Abstract
Background
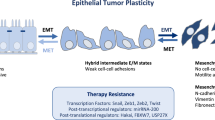
B-lymphoma Moloney murine leukemia virus insertion region-1 (Bmi-1) acts as an oncogene in various tumors, and its overexpression correlates with a poor outcome in several human cancers. Ectopic expression of Bmi-1 can induce epithelial-mesenchymal transition (EMT) and enhance the motility and invasiveness of human nasopharyngeal epithelial cells (NPECs), whereas silencing endogenous Bmi-1 expression can reverse EMT and reduce the metastatic potential of nasopharyngeal cancer cells (NPCs). Mouse xenograft studies indicate that coexpression of Bmi-1 and H-Ras in breast cancer cells can induce an aggressive and metastatic phenotype with an unusual occurrence of brain metastasis; although, Bmi-1 overexpression did not result in oncogenic transformation of MCF-10A cells. However, the underlying molecular mechanism of Bmi-1-mediated progression and the metastasis of breast cancer are not fully elucidated at this time.
Results
Bmi-1 expression is more pronouncedly increased in primary cancer tissues compared to matched adjacent non-cancerous tissues. High Bmi-1 expression is correlated with advanced clinicopathologic classifications (T, N, and M) and clinical stages. Furthermore, a high level of Bmi-1 indicates an unfavorable overall survival and serves as a high risk marker for breast cancer. In addition, inverse transcriptional expression levels of Bmi-1 and E-cadherin are detected between the primary cancer tissues and the matched adjacent non-cancerous tissues. Higher Bmi-1 levels are found in the cancer tissue, whereas the paired adjacent non-cancer tissue shows higher E-cadherin levels. Overexpression of Bmi-1 increases the motility and invasive properties of immortalized human mammary epithelial cells, which is concurrent with the increased expression of mesenchymal markers, the decreased expression of epithelial markers, the stabilization of Snail and the dysregulation of the Akt/GSK3β pathway. Consistent with these observations, the repression of Bmi-1 in highly metastatic breast cancer cells remarkably reduces cellular motility, invasion and transformation, as well as tumorigenesis and lung metastases in nude mice. In addition, the repression of Bmi-1 reverses the expression of EMT markers and inhibits the Akt/GSK3β/Snail pathway.
Conclusions
This study demonstrates that Bmi-1 promotes the invasion and metastasis of human breast cancer and predicts poor survival.
Similar content being viewed by others
Background
The processes of invasion and metastasis that cause mortality in patients are extraordinarily distinctive features of breast cancer progression [1]. Although lymph-node metastasis, large tumor size, and poorly-differentiated histopathological grade are commonly considered to be established prognostic markers related to metastasis [2], distant metastasis still occurs in 20-30% of the patients with negative lymph-node involvement [3]. Thus far, Human Epidermal Growth Factor Receptor 2 (HER-2/neu) [4], c-myc [5] and HOXB9 [6] have emerged as predictors of the risk of metastasis in breast cancer. The aberrant expression of these factors may induce the expression of growth and angiogenic factors in tumors, leading to increased local concentrations of these factors within the tumor microenvironment and thus favoring tumor progression [6]. Recently, a new genomic test (gene-expression profiling) has been suggested to predict the clinical outcome more accurately than the traditional clinical and pathological standards [7, 8]. However, it is an open question as to whether this method will enter into the clinical routine for staging and grading [9]. Although these new markers and methods have been implicated, the molecular mechanism of breast cancer metastasis remains far from being fully understood due to the heterogeneity of this cancer and represents a new prerequisite for develo** better treatment strategies.
