and to provide important information and direction for adaptation policy making. Fifty-five papers met the inclusion criteria for this study. Examination of these studies indicates that variability in temperature, precipitation, wind, and extreme weather events is linked to transmission of mosquito-borne diseases in some regions of China. However, study findings are inconsistent across geographical locations and this requires strengthening current evidence for timely development of adaptive options. After synthesis of available information we make several key adaptation recommendations including: improving current surveillance and monitoring systems; concentrating adaptation strategies and policies on vulnerable communities; strengthening adaptive capacity of public health systems; develo** multidisciplinary approaches sustained by an new mechanism of inter-sectional coordination; and increasing awareness and mobilization of the general public.
Similar content being viewed by others
Introduction
The Intergovernmental Panel on Climate Change (IPCC) has reported the existence of abundant evidence of climate change on a global scale [1]. According to the IPCC’s fourth assessment in 2007, global average surface temperature will increase by 1.1-6.4°C by 2100, 2-9 times more than globally averaged warming during last century [1]. Furthermore, the frequency and extent of extreme weather events; such as heat waves, bushfires, floods, and cyclones, can be highly impacted by the changing climate. Anthropogenic climate change has also been identified as an important risk factor for population health [2], including transmission of infectious diseases, and most importantly suspected impacts distribution and occurrence of vector borne diseases [1]. Despite the ongoing debate over the influence climate factors have on mosquito-borne disease occurrence, it is widely assumed that distribution and occurrence of these diseases, such as malaria, are determined by climate and that global warming trends will lead to higher incidence and wider geographic range [3–10]. In contrast, some studies hold that the current evidence is insufficient to clearly attribute local resurgences or such geographic spread to regional changes in climate [11–14]. More research is needed to better understand the relationship between climate change and transmission of mosquito-borne diseases, and to further promote adaptive policies formulation to reduce unexpected climate-related risk at a global, regional or local level.
Mosquito-borne diseases in China remain a serious public health problem. For example, 46,988 malaria cases and 18 deaths were reported in 1,097 counties in 2007 [15]. In 2002, the most serious outbreak of dengue fever occurred in Taiwan with 5,285 diagnosed cases [16]. In 2006, an outbreak of Japanese encephalitis occurred in Shanxi Province causing 19 deaths [17]. As the largest develo** country, China has experienced considerable changes in climate over during the last decade with more rapid changes in the past 50 years [18]. The annual average temperature has risen by 0.5-0.8°C, which is slightly higher than the global average level. These variation and fluctuation in weather patterns and extreme climatological phenomena (e.g. droughts, storms, floods etc.) may have a detrimental effect on frequency and distribution of mosquito-borne diseases.
In recent years, the impact of climate change on the transmission of mosquito-borne diseases has been studied in China. However, the quantitative relationship between meteorological variables and the spatial and temporal distributions of these infectious diseases is still not clear. Study findings are inconsistent, which may be due to methodological limitations, unavailability of relevant data and many uncertainties about the range and magnitude of influences of climate change. Moreover, there remains no adaptive mechanism to reduce adverse consequences of mosquito-borne diseases under the changing climate in China. It is urgent to improve our understanding of current evidence, knowledge gaps and development of adaptation options. Our aims were to summarize previous research exploring climate change-related impacts on mosquito-borne diseases in China by reviewing the published studies examining the relationship between climate variability and the transmission of malaria, dengue fever and Japanese encephalitis, and to give some suggestions for the development of adaptation strategies and measures to lessen the adverse impacts on mosquito-borne diseases in China.
Methods
Search strategy
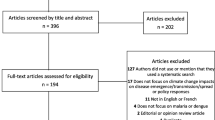
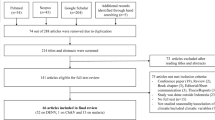
The PubMed electronic database and China Hospital Knowledge Database (CHKD) were used in December 2011 to retrieve original studies published in English and Chinese, respectively. Searches of the “Google” search engine and “Google Scholar” were also conducted. Combinations of the key terms “malaria”, “dengue”, “dengue fever”, “dengue hemorrhagic fever”, “Japanese encephalitis”, “climate”, “weather”, “climate change”, “climate variability”, “climatic factors”, “temperature”, “rainfall”, and “humidity” were used to maximize search yield. Titles, abstracts and keywords were first screened for relevance and full texts were obtained to evaluate for inclusion criteria. Reference lists of each included article were then evaluated if missed in the in the initial electronic database search. Figure 1 illustrates the systematic search and inclusion/exclusion process.
Inclusion criteria
Studies were included on the basis of the following criteria:
-
1.
Articles must evaluate the effects of climatic factors on the distribution and transmission of malaria, dengue fever or Japanese encephalitis. Meteorological variables (e.g. temperature, rainfall etc.) or ecological proxy indicators (e.g. Normalized Difference Vegetation Index, South Oscillation Index) had to be included. Disease variables (e.g. incidence, cases) or entomologic variables (e.g. Breteau Index, House Index etc.) had to be included.
-
2.
The papers had to use an epidemiological study design (e.g. time series analysis, spatial and/or temporal analysis and descriptive study) to identify the association between climatic variables and incidence of mosquito-borne diseases and/or vector factors (e.g. mosquito density, distribution, infectious life span).
-
3.
Only studies published before December 2012 and conducted in China (including Chinese Autonomous Regions, Hong Kong, Macau and Taiwan) were examined.
Results and discussion
Literature search
To avoid language bias, studies published in English and Chinese were considered for inclusion (Table 1). The initial search generated 3769 articles from PubMed, CHKD and Google Scholar databases. Review of the titles, abstracts and keywords excluded 2989 articles, leaving 780 studies identified as potential epidemiological papers. Then, 517 full-text articles were identified based on the abstracts and evaluated for inclusion. Of these, fifty-four articles met the inclusion criteria and 3 papers were included after cross-referencing. The methodologies and major findings of the final 57 studies are summarized in Tables 2, 3 and 4.
Study sites mainly included Yunnan Province (n = 9), Hainan Province (n = 8), Anhui Province (n = 7), Taiwan (n = 7), Guizhou Province (n = 5), Shandong Province (n = 3), Guangdong Province (n = 3), Henan Province (n = 2), Hubei Province (n = 2), Jiangsu Province (n = 2), and Liaoning Province (n = 2). Other locations included Jiangxi Province, Hebei Province, Shanxi Province, Shaanxi Province, Sichuan Province, Gansu Province, Zhejiang Province, Fujian Province, Bei**g Municipality, Chongqing Municipality, Tian** Municipality, Inner Mongolian Autonomous Region, and Tibetan Autonomous Region. However, there was no study conducted in some regions where mosquito-borne diseases are endemic, such as Guangxi and Hunan Province.
