Abstract
Neuropathic pain is a common clinical condition. Current treatments are often inadequate, ineffective, or produce potentially severe adverse effects. Understanding the mechanisms that underlie the development and maintenance of neuropathic pain will be helpful in identifying new therapeutic targets and develo** effective strategies for the prevention and/or treatment of this disorder. The genesis of neuropathic pain is reliant, at least in part, on abnormal spontaneous activity within sensory neurons. Therefore, voltage-gated sodium channels, which are essential for the generation and conduction of action potentials, are potential targets for treating neuropathic pain. However, preclinical studies have shown unexpected results because most pain-associated voltage-gated channels in the dorsal root ganglion are down-regulated after peripheral nerve injury. The role of dorsal root ganglion voltage-gated channels in neuropathic pain is still unclear. In this report, we describe the expression and distribution of voltage-gated sodium channels in the dorsal root ganglion. We also review evidence regarding changes in their expression under neuropathic pain conditions and their roles in behavioral responses in a variety of neuropathic pain models. We finally discuss their potential involvement in neuropathic pain.
Similar content being viewed by others
Introduction
Neuropathic pain is a chronic condition that affects millions of people worldwide. It is characterized by pain hypersensitivity, including spontaneous ongoing or intermittent burning pain, an exaggerated response to painful stimuli, and pain in response to normally innocuous stimuli. Because the mechanisms of neuropathic pain induction and maintenance are far more complicated than previously assumed, current treatments can be ineffective or produce potentially severe adverse effects. Understanding molecular mechanisms of this disorder may allow improvement of its treatment.
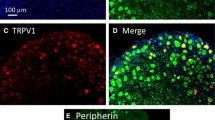
It is generally believed that neuropathic pain is caused by changes in expression and function of receptors, enzymes, and voltage-dependent ion channels in peripheral nerves and dorsal root ganglion (DRG) neurons, as well as at synapses in the nociceptive pathway in the central nervous system [1, 2]. DRG neurons express many kinds of ion channels/receptors. These channels and receptors have at least three functions (Figure 1): 1) Transduction (e.g., transient receptor potential channels, sodium channels, acid-sensing ion channels, and ATP-sensitive receptors that are expressed in the peripheral terminals of DRG neurons transduce noxious stimuli into electric impulses), 2) Conduction (e.g., sodium and potassium channels are involved in the propagation of action potentials), and 3) Modulation of synaptic transmission (e.g., voltage-gated calcium channels and glutamate receptors that are expressed on presynaptic terminals of the primary afferents in dorsal horn regulate the release of neurotransmitters). After nerve injury, injured and uninjured DRG neurons become more excitable and exhibit ectopic firing [3, 4]. It is reasonable to conclude that this abnormal spontaneous activity might be related to nerve injury-induced changes in the density, distribution, and functional activities of voltage-gated sodium channels in the DRG neurons.
Involvement of dorsal root ganglion (DRG) channels and receptors in the induction and modulation of pain. A variety of DRG channels and receptors are involved in the transduction of noxious stimuli into electric impulses at the peripheral terminals of DRG neurons [e.g., transient receptor potential (TRP) channels, voltage-sensitive sodium (Na+) channels, ATP-sensitive receptors, acid sensing ion channels], in the conduction of action potentials along the axons [e.g., voltage-sensitive Na+ channels and potassium (K+) channels], and in the modulation of neurotransmitter release at presynaptic terminals of primary afferents in the dorsal horn [e.g., voltage-gated calcium (Ca2+) channels, GABA receptors, and glutamate receptors].
To date, at least nine subtypes of sodium channel have been cloned and identified on mammalian cells. All sodium channels consist of a central α-subunit and two auxiliary β-subunits. Nine α-subunits (Nav1.1-Nav1.9, also referred to as channels) and four β-subunits have been identified in mammals. The pore-forming α-subunit determines the primary function of sodium channels, but the kinetics and voltage-dependence of channel gating are in part modified by the β-subunits. The α-subunits form four homologous domains (I-IV), each of which contains six transmembrane α helices (S1-S6) and an additional pore loop located between the S5 and S6 segments. Voltage sensors of sodium channels are located in the highly conserved S4 transmembrane segments. Membrane depolarization produces changes in the transmembrane electric field and causes the S4 segment to spiral outward. This conformational change opens the pore. Following activation, sodium channels quickly inactivate to prevent further ion flow through the pore and to allow repetitive action potential firing of cells. Most voltage-gated sodium channels can be blocked by nanomolar concentrations of tetrodotoxin (TTX) and thereby are termed TTX-sensitive channels. These TTX-sensitive channels show rapidly activating and inactivating sodium currents. In contrast, Nav1.5, Nav1.8, and Nav1.9 are relatively resistant to this toxin and show sodium currents that are TTX-resistant [5].
Voltage-gated sodium channels can be modulated by receptors coupled to intracellular signaling molecules (Figure 2). The modulation can occur through phosphorylation of specific residues on the α-subunit after the activation of cytoplasmic protein kinases. Two protein kinases, protein kinase A and protein kinase C, have been shown to target voltage-gated sodium channels. Both are activated by G-protein-coupled second messenger systems. The specific amino acid residues that are phosphorylated by these two kinases are located primarily on the linker between domains 1 and 2. The phosphorylation of voltage-gated sodium channels alters their function [6]. Moreover, the expression of voltage-gated sodium channels can be up-regulated by neurotrophins, including nerve growth factor, brain-derived neurotrophic factor (BDNF), and glial-derived neurotrophic factor (GDNF) (Figure 3) [7–9]. Interestingly, intrathecal injection of neurotrophin-3 causes significant decreases in the levels of Nav1.8 and Nav1.9 in L5 DRGs ipsilateral and contralateral to chronic constriction injury (CCI) of sciatic nerve [10]. In addition, inflammatory cytokines such as tumor necrosis factor α (TNFα) up-regulate the expression of Nav1.3, Nav1.8, and Nav1.9 and increase both TTX-sensitive and -resistant currents in the DRG neurons [11, 12]. These effects of neurotrophins and pronociceptive cytokines on sodium channel expression might be mediated through regulation of intracellular downstream signaling pathways of their receptors, including p38 and ERK1/2 mitogen-activated protein kinase (Figure 3) [11, 13].