The polycomb (PcG) proteins constitute a global system with important roles in multi-cellular development, stem cell biology and cancer [10]. B-lymphoma Moloney murine leukemia virus insertion region-1 (Bmi-1), a member of the PcG family of transcription repressors, has emerged as a Myc-cooperating oncogene in murine lymphomas [11, 12]. Bmi-1 can not only lead human mammary epithelial cells (HMECs) to bypass senescence and immortalize, but it also can play a key role in human breast cancer [13, 14]. Moreover, a significant correlation has been observed between Bmi-1 expression and axillary lymph node metastasis in invasive ductal breast cancer [15]. These findings suggest that Bmi-1 could be involved in the carcinogenesis and metastasis of breast cancer. Although increasing evidence has shown that Bmi-1 expression is associated with unfavorable prognosis [16, 17], other studies have not confirmed these findings [18, 19]. Bmi-1 protein is detected in only 25% of African breast cancer patients and is associated with a low histological grade [18]. Additionally, higher Bmi-1 mRNA expression has been observed in early-stage patients without lymph node metastasis [20]. In contrast, up-regulation of Bmi-1 was shown to be associated with the invasion of nasopharyngeal carcinomas and to predict poor survival [84]. The blots were probed with mouse anti-Bmi-1, anti-E-cadherin, anti-β-catenin, anti-fibronectin and anti-vimentin antibodies (BD, Transduction Laboratories, Lexington, UK) as well as with rabbit anti-p-GSK, anti-t-GSK (Cell Signaling Technology, Inc. USA), anti-snail (Abcam, Cambridge Science Park, Cambridge, UK), anti-p-Akt (Santa Cruz Biotechnology, CA, USA) and goat anti-t-Akt (Santa Cruz Biotechnology, CA, USA) antibodies. The membranes were stripped and re-probed with mouse anti-α-tubulin (Sigma Aldrich, Inc. St Louis, Missouri, USA) to confirm equal loading of the samples.
Wound Healing Assay
Cells were seeded in six-well plates and cultured under permissive conditions until 90% confluence. After starving the cells for 24 h in medium without EGF or FBS, the confluent cell monolayer was lightly and quickly scratched with a pipette tip to produce a straight line. The debris was removed and the edge of the scratch was smoothed with PBS washing. The wound healing assays were done in growth factor-free medium, further excluding any effect due to a potential proliferation difference. The open gap was then inspected and photographed microscopically at indicated times, and is shown in the Figures at a 200X magnification. The migration activity was calculated as the number of cells entering into the rectangle. Experiments were repeated a minimum of three times.
Proliferation Assay
1 × 105 cells were plated on a P60 plate. Every 24 h, cells were trypsinized and counted under a light microscope at least three times until the sixth day. Experiments were repeated a minimum of three times.
Boyden Chamber Assay
This assay measures the ability of cells to invade a Matrigel matrix overlying a membrane containing 8-μm pores. Cells were seeded in medium deprived of EGF or FBS in the top chamber (BD), whereas medium containing EGF or FBS was added to the bottom chamber. After an appropriate cultivation time, the chambers were fixed with 1% paraformaldehyde and stained with hematoxylin. The number of cells in ten random fields of view was enumerated at 200X or 400X magnification for each filter. Three independent experiments were performed and the data are presented as the mean ± SD.
Three Dimensional Matrigel Culture
Matrigel (1.2 mg/ml, BD) was coated on the bottom of a 24-well plate. After Matrigel polymerization, cells were seeded into the well with growth medium containing 2% Matrigel. The cells were cultivated at 37°C incubation and alterations to the morphologic phenotype were monitored at 200X magnification every other day. Experiments were repeated a minimum of three times.
Anchorage-Independent Growth in Soft Agar
The soft agar assay was used to determine the propensity for anchorage-independent growth. Cells were plated in a 60-mm dish using 2 ml of growth medium, including 0.33% agar on the top of a bottom layer containing 0.66% agar. The cells were fed every two days with 1 ml medium. Colonies were photographed and counted in ten random fields of view at 200X magnification using light microscopy. Each experiment was done in triplicate.
Confocal Immunofluorescence Microscopy
Cells were seeded onto glass slides for 24 h, washed with PBS, fixed in 4% paraformaldehyde and permeabilized with 0.5% Triton X-100 for five minutes. After blocking with BSA, cells were stained with anti-snail primary antibody followed by FITC-conjugated anti-rabbit IgG. To visualize the nucleus, 4' 6-Diamidino-2-phenylindole (DAPI) staining was also performed, as previously described [85]. Immunofluorescence was detected by fluorescence microscopy (Olympus).