All included studies examined the relationship between climatic variables and mosquito-borne diseases. Of these, only 6 studies evaluated of the impacts of both meteorological factors and other relevant determinants, such as urbanization, agriculture and vaccination [51, 54, 64, 71, 73]. Several studies used ecological proxy indicators including Normalized Difference Vegetation Index (NDVI) and South Oscillation Index (SOI) as risk variables [28, 29, 35, 23, 31, 35, 19, 23, 47, 56]. Other statistical methods used included study designs utilizing Principle Component Analysis (PCA), Back propagation artificial neural network and CLIMEX model etc.
Associations between climatic variables and mosquito-borne diseases
Malaria
Despite considerable reductions in the overall burden of malaria in the 20th century, this ancient disease still represents a significant public health problem in China, especially in the southern and central regions. In 2010, 7,855 diagnosed malaria cases and 34,082 suspected cases with 19 deaths were reported in 1191 counties of 239 Provinces/Municipalities/Autonomous Regions in China. The annual incidence was 0.66/10,000 population [76]. Only sixteen percent of malaria cases were caused by Plasmodium falciparum[76] mostly occurring in Yunnan Province, which is located in southern China. Yunnan remains a hypo-endemic region with persistent cases of both P. falciparum and P. vivax malaria.
To identify risk factors related to climate change and its role in malaria transmission, a series of studies were conducted in mainland China to investigate the relationships between meteorological variables and malaria [19–46]. Except for a single study that found no association, all studies showed correlations between climatic variables and malaria in different locations and study periods in China. The contradictory study likely resulted from a short (6-month) study period [36]. In Yunnan province, two studies were conducted in 2009 to clarify potential risk factors of malaria transmission [26, 31]. Clements et al. (2009) demonstrated that for P. vivax the relative risk appeared to cycle every 3 to 4 years, whereas for P. falciparum the pattern was less regular [26]. Hui et al. (2009) found that the influence of meteorological variables on P. vivax malaria was greater than that of P. falciparum malaria, especially in cluster areas, indicating P. vivax malaria may be more climate-sensitive [31].
Almost all of these analyses identified a positive association between temperature indices and malaria transmission. Some studies also reported that temperature was the most important climatic determinant in the transmission of malaria. For example, a study conducted in **an, which is a temperate city in northern China, showed that a 1°C rise in maximum temperature may be related to a 7.7% to 12.7% increase in the number of malaria cases, while a 1°C rise in minimum temperature may result in approximately 11.8% to 12.7% increase in cases [22]. Zhou et al. (2010) revealed that temperature was a key meteorological factor correlated to malaria incidence, implying the potential role of global warming in malaria re-emergence in central China early in the 21th century, especially in Anhui, Henan and Hubei Provinces along the Huang-Huai River [21]. However, the association between temperature variables and malaria incidence may not be constant year-round. Tian et al. (2008) emphasized the stronger effect of minimum temperature on malaria incidence in the cool months in the rain forest area of Mengla County, Yunnan province, indicating increased risk of transmission as a result of warmer winters [27]. Although global warning could make more areas climatologically suitable for malarial transmission; because higher temperature promotes mosquito development, virus replication and feeding frequency of mosquitoes, extreme high temperature can also restrict the growth of mosquitoes and reduce the spread of malaria. Typically, temperatures lower than 16°C or higher than 30°C have a negative impact on the development and activities of mosquitoes [30].
High relative humidity is expected to prolong the life of the mosquito enabling it to transmit the infection to several persons. Correlations between relative humidity and malarial transmission were also detected in some regions in China [19, 20, 23–25, 30, 32, 23]. In Motou County of Tibet, Huang et al. (2011) found that relative humidity, which was greatest relative to malaria incidence among meteorological variables as it is a result of temperature, rainfall and other climatic indicators and influenced the activity of mosquito directly such as biting rate and breeding rate [20]. The distribution of mosquitoes, which also is also dependent on relative humidity, determines the extent of malarial spread. Thus, no malaria transmission occurs where the monthly average relative humidity is lower than 60% [23]. Conversely, it was reported that relative humidity is not a restricting factor in areas where it is higher than 60%, but temperature then becomes the major driver [23]. For example, no association of relative humidity and malaria transmission was detected in Hainan province [19–21, 23–26, 30–35, 94, 95], which may affect the development and infection capacity of both the mosquito and the virus. Relative humidity is also important in the transmission of JE because mosquitoes can survive longer and disperse further in areas with suitable relative humidity [96]. Studies in different areas of Asia have also shown the likely influence of climate on the incidence of JE [97–99]. However, little research has been conducted to examine the effect of climatic variables, along with mass vaccination and other non-climatic drivers in China. Bi et al. (2007) have identified positive relationships between climatic variables (monthly maximum temperature, minimum temperature and total rainfall) and JE transmission in a rural region of Anhui Province [65] and a metropolitan area of Shangdong Province [63] where no rice was grown and the role of pigs in disease transmission was not fully understood [63]. Unfortunately, the effects of vaccination on JE control in the two areas were very limited during the study periods. In the metropolitan area of **an city, a potential threshold of the effect of temperature on JE was also detected by the Hockey Stick model which is based on the assumption that temperature has no effect on JE cases until a threshold value. When the monthly mean maximum temperature was higher 25.2°C or the minimum temperature was over 21.0°C, an obvious increase in JE cases occurred [63]. These findings are consistent with the threshold temperature detection in previous Chinese studies [87]. Using ARIMA models, Lin et al. (2011) suggested that monthly average temperature and relative humidity at 0-month lag were positively associated with JE incidence in Linyi, another city of Shangdong Province after adjusting for mass vaccination in this area [62]. Time lag-0 of climate variables was perhaps because the behaviour of pig breeding in Linyi, along with the high density of mosquitoes help to shorten the transmission cycle [62]. With adjustment of more interactional factors including seasonal pattern, time trend, pig density, 23 geographic areas representing location of farm and paddy cultivation, and vaccination coverage, HSU et al. (2008) identified the significant effects of monthly temperature and rainfall with two months lag on the monthly occurrence of JE in Taiwan [64]. Similarly, temperature and rainfall were two significant determinants of JE spread with control of vaccination coverage and paddy field areas [71].