Schematic representation of signaling pathways that modulate Na+ channels (Nav). The activation of G-protein-coupled receptors (GPCR) by their ligands activates adenylyl cyclase (AC) and phospholipase C (PLC), which produce cyclic adenosine monophosphate (cAMP) and diacylglycerol (DAG), respectively. cAMP then activates cAMP-dependent protein kinase (PKA), whereas DAG activates protein kinase C (PKC). Both PKA and PKC phosphorylate (P) the Na+ channel to regulate its function.
Potential mechanisms by which sodium channel (Nav) expression is regulated. Neurotrophins such as nerve growth factor (NGF), brain-derived neurotrophic factor (BDNF), and glial-derived neurotrophic factor (GDNF) bind to their respective receptors: tyrosine kinase receptor (Trk) A, TrkB, and Ret; receptor stimulation then activates the Ras/MEK/MAPK pathway. Activated MAPK promotes expression of sodium channels at the levels of mRNA and protein through unknown mechanisms (indicated by the red dashed arrows). An inflammatory cytokine, tumor necrosis factor α (TNFα), also up-regulates expression of sodium channels through activation of the TRAF2/MEK/MAPK pathway. In contrast, neurotrophin-3 (NT-3) down-regulates the expression of sodium channels through TrkA-mediated inhibition of the Ras/MEK/MAPK pathway (indicated by the blue dashed arrows). MAPK: mitogen-activated protein kinases; MEK: MAPK kinase; TNFR1: tumor necrosis factor receptor 1; TRAF2: TNF receptor-associated factor 2.
Most sodium channels (except for Nav1.4, which is predominantly expressed in adult skeletal muscle [14] and Nav1.5, which is expressed in cardiac tissue) have been identified in adult DRGs [15]. Their expression level and the cell types to which they are localized in the DRG are distinct under normal conditions. Unexpectedly, preclinical studies indicate that peripheral nerve injury down-regulates most pain-associated voltage-gated channels in the injured DRG. Whether and how voltage-gated channels participate in nerve injury-evoked ectopic firing in the DRG neurons is still not unclear. In this review, we describe the expression and distribution of each sodium channel subtype in the DRG. We also review evidence regarding changes that occur in channel expression under neuropathic pain conditions and their roles in behavioral responses in a variety of neuropathic pain models. Finally, we discuss their potential involvement in this disorder.
Nav1.1
Nav1.1 is a TTX-sensitive sodium channel [16, 17], but the current properties of Nav1.1 have not been characterized in DRG neurons. In situ hybridization histochemistry has shown that Nav1.1 mRNA expression in DRGs is high in large-diameter neurons, moderate in medium-diameter neurons, and low in small-diameter neurons [18, 19]. Approximately 25-33% of DRG neurons in naïve rats are positive for Nav1.1 mRNA [20]. Double immunostaining has shown that most Nav1.1-labeled cells are positive for NF200 (a marker for myelinated A-fibers), and that 79.2% of NF200-positive neurons express Nav1.1 mRNA. Research also has shown that 65.0% of Nav1.1-positive cells co-express neurotrophin-3 receptor tyrosine kinase C (TrkC; a marker for non-nociceptive mechanosensors) and that 51.6% of TrkC-labeled DRG cells are positive for Nav1.1 [21]. These findings indicate that Nav1.1 is expressed predominantly in the large-diameter A-fiber DRG neurons and that it might participate mainly in proprioceptive transmission (Table 1). It should be noted that approximately 11% of Nav1.1 mRNA-positive DRG neurons are positive for IB4 (a marker for small non-peptidergic nociceptive neurons), suggesting that Nav1.1 in these small-diameter DRG neurons may participate in nociceptive transmission and modulation [20]. Indeed, mutations in SCN1A (the gene for Nav1.1) have been associated with inherited epileptic syndromes [22] and familial hemiplegic migraine in humans [23]. Interestingly, preclinical studies showed that the level of Nav1.1 mRNA was decreased in the injured DRG after peripheral spinal nerve ligation (SNL) or spared nerve injury (SNI) [24, 25]. Thus, whether and how DRG Nav1.1 is involved in neuropathic pain development is still elusive and remains to be further studied.
Nav1.2
Nav1.2 is one of the predominant sodium channels in the central nervous system; it is localized on dendrites, unmyelinated axons, and premyelinated axons [26]. The level of Nav1.2 mRNA expression in the adult DRG is very low [18], although its expression is moderate in early developmental stages. Peripheral nerve injury and inflammation do not alter the levels of Nav1.2 mRNA or protein in the DRG [19, 24, 25]. The evidence suggests that DRG Nav1.2 is unlikely to be involved in the development of neuropathic pain (Table 1).
Nav1.3
Although Nav1.3 is expressed abundantly in DRG neurons during fetal and neonatal periods, it is normally undetectable in adult naïve DRG neurons [27]. However, it can be up-regulated in the injured DRG and ipsilateral dorsal horn after peripheral nerve injury. Approximately 37.5% of DRG neurons are Nav1.3-positive in the L5 DRG after sciatic nerve lesion and 15.8% after sural axotomy [28]. In situ hybridization histochemistry showed that, after L5 SNL, 40.7-47.2% of DRG neurons were Nav1.3 mRNA-positive cells, most of which were medium or large in size [20]. A recent study indicated that L5 ventral root transection produces a TNFα-dependent increase in Nav1.3 at both the mRNA and protein levels in the L4 and L5 DRGs [12]. Nav1.3 protein was also found to accumulate in neuromas of patients with painful neuropathy [29] and to up-regulate in second-order dorsal horn neurons after CCI [30]. These findings suggest that an increase in Nav1.3 in DRG and dorsal horn might be involved in nerve injury-induced pain hypersensitivities.