Mouse Injections, Necropsy, Histopathology
The ability to form tumors and metastasize was analyzed by injecting cells with repressed Bmi-1 into nude mice. Mice were bred and maintained under SPF conditions in the Department of Animal Center, Cancer Center, Sun Yat-Sen University, as approved by the China Care Committee Institute. Ten healthy female nude mice, which were four- to six- weeks old, were randomly assigned to each group. Each mouse was injected in the fat pad with 2 × 106 cells in PBS solution. Tumor growth was measured by caliper, and tumor volume was calculated according to the formula: length × width2 × 0.52, as described previously [86]. All mice were sacrificed on the sixth week after injection. The primary tumor and lung tissues of each mouse were removed, weighed and embedded in 10% paraffin. Each tissue was chopped into small pieces. Total protein was extracted to detect Bmi-1 expression from the primary xenografts. Each section from the primary xenografts and lung tissues was subjected to H&E staining, according to standard protocols, for histological examination and metastasis evaluation. The nodes of lung metastasis were quantified by counting metastatic lesions in ten sections (10 μm per section in a series). Data were collected by counting the total numbers of metastatic lesions from ten sections. Sections of primary tumors and lung lesions were used to detect the expression of the markers (Bmi-1, β-catenin, fibronectin) by IHC, as described previously.
Statistical analysis
The Chi-Square test was employed to evaluate the differences in Bmi-1 expression between the two categories of tissues. For assessment of the correlation between clinical features and Bmi-1 expression in breast cancer, P values were calculated by using the Chi-Square test or the Fisher's exact test. Relative risks (RRs) of death associated with Bmi-1 expression and other predictive variables were estimated by using the univariate and multivariate Cox proportional hazards model. The overall survival curve was plotted using Kaplan-Meier survival analysis and compared by the log-rank test. Result variations for the chamber invasion assays, wound healing assay, soft agar assay, tumor volume, tumor weight and lung metastasis lesions in mice, described as mean ± SD, were assessed using the two-tailed Student's t test. A value of P < 0.05 was considered significant (two tailed) by using SPSS 16.0.
Abbreviations
- Bmi-1:
-
B-lymphoma Moloney murine leukemia virus insertion region-1
- EMT:
-
epithelial-mesenchymal transition
- HER-2/neu:
-
Human Epidermal Growth Factor Receptor 2
- NPCs:
-
nasopharyngeal cancer cells
- NPECs:
-
nasopharyngeal epithelial cells.
References
Parkin DM, Bray F, Ferlay J, Pisani P: Global cancer statistics, 2002. CA: a cancer journal for clinicians. 2005, 55 (2): 74-108. 10.3322/canjclin.55.2.74 10.3322/canjclin.55.2.74
Carter CL, Allen C, Henson DE: Relation of tumor size, lymph node status, and survival in 24, 740 breast cancer cases. Cancer. 1989, 63 (1): 181-7. 10.1002/1097-0142(19890101)63:1<181::AID-CNCR2820630129>3.0.CO;2-H 10.1002/1097-0142(19890101)63:1<181::AID-CNCR2820630129>3.0.CO;2-H
Braun S, Pantel K, Muller P, Janni W, Hepp F, Kentenich CR, Gastroph S, Wischnik A, Dimpfl T, Kindermann G, Riethmüller G, Schlimok G: Cytokeratin-positive cells in the bone marrow and survival of patients with stage I, II, or III breast cancer. The New England journal of medicine. 2000, 342 (8): 525-33. 10.1056/NEJM200002243420801 10.1056/NEJM200002243420801
Zhang L, Sullivan P, Suyama J, Marchetti D: Epidermal growth factor-induced heparanase nucleolar localization augments DNA topoisomerase I activity in brain metastatic breast cancer. Mol Cancer Res. 2010, 8 (2): 278-90. 10.1158/1541-7786.MCR-09-0375 10.1158/1541-7786.MCR-09-0375
Wolfer A, Wittner BS, Irimia D, Flavin RJ, Lupien M, Gunawardane RN, Meyer CA, Lightcap ES, Tamayo P, Mesirov JP, Liu XS, Shioda T, Toner M, Loda M, Brown M, Brugge JS, Ramaswamy S: MYC regulation of a "poor-prognosis" metastatic cancer cell state. Proc Natl Acad Sci USA. 2010, 107 (8): 3698-703. 10.1073/pnas.0914203107
Hayashida T, Takahashi F, Chiba N, Brachtel E, Takahashi M, Godin-Heymann N, Gross KW, Vivanco MM, Wijendran V, Shioda T, Sgroi D, Donahoe PK, Maheswaran S: HOXB9, a gene overexpressed in breast cancer, promotes tumorigenicity and lung metastasis. Proc Natl Acad Sci USA. 2010, 107 (3): 1100-5. 10.1073/pnas.0912710107
Perou CM, Sorlie T, Eisen MB, van de Rijn M, Jeffrey SS, Rees CA, Pollack JR, Ross DT, Johnsen H, Akslen LA, Fluge O, Pergamenschikov A, Williams C, Zhu SX, Lønning PE, Børresen-Dale AL, Brown PO, Botstein D: Molecular portraits of human breast tumours. Nature. 2000, 406 (6797): 747-52. 10.1038/35021093
Wang Y, Klijn JG, Zhang Y, Sieuwerts AM, Look MP, Yang F, Talantov D, Timmermans M, Meijer-van Gelder ME, Yu J, Jatkoe T, Berns EM, Atkins D, Foekens JA: Gene-expression profiles to predict distant metastasis of lymph-node-negative primary breast cancer. Lancet. 2005, 365 (9460): 671-9.