Few analyses, without controlling for non-climatic factors that potentially affect JE transmission, also reported associations between different climatic variables such as temperature, rainfall and JE annual incidence by correlation and regression analyses [66–69, 72, 100]. Based in part on recommendations and established approaches in recent studies of adaptation to climate change [81, 101–105], as well as on the status of mosquito-borne diseases in China, we highlight five principles to guide timely development of adaptation mechanism to reduce the adverse impacts of climate change on the control of mosquito-borne diseases. These guidelines may also be applicable in addressing the threat to other health outcomes from climate change.
Improving current surveillance and monitoring systems integrated with climate-sensitive conditions
In recent years, the Chinese government has paid great attention to the prevention and control of mosquito-borne diseases. Since 2004, cases of infectious diseases have been electronically recorded and the data collected at the national level by the Chinese Center for Diseases Control and Prevention (China CDC). This important step means the disease surveillance system is more sensitive and efficient than in previous years. However, unavailability of good quality long-term data sets has hampered our understanding of the likely impacts of climate change on mosquito-borne diseases and vector distribution. Kovats et al. (2001) have pointed out that climate change and health researches require at least 30 years of data because short- and medium- term associations may not provide an accurate picture of the impact of climate change occurring over many decades [106]. In China, imperfect data collected by passive surveillance systems restrict such climate-health relationship analysis. For example, onset dates rather than notification dates are not available, which may lead to considerable information bias. According to a national report in 2005, it was also estimated that only 1/18 (5.6%) malaria cases in China are reported [107]. Furthermore, lack of routine data collection of vectorial indicators has restricted our understanding of real geographic and temporal distributions of mosquito vectors.
Under the circumstance of the changing climate, truly effective surveillance systems and monitoring systems can be used to identify changes in the range and incidence of diseases; determine whether these changes are to be the result of climate change; assist the development of response measures and develop hypotheses about the climate-health relationship [108]. We believe that there are also many gaps for improving current surveillance and monitoring of infectious diseases in China in response to climate variation. Surveillance for early detection of epidemics of mosquito-borne diseases based on readily climatic data, such as daily temperature records, in combination with other interactional factors are of paramount importance [108]. For example, an effective early warning system for outbreaks of mosquito-borne diseases based on predicted extreme weather conditions, such as extreme temperature or rainfall, can be considered as an immediate opportunity for adaptation by strengthening the preparedness of emergency response before periods of high-risk [100]. Careful tracking of imported cases, in conjunction with relevant meteorological data, is also of assistance in providing earlier warning signals for emerging indigenous epidemics [109, 110]. In short, coherent surveillance systems integrated with climate-sensitive conditions are urgently needed to improve scientific knowledge about the health risks of climate change, and to prioritize needs for intervention and adaptation options.
Focusing adaptation strategies and policies on vulnerable communities
Some populations and geographical regions will be particularly vulnerable to climate change. Although climate change is a global threat to public health, it is well acknowledged that poorer nations and communities who have contributed least to greenhouse gas emissions are most vulnerable to the effects [111]. Higher malaria risk in China has also been associated with poverty, poor quality housing, unhygienic surroundings and agricultural activities in rural and remote areas. Chinese farmers in rural regions who usually work in fields and sleep in the open are at higher risk of mosquito biting especially in summer and autumn, when the peak times of malaria occurred due to favorable climate conditions and active propagation of mosquitoes. However, urban populations may also share some increased vulnerabilities in the context of climate change. For example, populations living in cities located on the coast or on small islands may be particularly vulnerable to frequent rainfall and storms and are also exposed to changes in the spread of mosquito-borne diseases, such as Taiwan. Additionally, metropolitan regions may be experiencing two types of warming trends;warmer temperatures caused by the urban heat island effect as well as global climate change, which could make more urban areas suitable for the transmission of mosquito-borne diseases by reducing development times, increasing survival probabilities and biting frequency for the mosquitoes [102, 112].
Due to limited funding, resources, and time, effective adaptive action is required to protect the most vulnerable individuals and communities, due to geographic locations and low adaptive capacity, from inevitable effects of climate change on mosquito-borne diseases. Firstly, better identification of real vulnerable groups needs to be based on more comprehensive factors, such as political rigidity, population growth, poverty, culture, dependency, geographic isolation, population immunity and human perceptions, behaviours and activities etc. This requires both qualitative and quantitative assessing methods in future adaptation research. The next step is the development and implementation of timely and efficient adaptive strategies in those targeted communities by collective coordination of all relevant sectors. Adaptive options may include expanding mosquito control, improving vaccination coverage, enhancing existing elimination programs and conducting health education programs in a relative short term, and the establishing an early warning system, improving housing quality, strengthening preparedness and response of extreme weather events (e.g. better and adequate urban drainage systems) in a long run.
Strengthening the capacity of public health system to adapt climate change
In the Chinese context, an efficient network system of mosquito-borne diseases control has been established and CDCs at national, province, and city level take the major responsibility in the network. Although the public health system has credible skills and experience ranging in disease control and prevention, public health management and emergency preparedness services, the status of the resources and capacity of mosquito-borne diseases control at local levels is not optimistic, especially in rural counties, townships and communities. For example, Chen et al. (2010) pointed out that lack of additional funding, additional staff, staff straining and equipment currently has become the major hamper of improving ability of local public health sectors in malaria surveillance, diagnosis and treatment, and mosquito control [114]. Moreover, inaccessible information and training on health influences of climate change may restrict awareness, knowledge, attitude and decisions of local public health departments. In brief, adaptation to climate change will require the public health system has a key leadership role to take in health adaptation strategy making and implementation in China. Stable funding, additional staff and better information access will be needed to best prepare the public health sectors to manage the health risks associated with climate change.
Develo** multidisciplinary approaches sustained by a new mechanism of intersectoral coordination and collaboration
What makes addressing the range and magnitude of health impacts of climate change even more difficult is unavoidable complexities and uncertainties in multi-factorial causal webs. We can not deal with climatic variables or health outcomes or any other potential interacting drivers in isolation and need to integrate scientific knowledge from various disciplines to tackle these interactions by develo** a better collaborated mechanism across all relevant governmental and non-governmental sectors and institutions which are responsible for the prevention and control of climate-sensitive disease [101, 112]. Although the existing national plans and policies about climate change clearly indicate that adaptation to health burdens from climate-sensitive diseases is a multiple-sector responsibility, mechanisms of intersectoral decision making and coordination do not yet operated to guarantee free and open exchange of information, adequate compliance and participation, ongoing financial and technological support.