Despite the accrued evidence, the role of Nav1.3 in neuropathic pain behavior is still controversial. Hains et al. [31] reported that knockdown of DRG Nav1.3 via intrathecal administration of Nav1.3 antisense oligodeoxynucleotides (ASO) attenuated pain hypersensitivities induced by spinal cord injury and sciatic nerve CCI. In contrast, Lindia et al. [28] found that intrathecal administration of Nav1.3 ASO did not attenuate SNI-induced mechanical or cold allodynia, although it did significantly block the SNI-induced increase in DRG Nav1.3. In addition, neuropathic pain development remained intact in both conventional and conditional Nav1.3 knockout mice [32]. Furthermore, ectopic discharges from the injured nerves were unaffected in the absence of Nav1.3 in conventional knockout mice [32]. These results suggest that Nav1.3 is unlikely to be a key player in the induction of abnormal spontaneous activity in injured neurons (Table 1).
Nav1.6
Nav1.6 is predominantly located in the Nodes of Ranvier of both motor and sensory axons in the peripheral and central nervous systems [33]. In adult DRG, the cellular distribution pattern of Nav1.6 is similar to that of Nav1.1. That is, it is highly colocalized with NF200 [20], indicating that Nav1.6 is an A-fiber-specific channel (Table 1).
Nerve injury alters expression of DRG Nav1.6. Its mRNA is down-regulated in the injured L5 DRG following SNL and SNI [25]. However, in a rat model of infraorbital nerve injury, the level of Nav1.6 protein was found to be significantly increased proximal to the lesion site [34], suggesting that it might be transported quickly to the peripheral terminals under neuropathic pain conditions. Whether this increase participates in the generation of abnormal spontaneous activity in the injured DRG neurons remains to be further studied.
Nav1.7
Nav1.7 is widely expressed in sensory, sympathetic, and myenteric neurons [18, 35, 36]. In the DRG, Nav1.7 is distributed predominantly in small-diameter neurons [18, 19]. Double-labeling studies have shown that most NF200-negative neurons (>99%) express Nav1.7 mRNA [20] (Table 1). Nav1.7, as well as Nav1.6, Nav1.8, and Nav1.9, is present in most intra-epidermal free nerve endings [37], suggesting that these sodium channels are poised to participate in amplification of generator potentials, and sets the gain on nociceptors. Nav1.7 displays slow closed-state inactivation [38]. As a result of this characteristic, Nav1.7 is unable to respond during high-frequency stimulation, but it responds to small depolarizing stimuli close to the resting membrane potential [38]. Nav1.7 may be physiologically coupled to Nav1.8 within DRG neurons. It serves to boost subthreshold stimuli, resulting in the activation of Nav1.8, which recovers rapidly from inactivation and produces high-frequency action potentials [39]. The evidence indicates that Nav1.7 is expressed mainly on C- and Aδ-nociceptive fibers, contributes to amplification of generator potentials, and sets the gain on nociceptors [40, 41]. Indeed, data from animal studies have indicated that Nav1.7 plays a crucial role in nociception. Nav1.7 mRNA and protein are up-regulated in DRG after peripheral inflammation induced by carrageenan or complete Freund's adjuvant (CFA) [19, 42]. In addition, knockdown of DRG Nav1.7 significantly prevents the development of hyperalgesia in response to CFA [43]. Nav1.7 knockout mice also fail to develop hyperalgesia in several inflammatory pain models (Table 1) [44].
In humans, mutations in the SCN9A gene (which encodes Nav1.7) are associated with three known pain disorders: channelopathy-associated insensitivity to pain (CIP), paroxysmal extreme pain disorder (PEPD), and primary erythermalgia (PE) [45, 46]. Patients with CIP lose normal response to painful insults such as puncture wounds, bone fracture, biting, or contact with hot surfaces, although other sensory responses are normal [47]. PEPD is characterized by severe burning pain in the rectal, ocular, and submandibular regions, and PE by burning pain and redness of the extremities [48]. The evidence indicates that DRG Nav1.7 plays a key role in acute and inflammatory pain.
In contrast to its role in acute and inflammatory pain, whether Nav1.7 is involved in nerve injury-induced neuropathic pain is still unclear. Nav1.7 protein and current are both increased in the DRG in a rat model of painful diabetic neuropathy [49, 50], whereas the amount of Nav1.7 protein is reduced in the injured DRG after SNL, SNI, and sciatic nerve axotomy in animals [25, 51]. The level of Nav1.7 protein is also decreased in the injured DRG of humans after peripheral axotomy or traumatic central axotomy [52], but Nav1.7 protein has been observed to accumulate in painful neuromas of amputees with phantom limb pain [29, 53]. Interestingly, a mouse behavioral study showed that conditional knockout of DRG Nav1.7 did not affect SNL-induced development of mechanical allodynia [54]. Thus, it remains questionable whether DRG Nav1.7 has a role in the development of neuropathic pain.
Nav1.8
Nav1.8 is a sensory neuron-specific voltage-gated sodium channel that is expressed exclusively in small-diameter nociceptive DRG neurons [55]. Double-labeling studies have shown that 60.0% of Nav1.8-positive DRG neurons are IB4-positive [20]. Nav1.8 mRNA and protein are increased in DRG neurons of rodents following injection of carrageenan into a hind paw [19, 56, 57]. Knockdown of DRG Nav1.8 reduces the mechanical allodynia caused by intraplantar injection of CFA [58]. Furthermore, Nav1.8 knockout mice display impaired thermal and mechanical pain hypersensitivity in response to carrageenan-induced inflammation [59]. These results indicate that Nav1.8 in DRG plays a key role in inflammatory pain (Table 1).