Kallioniemi OP, Wagner U, Kononen J, Sauter G: Tissue microarray technology for high-throughput molecular profiling of cancer. Hum Mol Genet. 2001, 10 (7): 657-62. 10.1093/hmg/10.7.657
Bracken AP, Helin K: Polycomb group proteins: navigators of lineage pathways led astray in cancer. Nat Rev Cancer. 2009, 9 (11): 773-84. 10.1038/nrc2736
Haupt Y, Alexander WS, Barri G, Klinken SP, Adams JM: Novel zinc finger gene implicated as myc collaborator by retrovirally accelerated lymphomagenesis in E mu-myc transgenic mice. Cell. 1991, 65 (5): 753-63. 10.1016/0092-8674(91)90383-A
van Lohuizen M, Verbeek S, Scheijen B, Wientjens E, van der Gulden H, Berns A: Identification of cooperating oncogenes in E mu-myc transgenic mice by provirus tagging. Cell. 1991, 65 (5): 737-52. 10.1016/0092-8674(91)90382-9
Dimri GP, Martinez JL, Jacobs JJ, Keblusek P, Itahana K, Van Lohuizen M, Campisi J, Wazer DE, Band V: The Bmi-1 oncogene induces telomerase activity and immortalizes human mammary epithelial cells. Cancer research. 2002, 62 (16): 4736-45.
Lessard J, Sauvageau G: Bmi-1 determines the proliferative capacity of normal and leukaemic stem cells. Nature. 2003, 423 (6937): 255-60. 10.1038/nature01572
Kim JH, Yoon SY, Jeong SH, Kim SY, Moon SK, Joo JH, Lee Y, Choe IS, Kim JW: Overexpression of Bmi-1 oncoprotein correlates with axillary lymph node metastases in invasive ductal breast cancer. Breast. 2004, 13 (5): 383-8. 10.1016/j.breast.2004.02.010
Glinsky GV, Berezovska O, Glinskii AB: Microarray analysis identifies a death-from-cancer signature predicting therapy failure in patients with multiple types of cancer. J Clin Invest. 2005, 115 (6): 1503-21. 10.1172/JCI23412
Silva J, Garcia V, Garcia JM, Pena C, Dominguez G, Diaz R, Lorenzo Y, Hurtado A, Sánchez A, Bonilla F: Circulating Bmi-1 mRNA as a possible prognostic factor for advanced breast cancer patients. Breast Cancer Res. 2007, 9 (4): R55- 10.1186/bcr1760
Nalwoga H, Arnes JB, Wabinga H, Akslen LA: Expression of aldehyde dehydrogenase 1 (ALDH1) is associated with basal-like markers and features of aggressive tumours in African breast cancer. Br J Cancer. 2010, 102 (2): 369-75. 10.1038/sj.bjc.6605488
Choi YJ, Choi YL, Cho EY, Shin YK, Sung KW, Hwang YK, Lee SJ, Kong G, Lee JE, Kim JS, Kim JH, Yang JH, Nam SJ: Expression of Bmi-1 protein in tumor tissues is associated with favorable prognosis in breast cancer patients. Breast cancer research and treatment. 2009, 113 (1): 83-93. 10.1007/s10549-008-9909-4
Saeki M, Kobayashi D, Tsuji N, Kuribayashi K, Watanabe N: Diagnostic importance of overexpression of Bmi-1 mRNA in early breast cancers. Int J Oncol. 2009, 35 (3): 511-5.