For the control and prevention mosquito-borne diseases under condition of climate change, it is even more urgent to produce multidisciplinary insights from diverse public and private sectors. Although some health risks can be reduced largely by health sector interventions such as surveillance, mosquito control, spraying, vaccination, sanitation activities and health education, many adverse impacts require concerted adaptive options with other relevant sectors such as meteorology, environmental, urban designing and planning, water, agriculture and housing [101]. Unfortunately, health sectors in China which invest greater financial and resources support, are often the only ones responsible for disease prevention and control. Therefore, there is a particular need for a multidisciplinary approach sustained by ongoing intersectoral coordination and collaboration, which not only allow us to have a bettering understanding of the complex climate-health relationship, but will provide integrated and practical adaptive strategies to minimize climate-sensitive disease impairments, and further influence policy-formulation and decision-making [115, 116].
Promoting awareness and mobilization of the public and individuals
An important step in the development and promotion of successful local adaptation options is raising public and professional awareness. Governments, institutions, and organizations play indispensable roles in those adaptive actions but so do the public and individuals if they are receptive to behavior change to adapt to a world altered by climate change [101]. It is well acknowledged that the perceived risk of climate change in the population is the strongest motivator of health behaviour change, that is, it is only when individuals feel vulnerable and threatened to the impacts of climate change that they will take autonomous adaptation seriously [117]. In China, climate change has traditionally been treated as an environmental threat rather than a public health issue. We highlight that awareness programs about the health aspects of climate change are urgently needed, coupled with high-quality baseline investigations to examine public perception of adverse health effects from climate change in China.
Mobilization of the public to adapt to climate change also depends on availability of information about effective adaptation measures as well as social capacity to deal with these problems. A recent cross-sectional survey conducted in the U.S. showed that people who report knowledge of the necessary information to prepare for adverse health impacts of climate change were more likely to have an adaptive plan for their household [118]. For the prevention of mosquito-borne diseases, scientific knowledge and information, such as risk behaviour and self-protection measures, should be rapidly dispersed during high-risk periods to strengthen the adaptive capacity of the public. For example, relevant health intervention campaigns can be conducted to warn and educate local communities to change personal behaviour, e.g. use of mosquito nets in the field at peak time of mosquito-borne diseases; cleaning living conditions as soon as an increase in cases; emptying artificial containers with stagnant water timely. Moreover, better implementation of planned adaptation to climate change requires good social capability which depends on resource availability and cultural acceptability, indicating that successful adaptation strategies much be suitable for local conditions and accepted by local populations [101].
Conclusions
This study included scientific evidence of impacts of climate change on the transmission of mosquito-borne diseases, resulting in increase in incidence and geographic spread in China. Variability in temperature, precipitation, wind and extreme weather events has been observed to be linked with changes of spatial and temporal distribution of malaria, dengue fever, Japanese encephalitis in some regions in China. However, research to date has limitations and challenges in attributing changes in the status of mosquito-borne diseases to climate change. Potential adverse effects heighten the urgent need to conduct more high-quality research for assessing risks of these climate-sensitive vector-borne diseases, to improve current control policies from a weather-based direction, and to develop targeted policies for adapting short-term and long-term climate shifts in China.
Based on summarization of what is known about the likely impacts of climate change on these diseases in China we highlight five principles to guide policy formulation to enhance adaptation mechanism to reduce the adverse impacts of climate change on the control of mosquito-borne diseases. These recommendations include: 1) improving current surveillance and monitoring systems integrated with climate-sensitive conditions; 2) focusing adaptation strategies and policies on vulnerable communities; 3) strengthening public health system capacity to adapt to climate change; 4) develo** multidisciplinary approaches sustained by a new mechanism of intersectoral collaboration; and 5) promoting awareness and mobilization of the public as well as health and other professionals.
Abbreviations
- IPCC:
-
Intergovernmental Panel on Climate Change
- CHKD:
-
China Hospital Knowledge Database
- NDVI:
-
Normalized Difference Vegetation Index
- SOI:
-
South Oscillation Index
- ARIMA:
-
Autoregressive integrated moving average model
- GIS:
-
Geographic Information System
- PCA:
-
Principle Component Analysis
- P. vivax:
-
Plasmodium vivax
- P. falciparum:
-
Plasmodium falciparum
- ENSO:
-
EI Nino-Southern Oscillation
- BI:
-
Breteau Index
- HI:
-
Housing Index
- CI:
-
Container Index
- JE:
-
Japanese encephalitis
- CDC:
-
Center for Diseases Control and Prevention.
References
Climate change 2007: Impacts, Adaptation and Vulnerability. Proceedings of the Working Group II to the Fourth Assessment Report of the IPCC. Edited by: Parry ML, Canziani OF, Palutikof JP, van der Linden P, Hanson C. 2007, Cambridge: Cambridge University Press, 391-431.
McMichael AJ, Githeko AK: Climate change: Impacts, adaptation, and vulnerability. Human health. Chapter 9. Edited by: McCarthy JJ, Canziani OF, Leary NA, Dokken DJ, White KS. 2001, Cambridge: Cambridge University Press
McMichael AJ, Haines A, Slooff R, Kovats S: Climate Change and Human Health. 1996, Geneva: World Health Organization (WHO)
Impacts, Adaptations and Mitigation of Climate Change: Scientific-Technical Analyses. Proceedings of the Working Group II to the Second Assessment of the Intergovernmental Panel on Climate Change (IPCC). Edited by: Watson RT, Zinyowera MC, Moss RH. 1996, Cambridge: Cambridge University Press,
The Regional Impacts of Climate Change: An Assessment of Vulnerability. Special Report of the Intergovernmental Panel on Climate Change (IPCC) Working Group II. Edited by: Watson RT, Zinyowera MC, Moss RH. 1998, Cambridge: Cambridge University Press,
Alsop Z: Malaria returns to Kenya's highlands as temperatures rise. Lancet. 2007, 370: 925-926. 10.1016/S0140-6736(07)61428-7.
Olson SH, Gangnon R, Elguero E, Durieux L, Guegan JF, Foley JA, Patz JA: Links between climate, malaria, and wetlands in the Amazon Basin. Emerg Infect Dis. 2009, 15: 659-662. 10.3201/eid1504.080822.
Dantur Juri MJ, Zaidenberg M, Claps GL, Santana M, Almiron WR: Malaria transmission in two localities in north-western Argentina. Malar J. 2009, 8: 18-10.1186/1475-2875-8-18.
Pascual M, Ahumada JA, Chaves LF, Rodo X, Bouma M: Malaria resurgence in the East African highlands: temperature trends revisited. Proc Natl Acad Sci. 2006, 103: 5829-5834. 10.1073/pnas.0508929103.