In contrast to inflammatory insult, peripheral nerve injury down-regulates Nav1.8 mRNA and protein expression in the small-diameter neurons of the injured DRG [25, 60–62]. This down-regulation might be related to epigenetic gene silencing. Peripheral nerve injury up-regulates neuron-restrictive silence factor (NRSF) expression in the DRG and promotes NRSF binding to the neuron-restrictive silencer element within the Nav1.8 gene, thereby silencing its expression [63]. Interestingly, an increase in Nav1.8 protein was observed in the large-diameter neurons of the uninjured L4 DRG after L5 SNL [25, 64]. After L5 SNL, Nav1.8 immunoreactivity was also strikingly increased in the uninjured C-fibers of sciatic nerves [62]. Moreover, intrathecal administration of Nav1.8 ASO prevented the nerve injury-induced increase in Nav1.8 in the sciatic nerve [62]. TNFα might participate in this increase because inhibition of TNFα synthesis and knockout of TNFα strongly inhibited nerve injury-induced up-regulation of DRG Nav1.8 [12]. In patients with chronic neuropathic pain, Nav1.8 channel expression was reported to be increased in the nerves proximal to injury sites [29]. These results suggest that peripheral nerve injury might trigger TNFα-dependent translation of Nav1.8 in uninjured DRG neurons and promote the transportation of Nav1.8 from the uninjured DRG cell bodies to their axons.
The elevated Nav1.8 in uninjured DRG neurons and their axons might account, at least in part, for the abnormal spontaneous activity and behavioral tactile allodynia observed after nerve injury. Behavioral studies appear to support this conclusion. Intrathecal administration of Nav1.8 ASO attenuated nerve injury-induced mechanical and thermal hyperalgesia [62], although it failed to reduce mechanical allodynia in vincristine-induced neuropathic pain [58]. Small interfering RNAs that specifically target Nav1.8 were able to reverse mechanical allodynia in a rat CCI model when administered intrathecally [65]. Additionally, a Nav1.8 blocker, A-803467, dose-dependently attenuated mechanical allodynia in rat neuropathic pain models of SNL and sciatic nerve injury [66]. Interestingly, neuropathic pain develops normally in the Nav1.8 knockout mouse [59, 67]. Moreover, the use of diphtheria toxin to selectively delete most nociceptors (> 85%) that predominantly express Nav1.8 (as well as Nav1.7 and Nav1.9) in mouse DRG did not affect nerve injury-induced mechanical or thermal pain hypersensitivities [68]. These conflicting results indicate that the role of DRG Nav1.8 in neuropathic pain development is still uncertain and needs to be investigated further.
Nav1.9
Nav1.9 is selectively expressed in small-diameter (<30 μm) DRG neurons. Sixty-two percent of Nav1.9-positive DRG neurons are IB4-positive [20]. DRG Nav1.9 is also highly co-localized with TRPV1, purinergic P2X3 receptor, and B2 bradykinin receptor [69]. Although carrageenan injection does not alter the expression of Nav1.9 mRNA or protein in DRG [19], the level of Nav1.9 mRNA in DRG neurons is significantly increased in the CFA model [70]. Nav1.9 knockout mice exhibit blunted pain behaviors in response to formalin, carrageenan, CFA, and prostaglandin E2 [71]. Similar to Nav1.7 and Nav1.8, DRG Nav1.9 may be required for the development of inflammatory pain (Table 1).
In contrast to its involvement in inflammatory pain, DRG Nav1.9 might not contribute to the development of neuropathic pain. The levels of Nav1.9 mRNA and protein, as well as its current density, are reduced in the DRG after sciatic nerve axotomy [60, 72], SNL, and SNI [25, 61]. In addition, intrathecal administration of Nav1.9 ASO has no effect on SNL-induced neuropathic pain [64]. Intact mechanical and thermal pain hypersensitivities were observed in Nav1.9 knockout mice after SNI and partial ligation of the sciatic nerve [69, 71]. Current preclinical evidence does not support a role for DRG Nav1.9 in the development of neuropathic pain.
Conclusion
Voltage-gated sodium channels conduct sodium ion influx and control action potential generation. It has been assumed that DRG voltage-gated sodium channels participate in induction of neuropathic pain. However, as summarized in Table 1, most voltage-gated sodium channels in DRG (with the exception of Nav1.3) are down-regulated after peripheral nerve injury. This down regulation is in contrast to the increased expression that is observed under persistent inflammatory pain conditions. The mechanisms that underlie the expression changes in neuropathic pain are still unclear. As discussed above, neurotrophins (e.g., BDNF and GDNF) and cytokines modulate voltage-gated sodium channel expression (Figure 3). Up-regulation of the neurotrophic factors and the release of cytokines cannot explain the down-regulation of voltage-gated sodium channels in the DRG under neuropathic pain conditions [73, 74]. More importantly, most behavioral findings from animal models do not support a role for DRG voltage-gated sodium channels in neuropathic pain (Table 1). Interestingly, the use of sodium channel blockers (such as lidocaine) in patients can effectively inhibit a variety of neuropathic pain syndromes [75], although they also produce significant side effects. Inconsistent results between clinical and laboratory observations necessitate careful consideration of the differences between human and animal models and the methods for pain assessment. Therefore, a possible role for DRG voltage-gated sodium channel function in neuropathic pain cannot be excluded and remains to be further investigated.