Song LB, Zeng MS, Liao WT, Zhang L, Mo HY, Liu WL, Shao JY, Wu QL, Li MZ, **a YF, Fu LW, Huang WL, Dimri GP, Band V, Zeng YX: Bmi-1 is a novel molecular marker of nasopharyngeal carcinoma progression and immortalizes primary human nasopharyngeal epithelial cells. Cancer Res. 2006, 66 (12): 6225-32. 10.1158/0008-5472.CAN-06-0094
Li DW, Tang HM, Fan JW, Yan DW, Zhou CZ, Li SX, Wang XL, Peng ZH: Expression level of Bmi-1 oncoprotein is associated with progression and prognosis in colon cancer. J Cancer Res Clin Oncol. 2009
Liu JH, Song LB, Zhang X, Guo BH, Feng Y, Li XX, Liao WT, Zeng MS, Huang KH: Bmi-1 expression predicts prognosis for patients with gastric carcinoma. J Surg Oncol. 2008, 97 (3): 267-72. 10.1002/jso.20934
Zhang XW, Sheng YP, Li Q, Qin W, Lu YW, Cheng YF, Liu BY, Zhang FC, Li J, Dimri GP, Guo WJ: BMI1 and Mel-18 oppositely regulate carcinogenesis and progression of gastric cancer. Mol Cancer. 2010, 9 (1): 40- 10.1186/1476-4598-9-40
Mihic-Probst D, Kuster A, Kilgus S, Bode-Lesniewska B, Ingold-Heppner B, Leung C, Storz M, Seifert B, Marino S, Schraml P, Dummer R, Moch H: Consistent expression of the stem cell renewal factor BMI-1 in primary and metastatic melanoma. Int J Cancer. 2007, 121 (8): 1764-70. 10.1002/ijc.22891
Jiang Y, Su B, Meng X, Liu C, Liu B, Liu D, Fan Y, Yang H: Effect of siRNA-mediated silencing of Bmi-1 gene expression on HeLa cells. Cancer Sci. 101 (2): 379-86.
Song LB, Li J, Liao WT, Feng Y, Yu CP, Hu LJ, Kong QL, Xu LH, Zhang X, Liu WL, Li MZ, Zhang L, Kang TB, Fu LW, Huang WL, **a YF, Tsao SW, Li M, Band V, Band H, Shi QH, Zeng YX, Zeng MS: The polycomb group protein Bmi-1 represses the tumor suppressor PTEN and induces epithelial-mesenchymal transition in human nasopharyngeal epithelial cells. J Clin Invest. 2009, 119 (12): 3626-36. 10.1172/JCI39374
Hoenerhoff MJ, Chu I, Barkan D, Liu ZY, Datta S, Dimri GP, Green JE: BMI1 cooperates with H-RAS to induce an aggressive breast cancer phenotype with brain metastases. Oncogene. 2009, 28 (34): 3022-32. 10.1038/onc.2009.165
Langley RR, Fidler IJ: Tumor cell-organ microenvironment interactions in the pathogenesis of cancer metastasis. Endocr Rev. 2007, 28 (3): 297-321. 10.1210/er.2006-0027
Sleeman JP: The lymph node as a bridgehead in the metastatic dissemination of tumors. Recent results in cancer research Fortschritte der Krebsforschung. 2000, 157: 55-81.