Zhou G, Minakawa N, Githeko AK, Yan G: Association between climate variability and malaria epidemics in the East African highlands. Proc Natl Acad Sci. 2004, 101: 2375-2380. 10.1073/pnas.0308714100.
McMichael AJ, Woodruff RE, Hales S: Climate change and human health: present and future risks. Lancet. 2006, 367: 859-869. 10.1016/S0140-6736(06)68079-3.
Hay SI, Cox J, Rogers DJ, Randolph SE, Stern DI, Shanks GD, Myers MF, Snow RW: Climate change and the resurgence of malaria in the East African highlands. Nature. 2002, 415: 905-909. 10.1038/415905a.
Hay SI, Shanks GD, Stern DI, Snow RW, Randolph SE, Rogers DJ: Climate variability and malaria epidemics in the highlands of East Africa. Trends Parasitol. 2005, 21: 52-53. 10.1016/j.pt.2004.11.007.
Reiter P: Climate change and mosquito-borne disease. Environ Health Perspect. 2001, 109 (Suppl 1): 141-161.
Zhou SS, Wang Y, Fang W, Tang LH: Malaria situation in the People's Republic of China in 2007. Zhongguo Ji Sheng Chong Xue Yu Ji Sheng Chong Bing Za Zhi. 2008, 26: 401-403.
Center for Disease Control, D. o. H., Executive Yuan, Taiwan: Statistics of communicable diseases and surveillance report in Taiwan area. 2004, Taiwan: Center for Disease Control, Department of Health, Executive Yuan
Wang LH, Fu SH, Wang HY, Liang XF, Cheng JX, **g HM, Cai GL, Li XW, Ze WY, Lv XJ, Wang HQ, Zhang DL, Feng Y, Yin ZD, Sun XH, Shui TJ, Li MH, Li YX, Liang GD: Japanese encephalitis outbreak, Yuncheng, China, 2006. Emerg Infect Dis. 2007, 13 (7): 1123-1125. 10.3201/eid1307.070010.
National Development and Reform Commission 2007: China's National Climate Change Programme. 2007, Bei**g: National Development and Reform Commission, Available: http://www.ccchina.gov.cn/WebSite/CCChina/UpFile/File188.pdf
Huang F, Zhou S, Zhang S, Zhang H, Li W: Meteorological factors-based spatio-temporal map** and predicting malaria in central China. AmJTrop Med Hyg. 2011, 85: 560-567. 10.4269/ajtmh.2011.11-0156.
Huang F, Zhou S, Zhang S, Wang H, Tang L: Temporal correlation analysis between malaria and meteorological factors in Motuo County, Tibet. Malar Journal. 2011, 10: 54-10.1186/1475-2875-10-54.
Zhou SS, Huang F, Wang JJ, Zhang SS, Su YP, Tang LH: Geographical, meteorological and vectorial factors related to malaria re-emergence in Huang-Huai River of central China. Malar J. 2010, 9: 337-10.1186/1475-2875-9-337.
Zhang Y, Bi P, Hiller JE: Meteorological variables and malaria in a Chinese temperate city: a twenty-year time-series data analysis. Environ Int. 2010, 36: 439-445. 10.1016/j.envint.2010.03.005.
Yang GJ, Gao Q, Zhou SS, Malone JB, McCarroll JC, Tanner M, Vounatsou P, Bergquist R, Utzinger J, Zhou XN: Map** and predicting malaria transmission in the People's Republic of China, using integrated biology-driven and statistical models. Geospat Health. 2010, 5: 11-22.
**ao D, Long Y, Wang S, Fang L, Xu D, Wang G, Li L, Cao W, Yan Y: Spatiotemporal distribution of malaria and the association between its epidemic and climate factors in Hainan, China. Malar Journal. 2010, 9: 185-10.1186/1475-2875-9-185.
Hui FM, Xu B, Chen ZW, Cheng X, Liang L, Huang HB, Fang LQ, Yang H, Zhou HN, Yang HL, Zhou XN, Cao WC, Gong P: Spatio-temporal distribution of malaria in Yunnan Province, China. AmJTrop Med Hyg. 2009, 81: 503-509.
Clements AC, Barnett AG, Cheng ZW, Snow RW, Zhou HN: Space-time variation of malaria incidence in Yunnan province, China. Malar Journal. 2009, 8: 180-10.1186/1475-2875-8-180.
Tian L, Bi Y, Ho SC, Liu W, Liang S, Goggins WB, Chan EY, Zhou S, Sung JJ: One-year delayed effect of fog on malaria transmission: a time-series analysis in the rain forest area of Mengla County, south-west China. Malar Journal. 2008, 7: 110-10.1186/1475-2875-7-110.
Bi P, Parton KA, Tong S: El Nino-Southern Oscillation and vector-borne diseases in Anhui, China. Vector Borne Zoonotic Dis. 2005, 5: 95-100. 10.1089/vbz.2005.5.95.
Liu J, Chen XP: Relationship of remote sensing normalized differential vegetation index to Anopheles density and malaria incidence rate. Biomed Environ Sci. 2006, 19: 130-132.
Bi P, Tong S, Donald K, Parton KA, Ni J: Climatic variables and transmission of malaria: a 12-year data analysis in Shuchen County, China. Public Health Rep. 2003, 118: 65-71. 10.1016/S0033-3549(04)50218-2.
Hu H, Singhasivanon P, Salazar NP, Thimasarn K, Li X, Wu Y, Yang H, Zhu D, Supavej S, Looarecsuwan S: Factors influencing malaria endemicity in Yunnan Province, PR China (analysis of spatial pattern by GIS). Southeast Asian J Trop Med Public Health. 1998, 29: 191-200.
Liu TY, Shi M, Liu L, Zhang Y, Lou PA, Yuan FM, Shan Y: Analysis of the correlation between malaria and meteorological factors. Chin J Gen Pract. 2011, 9: 604-608.
Wu SM: Influence of meteorological factors on the incidence of malaria. Chinese and Foreign Medical Research. 2011, 9: 139-140.
Huang GQ, Zhang HX, Chen GY, Yuan FY, Pei SJ, Hu LQ, Chen JS, Lin W: Evaluation of malaria epidemic situation in Tongbai and Dabieshan Mountain Area in Hubei. Journal of Tropical Medicine. 2009, 9: 11-
Wang LP, Fang LQ, Xu X, Wang JJ, Ma JQ, Cao WC, ** SG: Study on the determinants regarding malaria epidemics in Anhui province during 2004–2006. Chin J Epidemiol. 2009, 30: 38-41.