References
Scholz J, Woolf CJ: The neuropathic pain triad: neurons, immune cells and glia. Nat Neurosci 2007, 10: 1361–1368. 10.1038/nn1992
Reichling DB, Levine JD: Critical role of nociceptor plasticity in chronic pain. Trends Neurosci 2009, 32: 611–618. 10.1016/j.tins.2009.07.007
Devor M: Ectopic discharge in Abeta afferents as a source of neuropathic pain. Exp Brain Res 2009, 196: 115–128. 10.1007/s00221-009-1724-6
Wu G, Ringkamp M, Hartke TV, Murinson BB, Campbell JN, Griffin JW, Meyer RA: Early onset of spontaneous activity in uninjured C-fiber nociceptors after injury to neighboring nerve fibers. J Neurosci 2001, 21: RC140.
Roy ML, Narahashi T: Differential properties of tetrodotoxin-sensitive and tetrodotoxin-resistant sodium channels in rat dorsal root ganglion neurons. J Neurosci 1992, 12: 2104–2111.
Gold MS, Levine JD, Correa AM: Modulation of TTX-R INa by PKC and PKA and their role in PGE2-induced sensitization of rat sensory neurons in vitro. J Neurosci 1998, 18: 10345–10355.
Fjell J, Cummins TR, Dib-Hajj SD, Fried K, Black JA, Waxman SG: Differential role of GDNF and NGF in the maintenance of two TTX-resistant sodium channels in adult DRG neurons. Brain Res Mol Brain Res 1999, 67: 267–282. 10.1016/S0169-328X(99)00070-4
Kafitz KW, Rose CR, Thoenen H, Konnerth A: Neurotrophin-evoked rapid excitation through TrkB receptors. Nature 1999, 401: 918–921. 10.1038/44847
Cummins TR, Black JA, Dib-Hajj SD, Waxman SG: Glial-derived neurotrophic factor upregulates expression of functional SNS and NaN sodium channels and their currents in axotomized dorsal root ganglion neurons. J Neurosci 2000, 20: 8754–8761.
Wilson-Gerwing TD, Stucky CL, McComb GW, Verge VM: Neurotrophin-3 significantly reduces sodium channel expression linked to neuropathic pain states. Exp Neurol 2008, 213: 303–314. 10.1016/j.expneurol.2008.06.002
** X, Gereau RWt: Acute p38-mediated modulation of tetrodotoxin-resistant sodium channels in mouse sensory neurons by tumor necrosis factor-alpha. J Neurosci 2006, 26: 246–255. 10.1523/JNEUROSCI.3858-05.2006
He XH, Zang Y, Chen X, Pang RP, Xu JT, Zhou X, Wei XH, Li YY, **n WJ, Qin ZH, Liu XG: TNF-alpha contributes to up-regulation of Nav1.3 and Nav1.8 in DRG neurons following motor fiber injury. Pain 2010, 151: 266–279. 10.1016/j.pain.2010.06.005
Stamboulian S, Choi JS, Ahn HS, Chang YW, Tyrrell L, Black JA, Waxman SG, Dib-Hajj SD: ERK1/2 mitogen-activated protein kinase phosphorylates sodium channel Na(v)1.7 and alters its gating properties. J Neurosci 2010, 30: 1637–1647. 10.1523/JNEUROSCI.4872-09.2010
Trimmer JS, Cooperman SS, Tomiko SA, Zhou JY, Crean SM, Boyle MB, Kallen RG, Sheng ZH, Barchi RL, Sigworth FJ, et al.: Primary structure and functional expression of a mammalian skeletal muscle sodium channel. Neuron 1989, 3: 33–49. 10.1016/0896-6273(89)90113-X
Devor M: Sodium channels and mechanisms of neuropathic pain. J Pain 2006, 7: S3-S12. 10.1016/j.jpain.2005.09.006
Smith RD, Goldin AL: Functional analysis of the rat I sodium channel in xenopus oocytes. J Neurosci 1998, 18: 811–820.
Lossin C, Wang DW, Rhodes TH, Vanoye CG, George AL Jr: Molecular basis of an inherited epilepsy. Neuron 2002, 34: 877–884. 10.1016/S0896-6273(02)00714-6
Black JA, Dib-Hajj S, McNabola K, Jeste S, Rizzo MA, Kocsis JD, Waxman SG: Spinal sensory neurons express multiple sodium channel alpha-subunit mRNAs. Brain Res Mol Brain Res 1996, 43: 117–131. 10.1016/S0169-328X(96)00163-5
Black JA, Liu S, Tanaka M, Cummins TR, Waxman SG: Changes in the expression of tetrodotoxin-sensitive sodium channels within dorsal root ganglia neurons in inflammatory pain. Pain 2004, 108: 237–247. 10.1016/j.pain.2003.12.035
Fukuoka T, Kobayashi K, Yamanaka H, Obata K, Dai Y, Noguchi K: Comparative study of the distribution of the alpha-subunits of voltage-gated sodium channels in normal and axotomized rat dorsal root ganglion neurons. J Comp Neurol 2008, 510: 188–206. 10.1002/cne.21786
McMahon SB, Armanini MP, Ling LH, Phillips HS: Expression and coexpression of Trk receptors in subpopulations of adult primary sensory neurons projecting to identified peripheral targets. Neuron 1994, 12: 1161–1171. 10.1016/0896-6273(94)90323-9
Ragsdale DS: How do mutant Nav1.1 sodium channels cause epilepsy? Brain Res Rev 2008, 58: 149–159. 10.1016/j.brainresrev.2008.01.003
Dichgans M, Freilinger T, Eckstein G, Babini E, Lorenz-Depiereux B, Biskup S, Ferrari MD, Herzog J, van den Maagdenberg AM, Pusch M, Strom TM: Mutation in the neuronal voltage-gated sodium channel SCN1A in familial hemiplegic migraine. Lancet 2005, 366: 371–377. 10.1016/S0140-6736(05)66786-4
Kim CH, Oh Y, Chung JM, Chung K: The changes in expression of three subtypes of TTX sensitive sodium channels in sensory neurons after spinal nerve ligation. Brain Res Mol Brain Res 2001, 95: 153–161. 10.1016/S0169-328X(01)00226-1
Berta T, Poirot O, Pertin M, Ji RR, Kellenberger S, Decosterd I: Transcriptional and functional profiles of voltage-gated Na(+) channels in injured and non-injured DRG neurons in the SNI model of neuropathic pain. Mol Cell Neurosci 2008, 37: 196–208. 10.1016/j.mcn.2007.09.007
Trimmer JS, Rhodes KJ: Localization of voltage-gated ion channels in mammalian brain. Annu Rev Physiol 2004, 66: 477–519. 10.1146/annurev.physiol.66.032102.113328
Waxman SG, Kocsis JD, Black JA: Type III sodium channel mRNA is expressed in embryonic but not adult spinal sensory neurons, and is reexpressed following axotomy. J Neurophysiol 1994, 72: 466–470.