Pantel K, Brakenhoff RH: Dissecting the metastatic cascade. Nature reviews. 2004, 4 (6): 448-56. 10.1038/nrc1370
Thiery JP: Epithelial-mesenchymal transitions in tumour progression. Nature reviews. 2002, 2 (6): 442-54. 10.1038/nrc822
Nieto MA: The snail superfamily of zinc-finger transcription factors. Nat Rev Mol Cell Biol. 2002, 3 (3): 155-66. 10.1038/nrm757
Behrens J, Lowrick O, Klein-Hitpass L, Birchmeier W: The E-cadherin promoter: functional analysis of a G.C-rich region and an epithelial cell-specific palindromic regulatory element. Proceedings of the National Academy of Sciences of the USA. 1991, 88 (24): 11495-9. 10.1073/pnas.88.24.11495
Hajra KM, Ji X, Fearon ER: Extinction of E-cadherin expression in breast cancer via a dominant repression pathway acting on proximal promoter elements. Oncogene. 1999, 18 (51): 7274-9. 10.1038/sj.onc.1203336
Giroldi LA, Bringuier PP, de Weijert M, Jansen C, van Bokhoven A, Schalken JA: Role of E boxes in the repression of E-cadherin expression. Biochemical and biophysical research communications. 1997, 241 (2): 453-8. 10.1006/bbrc.1997.7831
Batlle E, Sancho E, Franci C, Dominguez D, Monfar M, Baulida J, García De Herreros A: The transcription factor snail is a repressor of E-cadherin gene expression in epithelial tumour cells. Nat Cell Biol. 2000, 2 (2): 84-9. 10.1038/35000034
Cano A, Perez-Moreno MA, Rodrigo I, Locascio A, Blanco MJ, del Barrio MG, Portillo F, Nieto MA: The transcription factor snail controls epithelial-mesenchymal transitions by repressing E-cadherin expression. Nat Cell Biol. 2000, 2 (2): 76-83. 10.1038/35000025
Zhou BP, Deng J, **a W, Xu J, Li YM, Gunduz M, Hung MC: Dual regulation of Snail by GSK-3beta-mediated phosphorylation in control of epithelial-mesenchymal transition. Nat Cell Biol. 2004, 6 (10): 931-40. 10.1038/ncb1173
Blanco MJ, Moreno-Bueno G, Sarrio D, Locascio A, Cano A, Palacios J, Nieto MA: Correlation of Snail expression with histological grade and lymph node status in breast carcinomas. Oncogene. 2002, 21 (20): 3241-6. 10.1038/sj.onc.1205416
Cheng CW, Wu PE, Yu JC, Huang CS, Yue CT, Wu CW, Shen CY: Mechanisms of inactivation of E-cadherin in breast carcinoma: modification of the two-hit hypothesis of tumor suppressor gene. Oncogene. 2001, 20 (29): 3814-23. 10.1038/sj.onc.1204505
Come C, Magnino F, Bibeau F, De Santa Barbara P, Becker KF, Theillet C, Savagner P: Snail and slug play distinct roles during breast carcinoma progression. Clin Cancer Res. 2006, 12 (18): 5395-402. 10.1158/1078-0432.CCR-06-0478
Takkunen M, Grenman R, Hukkanen M, Korhonen M, Garcia de Herreros A, Virtanen I: Snail-dependent and -independent epithelial-mesenchymal transition in oral squamous carcinoma cells. J Histochem Cytochem. 2006, 54 (11): 1263-75. 10.1369/jhc.6A6958.2006
Micalizzi DS, Christensen KL, Jedlicka P, Coletta RD, Baron AE, Harrell JC, Horwitz KB, Billheimer D, Heichman KA, Welm AL, Schiemann WP, Ford HL: The Six1 homeoprotein induces human mammary carcinoma cells to undergo epithelial-mesenchymal transition and metastasis in mice through increasing TGF-beta signaling. J Clin Invest. 2009, 119 (9): 2678-90. 10.1172/JCI37815
Evdokimova V, Tognon C, Ng T, Ruzanov P, Melnyk N, Fink D, Sorokin A, Ovchinnikov LP, Davicioni E, Triche TJ, Sorensen PH: Translational activation of snail1 and other developmentally regulated transcription factors by YB-1 promotes an epithelial-mesenchymal transition. Cancer Cell. 2009, 15 (5): 402-15. 10.1016/j.ccr.2009.03.017
Tryndyak VP, Beland FA, Pogribny IP: E-cadherin transcriptional down-regulation by epigenetic and microRNA-200 family alterations is related to mesenchymal and drug-resistant phenotypes in human breast cancer cells. Int J Cancer. 2010, 126 (11): 2575-83.