Wen L, Shi RH, Fang LQ, Xu DZ, Li CY, Wang Y, Yuan ZQ, Zhang H: Spatial epidemiological study on malaria epidemics in Hainan Province. Chin J Epidemiol. 2008, 29: 581-585.
Su YQ, Zhang ZY, Xu DZ, ** YZ, Wang SQ, Li CX: Factors analysis on the relationship of climatic variables, NDVI, and malaria transmission in Hainan. J Prev Med Chin PLA. 2006, 24: 276-278.
Yu GW, Tang LH: Study on a grey model for evaluation of anopheles minimus density. Chin J Parasitol Parasit Dis. 2005, 23: 4-
Wen L, Xu DZ, Wang SQ, Li CX, Zhang ZY, Su YQ: Analysis on the relationship between malaria epidemics and NOAA-AVHRR NDVI in Hainan province. Zhonghua Liu **ng Bing Xue Za Zhi. 2005, 26: 263-267.
Huang SJ, Wang FC, Huang J, Feng L: Apllication of path analysis in studying climatic factors in malaria transmission. Journal of Qiannan Medical College for Nationalities. 2004, 17: 232-233.
Gao CX, **ong HY, Yi D, Chai GJ, Yang XW, Liu L: Study on meteorological factors2based neural network model of malaria. Chin J Epidemiol. 2003, 24: 9-
Wen L, Xu DZ, Wang SQ, Li CX, Zhang ZY, Su YQ: Epidemic of malaria in Hainan Province and modeling malaria incidence with meteorological parameters. Chin J D is Control Prev. 2003, 7: 520-524.
Yang GJ, Zhou XN, Malone JB, Mccarroll JC, Wang TP, Liu JX, Gao Q, Zhang XP, Hong QB, Sun LP: GIS prediction model of malaria transmission in Jiangsu province. Chin J Prev Med. 2002, 36: 2-
Huang HS: Analysis of seasonal pattern of malaria distribution in Gaoan City by circular distribution method. Modern Preventive Medicine. 2001, 28: 3-
Kan SP, Shen YZ, Zou Z, Xu FN: Studies on malaria epidemic characteristics and countermeasures in Anhui Province. Chinese Journal of Parasitic Disease Control. 1999, 12: 2-
Yu YS, Deng ZM, Huang SJ, Chu ZQ: Path analysis of climatic impacts on malaria. Chi J Health Statistics. 1995, 12: 3-
Wu F, Liu Q, Lu L, Wang J, Song X, Ren D: Distribution of Aedes albopictus (Diptera: Culicidae) in northwestern China. Vector Borne Zoonotic Dis. 2011, 11: 1181-1186. 10.1089/vbz.2010.0032.
Lai LW: Influence of environmental conditions on asynchronous outbreaks of dengue disease and increasing vector population in Kaohsiung, Taiwan. Int J Environ Health Res. 2011, 21: 133-146. 10.1080/09603123.2010.515670.
Chen SC, Liao CM, Chio CP, Chou HH, You SH, Cheng YH: Lagged temperature effect with mosquito transmission potential explains dengue variability in southern Taiwan: insights from a statistical analysis. Sci Total Enviroon. 2010, 408: 4069-4075. 10.1016/j.scitotenv.2010.05.021.
Shang CS, Fang CT, Liu CM, Wen TH, Tsai KH, King CC: The role of imported cases and favorable meteorological conditions in the onset of dengue epidemics. PLoS Negl Trop Dis. 2010, 4: e775-10.1371/journal.pntd.0000775.
Lu L, Lin H, Tian L, Yang W, Sun J, Liu Q: Time series analysis of dengue fever and weather in Guangzhou, China. BMC Publ Health. 2009, 9: 395-10.1186/1471-2458-9-395.
Hsieh YH, Chen CW: Turning points, reproduction number, and impact of climatological events for multi-wave dengue outbreaks. Trop Med Int Health. 2009, 14: 628-638. 10.1111/j.1365-3156.2009.02277.x.
Yang T, Lu L, Fu G, Zhong S, Ding G, Xu R, Zhu G, Shi N, Fan F, Liu Q: Epidemiology and vector efficiency during a dengue fever outbreak in Cixi, Zhejiang Province, China. J Vector Ecol. 2009, 34: 148-154.
Wu PC, Lay JG, Guo HR, Lin CY, Lung SC, Su HJ: Higher temperature and urbanization affect the spatial patterns of dengue fever transmission in subtropical Taiwan. Sci Total Environ. 2009, 407: 2224-2233. 10.1016/j.scitotenv.2008.11.034.
Wu PC, Guo HR, Lung SC, Lin CY, Su HJ: Weather as an effective predictor for occurrence of dengue fever in Taiwan. Acta Trop. 2007, 103: 50-57. 10.1016/j.actatropica.2007.05.014.
Lu L, Lin HL, Liu QY: Risk map for dengue fever outbreaks based on meteorological factors. Adv. Clim. Change Res. 2010, 6 (4): 254-258.
Yu SX, Li ZQ, Teng WP, Cai J: Impact on the potential epidemic of dengue fever under warming winter in Hainan province. Chin J Epidemiol. 2005, 26: 25-28.
Chen FY, Wu F, Lv ZP, He YM, Chen GX: Prediction research on dengue fever and vectors in South port of China. China J Frontier Health Quarantine. 2003, 26: 5-9.
Yi BT, Zhang ZY, Xu DZ, ** YZ, Fu JG, Luo J, Yuan MH, Liu SQ, Kuang K: Influence of climate factors on vector aedes density of dengue. Chin J Public Health. 2003, 19: 129-131.
Chen WJ, Li CX, Lin MH, Wu KS, KL W: Study on the suitable duration for dengue fever (DF) transmission in a whole year and potential impact on DF by global warming in Hainan Province. China Tropical Medicine. 2002, 2: 31-34.
Zheng NX, Wang ZH, Zhang XY, Zheng G, Chen HH, Li WZ, Chen HG, Chen MH, Lin YQ, Zhao ST: Study on seasonal trend, propagating condition and the the influencing factors of Aedes albopictus in Fuzhou, China. Strait J Prev Med. 2001, 7: 6-9.
Lin H, Yang L, Liu Q, Wang T, Hossain SR, Ho SC, Tian L: Time series analysis of Japanese encephalitis and weather in Linyi City, China. Int J Public Health. 2011, 57 (2): 289-296.