Lindia JA, Kohler MG, Martin WJ, Abbadie C: Relationship between sodium channel NaV1.3 expression and neuropathic pain behavior in rats. Pain 2005, 117: 145–153. 10.1016/j.pain.2005.05.027
Black JA, Nikolajsen L, Kroner K, Jensen TS, Waxman SG: Multiple sodium channel isoforms and mitogen-activated protein kinases are present in painful human neuromas. Ann Neurol 2008, 64: 644–653. 10.1002/ana.21527
Hains BC, Saab CY, Klein JP, Craner MJ, Waxman SG: Altered sodium channel expression in second-order spinal sensory neurons contributes to pain after peripheral nerve injury. J Neurosci 2004, 24: 4832–4839. 10.1523/JNEUROSCI.0300-04.2004
Hains BC, Klein JP, Saab CY, Craner MJ, Black JA, Waxman SG: Upregulation of sodium channel Nav1.3 and functional involvement in neuronal hyperexcitability associated with central neuropathic pain after spinal cord injury. J Neurosci 2003, 23: 8881–8892.
Nassar MA, Baker MD, Levato A, Ingram R, Mallucci G, McMahon SB, Wood JN: Nerve injury induces robust allodynia and ectopic discharges in Nav1.3 null mutant mice. Mol Pain 2006, 2: 33. 10.1186/1744-8069-2-33
Caldwell JH, Schaller KL, Lasher RS, Peles E, Levinson SR: Sodium channel Na(v)1.6 is localized at nodes of ranvier, dendrites, and synapses. Proc Natl Acad Sci USA 2000, 97: 5616–5620. 10.1073/pnas.090034797
Henry MA, Freking AR, Johnson LR, Levinson SR: Sodium channel Nav1.6 accumulates at the site of infraorbital nerve injury. BMC Neurosci 2007, 8: 56. 10.1186/1471-2202-8-56
Sage D, Salin P, Alcaraz G, Castets F, Giraud P, Crest M, Mazet B, Clerc N: Na(v)1.7 and Na(v)1.3 are the only tetrodotoxin-sensitive sodium channels expressed by the adult guinea pig enteric nervous system. J Comp Neurol 2007, 504: 363–378. 10.1002/cne.21450
Toledo-Aral JJ, Moss BL, He ZJ, Koszowski AG, Whisenand T, Levinson SR, Wolf JJ, Silos-Santiago I, Halegoua S, Mandel G: Identification of PN1, a predominant voltage-dependent sodium channel expressed principally in peripheral neurons. Proc Natl Acad Sci USA 1997, 94: 1527–1532. 10.1073/pnas.94.4.1527
Persson AK, Black JA, Gasser A, Cheng X, Fischer TZ, Waxman SG: Sodium-calcium exchanger and multiple sodium channel isoforms in intra-epidermal nerve terminals. Mol Pain 2010, 6: 84.
Cummins TR, Howe JR, Waxman SG: Slow closed-state inactivation: a novel mechanism underlying ramp currents in cells expressing the hNE/PN1 sodium channel. J Neurosci 1998, 18: 9607–9619.
Rush AM, Cummins TR, Waxman SG: Multiple sodium channels and their roles in electrogenesis within dorsal root ganglion neurons. J Physiol 2007, 579: 1–14. 10.1113/jphysiol.2006.121483
Djouhri L, Newton R, Levinson SR, Berry CM, Carruthers B, Lawson SN: Sensory and electrophysiological properties of guinea-pig sensory neurones expressing Nav 1.7 (PN1) Na+ channel alpha subunit protein. J Physiol 2003, 546: 565–576. 10.1113/jphysiol.2002.026559
Waxman SG: Neurobiology: a channel sets the gain on pain. Nature 2006, 444: 831–832. 10.1038/444831a
Strickland IT, Martindale JC, Woodhams PL, Reeve AJ, Chessell IP, McQueen DS: Changes in the expression of NaV1.7, NaV1.8 and NaV1.9 in a distinct population of dorsal root ganglia innervating the rat knee joint in a model of chronic inflammatory joint pain. Eur J Pain 2008, 12: 564–572. 10.1016/j.ejpain.2007.09.001
Yeomans DC, Levinson SR, Peters MC, Koszowski AG, Tzabazis AZ, Gilly WF, Wilson SP: Decrease in inflammatory hyperalgesia by herpes vector-mediated knockdown of Nav1.7 sodium channels in primary afferents. Hum Gene Ther 2005, 16: 271–277. 10.1089/hum.2005.16.271
Nassar MA, Stirling LC, Forlani G, Baker MD, Matthews EA, Dickenson AH, Wood JN: Nociceptor-specific gene deletion reveals a major role for Nav1.7 (PN1) in acute and inflammatory pain. Proc Natl Acad Sci USA 2004, 101: 12706–12711. 10.1073/pnas.0404915101
Dib-Hajj SD, Rush AM, Cummins TR, Hisama FM, Novella S, Tyrrell L, Marshall L, Waxman SG: Gain-of-function mutation in Nav1.7 in familial erythromelalgia induces bursting of sensory neurons. Brain 2005, 128: 1847–1854. 10.1093/brain/awh514
Lee MJ, Yu HS, Hsieh ST, Stephenson DA, Lu CJ, Yang CC: Characterization of a familial case with primary erythromelalgia from Taiwan. J Neurol 2007, 254: 210–214. 10.1007/s00415-006-0328-3
Cox JJ, Reimann F, Nicholas AK, Thornton G, Roberts E, Springell K, Karbani G, Jafri H, Mannan J, Raashid Y, Al-Gazali L, Hamamy H, Valente EM, Gorman S, Williams R, McHale DP, Wood JN, Gribble FM, Woods CG: An SCN9A channelopathy causes congenital inability to experience pain. Nature 2006, 444: 894–898. 10.1038/nature05413
Waxman SG, Dib-Hajj SD: Erythromelalgia: a hereditary pain syndrome enters the molecular era. Ann Neurol 2005, 57: 785–788. 10.1002/ana.20511
Hong S, Morrow TJ, Paulson PE, Isom LL, Wiley JW: Early painful diabetic neuropathy is associated with differential changes in tetrodotoxin-sensitive and -resistant sodium channels in dorsal root ganglion neurons in the rat. J Biol Chem 2004, 279: 29341–29350. 10.1074/jbc.M404167200
Chattopadhyay M, Mata M, Fink DJ: Continuous delta-opioid receptor activation reduces neuronal voltage-gated sodium channel (NaV1.7) levels through activation of protein kinase C in painful diabetic neuropathy. J Neurosci 2008, 28: 6652–6658. 10.1523/JNEUROSCI.5530-07.2008
Kim CH, Oh Y, Chung JM, Chung K: Changes in three subtypes of tetrodotoxin sensitive sodium channel expression in the axotomized dorsal root ganglion in the rat. Neurosci Lett 2002, 323: 125–128. 10.1016/S0304-3940(02)00127-1
Coward K, Aitken A, Powell A, Plumpton C, Birch R, Tate S, Bountra C, Anand P: Plasticity of TTX-sensitive sodium channels PN1 and brain III in injured human nerves. Neuroreport 2001, 12: 495–500. 10.1097/00001756-200103050-00014
Bird EV, Robinson PP, Boissonade FM: Na(v)1.7 sodium channel expression in human lingual nerve neuromas. Arch Oral Biol 2007, 52: 494–502. 10.1016/j.archoralbio.2006.11.011
Nassar MA, Levato A, Stirling LC, Wood JN: Neuropathic pain develops normally in mice lacking both Na(v)1.7 and Na(v)1.8. Mol Pain 2005, 1: 24. 10.1186/1744-8069-1-24
Djouhri L, Fang X, Okuse K, Wood JN, Berry CM, Lawson SN: The TTX-resistant sodium channel Nav1.8 (SNS/PN3): expression and correlation with membrane properties in rat nociceptive primary afferent neurons. J Physiol 2003, 550: 739–752. 10.1113/jphysiol.2003.042127
Okuse K, Chaplan SR, McMahon SB, Luo ZD, Calcutt NA, Scott BP, Akopian AN, Wood JN: Regulation of expression of the sensory neuron-specific sodium channel SNS in inflammatory and neuropathic pain. Mol Cell Neurosci 1997, 10: 196–207. 10.1006/mcne.1997.0657
Coggeshall RE, Tate S, Carlton SM: Differential expression of tetrodotoxin-resistant sodium channels Nav1.8 and Nav1.9 in normal and inflamed rats. Neurosci Lett 2004, 355: 45–48. 10.1016/j.neulet.2003.10.023
Joshi SK, Mikusa JP, Hernandez G, Baker S, Shieh CC, Neelands T, Zhang XF, Niforatos W, Kage K, Han P, Krafte D, Faltynek C, Sullivan JP, Jarvis MF, Honore P: Involvement of the TTX-resistant sodium channel Nav 1.8 in inflammatory and neuropathic, but not post-operative, pain states. Pain 2006, 123: 75–82. 10.1016/j.pain.2006.02.011
Akopian AN, Souslova V, England S, Okuse K, Ogata N, Ure J, Smith A, Kerr BJ, McMahon SB, Boyce S, Hill R, Stanfa LC, Dickenson AH, Wood JN: The tetrodotoxin-resistant sodium channel SNS has a specialized function in pain pathways. Nat Neurosci 1999, 2: 541–548. 10.1038/9195
Cummins TR, Waxman SG: Downregulation of tetrodotoxin-resistant sodium currents and upregulation of a rapidly repriming tetrodotoxin-sensitive sodium current in small spinal sensory neurons after nerve injury. J Neurosci 1997, 17: 3503–3514.
Decosterd I, Ji RR, Abdi S, Tate S, Woolf CJ: The pattern of expression of the voltage-gated sodium channels Na(v)1.8 and Na(v)1.9 does not change in uninjured primary sensory neurons in experimental neuropathic pain models. Pain 2002, 96: 269–277. 10.1016/S0304-3959(01)00456-0
Gold MS, Weinreich D, Kim CS, Wang R, Treanor J, Porreca F, Lai J: Redistribution of Na(V)1.8 in uninjured axons enables neuropathic pain. J Neurosci 2003, 23: 158–166.