Bi P, Zhang Y, Parton KA: Weather variables and Japanese encephalitis in the metropolitan area of **an city, China. J Infect. 2007, 55: 551-556. 10.1016/j.**f.2007.07.004.
Hsu SM, Yen AM, Chen TH: The impact of climate on Japanese encephalitis. Epidemiol Infect. 2008, 136: 980-987.
Bi P, Tong S, Donald K, Parton KA, Ni J: Climate variability and transmission of Japanese encephalitis in eastern China. Vector Borne Zoonotic Dis. 2003, 3: 111-115. 10.1089/153036603768395807.
Huo AM, Zhao DS, Fang LQ, Cao WC: Association between infectious diseases with natural factors and meteorological factors in North China. Journal of Pathogen Biology. 2011, 6: 5-7.
Xu L, Yang ZZ, Ran L, Fan QJ: Multiple stepwise regression analysis of relationship between disease occurred and meteorological factors. C J G MCM. 2009, 24: 993-995.
Gao L, Li X, Lu CG, Li XY, Yang JZ, Long FX, Jiang QY: Epidemic analysis of Japanese encephalitis in Guizhou Province. Modern Preventive Medicine. 2009, 36: 4608-4609.
Liu ZY, Du AG: Grey correlation analysis of meteorological factors and Japanese encephalitis incidences. Journal of Mathematical Medicine. 2008, 22: 64-66.
Qu B, Guo HQ, Guan P, Zhou BS, Huang DS: Study on the impact of meteorological factors on Japanese encephalitis incidence. Chin J Epidemiol. 2006, 27: 179-
Zhang YZ, Potjaman S, Zhang HL, Dong XQ, Wang SD, Huang QY, Chen BY, Chen HY: Situational analysis of Japanese Encephalitis in Dali Prefecture, Yunnan Province, China from 1992 to 2001. Endemic Diseases Bull etin. 2004, 19: 31-35.
Liu YJ, Deng Z, Zhao R, Hou WM, Li LH: Correlation analysis of Japanese encephalitis incidences and meteorological factors in Chaoyang City, Liaoning Province from 1983–2002. Journal of Tropical Disease and Parasitology. 2003, 1: 188-
Shen B, Ding D, Li YT: Study on ecological factors for secular changes in incidence of Japanese Encephalitis in Shanghai. CHINA PUBLIC HEALTH. 2002, 18 (3): 308-309.
Zhang YP, Li LC, Wu ZY, Guo WS, Wang WZ, **a ZG, Zhao ZM, Que MJ: Study on geographical epidemiology of Japanese encephalitis in Henan Province. Henan Medical Research. 1997, 6: 69-73.
Feng XG, Zhang HL, Hong ZD, Li W: Epidemic investigation of Japanese encephalitis outbreaks in Eyuan County. Chinese Journal of Vector Biology and Control. 1996, 7 (5): 365-366.
Zhou SS, Wang Y, Li Y: Malaria situation in the People’s Republic of China in 2010. Chin J Parasitol Parasit Dis. Dec. 2011, 29: 6-
Gubler DJ, Reiter P, Ebi K, Yap W, Nasci R, Patz J: Climate variability and change in the United States: potential impacts on vector- and rodent-borne diseases. Environ Health Perspect. 2001, 109 (Suppl. 2): 223-233.
Qiu FX, Gubler DJ, Liu JC, Chen QQ: Dengue in China: a clinical review. Bull World Health Organ. 1993, 71: 349-359.
Jiang Y, Yan ZJ: Mechanism of dengue fever in the subtropical region of China. Chin J Vector Biol Control. 2008, 19: 80-81.
**e H, Zhou HN, Yang YM: Advances in the research on the primary dengue vector Aedes aegypti in China. Chin J Vector Biol & Control. 2011, 22: 2-
Sutherst RW: Global change and human vulnerability to vector-borne diseases. Clin Microbiol Rev. 2004, 17: 136-173. 10.1128/CMR.17.1.136-173.2004.
Hales S, de Wet N, Maindonald J, Woodward A: Potential effect of population and climate changes on global distribution of dengue fever: an empirical model. Lancet. 2002, 360: 830-834. 10.1016/S0140-6736(02)09964-6.
Nagao Y, Thavara U, Chitnumsup P, Tawatsin A, Chansang C, Campbell-Lendrum D: Climatic and social risk factors for Aedesinfestation in rural Thailand. TropMed Int Health. 2003, 8 (7): 650-659. 10.1046/j.1365-3156.2003.01075.x.
Watts DM, Burke DS, Harrison BA, Whitmire RE, Nisalak A: Effect of temperature on the vector efficiency of Aedes aegypti for dengue 2 virus. AmJTrop Med Hyg. 1987, 36 (1): 143-152.
Kay BH, Fanning ID, Mottram P: Rearing temperature influences flavivirus vector competence of mosquitoes. Med Vet Entomol. 1989, 3 (4): 415-422. 10.1111/j.1365-2915.1989.tb00249.x.
Turell MJ: Effect of environmental temperature on the vector competence of Aedes fowleri for Rift Valley fever virus. Res Virol. 1989, 140 (2): 147-154.
Li HR: Epidemic encephalitis B. Vector-Borne Infectious Diseases. Edited by: Xu ZY. 1990, Ningxia, China: Ningxia People’s Publishing House, 85-95.
Wang HY, Li YX, Liang XF, Liang GD: Japanese encephalitis in Mainland China. Jpn J Infect Dis. 2009, 62 (5): 331-336.
Wu YC: The epidemiology of Japanese encephalitis on Taiwan during 1966–1997. AmJTrop Med Hyg. 1999, 61: 78-84.
Li YX, Li MH, Fu SH, Chen WX, Liu QY, Zhang HL, Da W, Hu SL, Mu SD, Bai J, Yin ZD, Jiang HY, Guo YH, Ji DZ, Xu HM, Li G, Mu GG, Luo HM, Wang JL, Wang J, Ye XM, ** ZM, Zhang W, Ning GJ, Wang HY, Li GC, Yong J, Liang XF, Liang GD: Japanese encephalitis, Tibet, China. Emerg Infect Dis. 2011, 17: 934-936. 10.3201/eid1705.101417.
Van Den Hurk AF, Montgomery BL, Northill JA, Smith IL, Zborowski P, Ritchie SA, Mackenzie JS, Smith GA: Short report: the first isolation of Japanese encephalitis virus from mosquitoes collected from mainland Australia. AmJTrop Med Hyg. 2006, 75 (1): 21-25.