Uchida H, Ma L, Ueda H: Epigenetic gene silencing underlies C-fiber dysfunctions in neuropathic pain. J Neurosci 2010, 30: 4806–4814. 10.1523/JNEUROSCI.5541-09.2010
Porreca F, Lai J, Bian D, Wegert S, Ossipov MH, Eglen RM, Kassotakis L, Novakovic S, Rabert DK, Sangameswaran L, Hunter JC: A comparison of the potential role of the tetrodotoxin-insensitive sodium channels, PN3/SNS and NaN/SNS2, in rat models of chronic pain. Proc Natl Acad Sci USA 1999, 96: 7640–7644. 10.1073/pnas.96.14.7640
Dong XW, Goregoaker S, Engler H, Zhou X, Mark L, Crona J, Terry R, Hunter J, Priestley T: Small interfering RNA-mediated selective knockdown of Na(V)1.8 tetrodotoxin-resistant sodium channel reverses mechanical allodynia in neuropathic rats. Neuroscience 2007, 146: 812–821. 10.1016/j.neuroscience.2007.01.054
Jarvis MF, Honore P, Shieh CC, Chapman M, Joshi S, Zhang XF, Kort M, Carroll W, Marron B, Atkinson R, Thomas J, Liu D, Krambis M, Liu Y, McGaraughty S, Chu K, Roeloffs R, Zhong C, Mikusa JP, Hernandez G, Gauvin D, Wade C, Zhu C, Pai M, Scanio M, Shi L, Drizin I, Gregg R, Matulenko M, Hakeem A, Gross M, Johnson M, Marsh K, Wagoner PK, Sullivan JP, Faltynek CR, Krafte DS: A-803467, a potent and selective Nav1.8 sodium channel blocker, attenuates neuropathic and inflammatory pain in the rat. Proc Natl Acad Sci USA 2007, 104: 8520–8525. 10.1073/pnas.0611364104
Kerr BJ, Souslova V, McMahon SB, Wood JN: A role for the TTX-resistant sodium channel Nav 1.8 in NGF-induced hyperalgesia, but not neuropathic pain. Neuroreport 2001, 12: 3077–3080. 10.1097/00001756-200110080-00019
Abrahamsen B, Zhao J, Asante CO, Cendan CM, Marsh S, Martinez-Barbera JP, Nassar MA, Dickenson AH, Wood JN: The cell and molecular basis of mechanical, cold, and inflammatory pain. Science 2008, 321: 702–705. 10.1126/science.1156916
Amaya F, Wang H, Costigan M, Allchorne AJ, Hatcher JP, Egerton J, Stean T, Morisset V, Grose D, Gunthorpe MJ, Chessell IP, Tate S, Green PJ, Woolf CJ: The voltage-gated sodium channel Na(v)1.9 is an effector of peripheral inflammatory pain hypersensitivity. J Neurosci 2006, 26: 12852–12860. 10.1523/JNEUROSCI.4015-06.2006
Tate S, Benn S, Hick C, Trezise D, John V, Mannion RJ, Costigan M, Plumpton C, Grose D, Gladwell Z, Kendall G, Dale K, Bountra C, Woolf CJ: Two sodium channels contribute to the TTX-R sodium current in primary sensory neurons. Nat Neurosci 1998, 1: 653–655. 10.1038/3652
Priest BT, Murphy BA, Lindia JA, Diaz C, Abbadie C, Ritter AM, Liberator P, Iyer LM, Kash SF, Kohler MG, Kaczorowski GJ, MacIntyre DE, Martin WJ: Contribution of the tetrodotoxin-resistant voltage-gated sodium channel NaV1.9 to sensory transmission and nociceptive behavior. Proc Natl Acad Sci USA 2005, 102: 9382–9387. 10.1073/pnas.0501549102
Dib-Hajj SD, Tyrrell L, Black JA, Waxman SG: NaN, a novel voltage-gated Na channel, is expressed preferentially in peripheral sensory neurons and down-regulated after axotomy. Proc Natl Acad Sci USA 1998, 95: 8963–8968. 10.1073/pnas.95.15.8963
Vivoli E, Di Cesare Mannelli L, Salvicchi A, Bartolini A, Koverech A, Nicolai R, Benatti P, Ghelardini C: Acetyl-L-carnitine increases artemin level and prevents neurotrophic factor alterations during neuropathy. Neuroscience 2010, 167: 1168–1174. 10.1016/j.neuroscience.2010.03.017
Vanelderen P, Rouwette T, Kozicz T, Roubos E, Van Zundert J, Heylen R, Vissers K: The role of brain-derived neurotrophic factor in different animal models of neuropathic pain. Eur J Pain 2010, 14: e471–479. 473 10.1016/j.ejpain.2009.09.006
Priest BT, Kaczorowski GJ: Blocking sodium channels to treat neuropathic pain. Expert Opin Ther Targets 2007, 11: 291–306. 10.1517/14728222.11.3.291
Acknowledgements
This work was supported by the Blaustein Pain Research Fund, Mr. David Koch and the Patrick C. Walsh Prostate Cancer Research Fund, and the Brain Science Institute at the Johns Hopkins University; NIH Grant NS 058886; the National Natural Science Foundation of China (30771133, 30971123, 31010103909); the National Program of Basic Research of China (G2006CB500808); and the Innovation Research Team Program of Ministry of Education of China (31010103909). The authors thank Claire F. Levine, MS, for her editorial assistance.
Author information
Authors and Affiliations
Corresponding authors
Additional information
Competing interests
The authors declare that they have no competing interests.
Authors' contributions
WW and YXT participated in the drafted manuscript. JG, YQL, and YXT contributed to critical review of the manuscript. All authors have read and approved the final manuscript.
Authors’ original submitted files for images
Below are the links to the authors’ original submitted files for images.
Rights and permissions
Open Access This article is published under license to BioMed Central Ltd. This is an Open Access article is distributed under the terms of the Creative Commons Attribution License ( https://creativecommons.org/licenses/by/2.0 ), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
About this article
Cite this article
Wang, W., Gu, J., Li, YQ. et al. Are voltage-gated sodium channels on the dorsal root ganglion involved in the development of neuropathic pain?. Mol Pain 7, 16 (2011). https://doi.org/10.1186/1744-8069-7-16
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/1744-8069-7-16