Erlanger TE, Weiss S, Keiser J, Utzinger J, Wiedenmayer K: Past, present, and future of Japanese encephalitis. Emerg Infect Dis. 2009, 15 (1): 1-7. 10.3201/eid1501.080311.
Jeffrey NH, Scott AR, Debra AP: An outbreak of Japanese encephalitis in the Torres Strait, Australia. Med J Aust. 1998, 165: 256-260.
Anyamba A, Chretien JP, Small J, Tucker CJ, Linthicum KJ: Develo** global climate anomalies suggest potential disease risks for 2006–2007. Int J Health Geogr. 2006, 5: 60-10.1186/1476-072X-5-60.
Houghton JT, Ding Y, Griggs DJ, Noguer M, Linden P, Dai X, Maskell K, Johnson CA: Climate change 2001: the scientific basis. proceeding of working group I to the third assessment report of the intergovernmental panel on climate change (IPCC). 2001, Cambridge: Cambridge University Press
Tong SL, Hu WB: Climate variation and incidence of Ross River virus in Cairns, Australia: a time-series analysis. Environ Health Perspect. 2001, 109 (12): 1271-1273. 10.1289/ehp.011091271.
Khan S, Narain K, Handigue R, Dutta P, Mahanta J, Satyanarayana K: Role of some environmental factors in modulating seasonal abundance of potential Japanese encephalitis vectors in Assam, India. Southeast Asian J Trop Med Public Health. 1996, 27: 382-391.
Sakai T, Takahashi K, Hisasue S, Horimoto M, Takizawa T: Meteorological factors involved in Japanese encephalitis virus infection in cattle. Nippon Juigaku Zasshi. 1990, 52: 121-127. 10.1292/jvms1939.52.121.
Mogi M: Relationship between number of human Japanese encephalitis cases and summer meteorological conditions in Nagasaki, Japan. AmJTrop Med Hyg. 1983, 32: 170-174.
Weaver HJ, Blashki GA, Capon AG, McMichael AJ: Climate change and Australia's healthcare system - risks, research and responses. Aust Health Rev. 2010, 34: 441-444. 10.1071/AH09829.
Füssel HM: Assessing adaptation to the health risks of climate change: what guidance can existing frameworks provide?. Int J Environ Health Res. 2008, 18: 37-63. 10.1080/09603120701358416.
Campbell-Lendrum D, Corvalán C: Climate change and develo**-country cities: implications for environmental health and equity. J Urban Health. 2007, 84 (Suppl 3): i109-i117.
Frumkin H, Hess J, Luber G, Mafilayt J, McGeehin M: Climate change: the public health response. Amer. J. Public Health. 2008, 98: 435-445. 10.2105/AJPH.2007.119362.
McMichael AJ: Global environmental change as “risk factor”: can epidemiology cope?. Am J Public Health. 2001, 91: 1172-1174. 10.2105/AJPH.91.8.1172.
Haines A: Climate change and health: strengthening the evidence base for policy. Am J Prev Med. 2008, 35: 411-413. 10.1016/j.amepre.2008.08.003.
Kovats RS, Campbell-Lendrum D, McMichael AJ, Woodward A, Cox J: Early effects of climate change: do they include changes in vector borne diseases?. Philos T Roy Soc B. 2001, 356: 1057-1068. 10.1098/rstb.2001.0894.
Zhou SS, Tang LH, Sheng HF: Malaria situation in the People's Republic of China in 2003. Chin J Parasitol and Prasit Dis. 2005, 23: 385-387.
Haines A, McMichael AJ: Climate change and health: implications for research, monitoring, and policy. BMJ. 1997, 315: 870-874. 10.1136/bmj.315.7112.870.
Anker M: Using climate to predict infectious disease outbreaks: A review. Corval C(Eds):. 2004, Geneva: World Health Organization
Shu PY, Chien LJ, Chang SF, Su CL, Kuo YC: Fever screening at airports and imported dengue. Emerg Infect Dis. 2005, 11: 460-462. 10.3201/eid1103.040420.
Patz J, Campbell-Lendrum D, Gibbs H, Woodruff R: Health impact assessment of global climate change: expanding on comparative risk assessment approaches for policy making. Annu Rev Public Health. 2008, 29: 27-39. 10.1146/annurev.publhealth.29.020907.090750.
Rosenthal JK, Sclar ED, Kinney PL, Knowlton K, Crauderueff R, Brandt-Rauf PW: Links between the built environment, climate and population health: interdisciplinary environmental change research in New York City. Ann Acad Med Singapore. 2007, 36: 834-846.
Zhang S, **ng HJ, Zhu CC: Present status of malaria control resources in China. Journal of Pathogen Biology. 2010, 5 (8): 627-629.
Maibach EW, Chadwick A, McBride D, Chunk M, Ebi K, Balbus J: Climate change and local public health in the United stateds: preparedness, programs and perceptions of local public health department directors. PLoS One. 2008, 3 (7): 1-8.
Watson RT: Turning science into policy: challenges and experiences from the science-policy interface. Philos Trans R Soc Lond B Biol Sci. 2005, 360: 471-477. 10.1098/rstb.2004.1601.
Millennium Ecosystem Assessment: Ecosystems and human well being: a framework for assessment. 2003, Washington, DC: Island Press
Ostry A, Ogborn M, Bassil KL, Takaro TK, Allen DM: Climate change and health in British Columbia: projected impacts and a proposed agenda for adaptation research and policy. Int J Environ Res Public Health. 2010, 7: 1018-1035. 10.3390/ijerph7031018.
Semenza JC, Ploubidis GB, George LA: Climate change and climate variability: personal motivation for adaptation and mitigation. Environ Health. 2011, 10: 46-10.1186/1476-069X-10-46.
Acknowledgements
This study was supported by the National Basic Research Program of China (973 Program) (Grant No. 2012CB955504).
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
The authors declare that they have no competing interests.
Authors’ contributions
LB and QL designed the study and carried out the literature search. LB and LCM reviewed included studies and wrote the paper. All authors read and approved the final manuscript.
Authors’ original submitted files for images
Below are the links to the authors’ original submitted files for images.
Rights and permissions
Open Access This article is published under license to BioMed Central Ltd. This is an Open Access article is distributed under the terms of the Creative Commons Attribution License ( https://creativecommons.org/licenses/by/2.0 ), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
About this article
Cite this article
Bai, L., Morton, L.C. & Liu, Q. Climate change and mosquito-borne diseases in China: a review. Global Health 9, 10 (2013). https://doi.org/10.1186/1744-8603-9-10
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/1744-8603-9-10