Cowell JK, LaDuca J, Rossi MR, Burkhardt T, Nowak NJ, Matsui S: Molecular characterization of the t(3;9) associated with immortalization in the MCF10A cell line. Cancer genetics and cytogenetics. 2005, 163 (1): 23-9. 10.1016/j.cancergencyto.2005.04.019
Cailleau R, Olive M, Cruciger QV: Long-term human breast carcinoma cell lines of metastatic origin: preliminary characterization. In Vitro. 1978, 14 (11): 911-5. 10.1007/BF02616120
Kremer M, Quintanilla-Martinez L, Fuchs M, Gamboa-Dominguez A, Haye S, Kalthoff H, Rosivatz E, Hermannstädter C, Busch R, Höfler H, Luber B: Influence of tumor-associated E-cadherin mutations on tumorigenicity and metastasis. Carcinogenesis. 2003, 24 (12): 1879-86. 10.1093/carcin/bgg148
Guo WJ, Zeng MS, Yadav A, Song LB, Guo BH, Band V, Dimri GP: Mel-18 acts as a tumor suppressor by repressing Bmi-1 expression and down-regulating Akt activity in breast cancer cells. Cancer Res. 2007, 67 (11): 5083-9. 10.1158/0008-5472.CAN-06-4368
Guo WJ, Datta S, Band V, Dimri GP: Mel-18, a polycomb group protein, regulates cell proliferation and senescence via transcriptional repression of Bmi-1 and c-Myc oncoproteins. Molecular biology of the cell. 2007, 18 (2): 536-46. 10.1091/mbc.E06-05-0447
Gong Y, Wang X, Liu J, Shi L, Yin B, Peng X, Qiang B, Yuan J: NSPc1, a mainly nuclear localized protein of novel PcG family members, has a transcription repression activity related to its PKC phosphorylation site at S183. FEBS letters. 2005, 579 (1): 115-21. 10.1016/j.febslet.2004.11.056
Noguchi K, Shiurba R, Higashinakagawa T: Nuclear translocation of mouse polycomb m33 protein in regenerating liver. Biochemical and biophysical research communications. 2002, 291 (3): 508-15. 10.1006/bbrc.2002.6480
Alkema MJ, Bronk M, Verhoeven E, Otte A, van 't Veer LJ, Berns A, van Lohuizen M: Identification of Bmi1-interacting proteins as constituents of a multimeric mammalian polycomb complex. Genes & development. 1997, 11 (2): 226-40.
Sawa M, Yamamoto K, Yokozawa T, Kiyoi H, Hishida A, Kajiguchi T, Seto M, Kohno A, Kitamura K, Itoh Y, Asou N, Hamajima N, Emi N, Naoe T: BMI-1 is highly expressed in M0-subtype acute myeloid leukemia. Int J Hematol. 2005, 82 (1): 42-7. 10.1532/IJH97.05013
Mihara K, Chowdhury M, Nakaju N, Hidani S, Ihara A, Hyodo H, Yasunaga S, Takihara Y, Kimura A: Bmi-1 is useful as a novel molecular marker for predicting progression of myelodysplastic syndrome and patient prognosis. Blood. 2006, 107 (1): 305-8. 10.1182/blood-2005-06-2393
Breuer RH, Snijders PJ, Sutedja GT, Sewalt RG, Otte AP, Postmus PE, Meijer CJ, Raaphorst FM, Smit EF: Expression of the p16(INK4a) gene product, methylation of the p16(INK4a) promoter region and expression of the polycomb-group gene BMI-1 in squamous cell lung carcinoma and premalignant endobronchial lesions. Lung Cancer. 2005, 48 (3): 299-306. 10.1016/j.lungcan.2004.11.026
Kim JH, Yoon SY, Kim CN, Joo JH, Moon SK, Choe IS, Choe YK, Kim JW: The Bmi-1 oncoprotein is overexpressed in human colorectal cancer and correlates with the reduced p16INK4a/p14ARF proteins. Cancer Lett. 2004, 203 (2): 217-24. 10.1016/j.canlet.2003.07.009
Silva J, Garcia JM, Pena C, Garcia V, Dominguez G, Suarez D, Camacho FI, Espinosa R, Provencio M, España P, Bonilla F: Implication of polycomb members Bmi-1, Mel-18, and Hpc-2 in the regulation of p16INK4a, p14ARF, h-TERT, and c-Myc expression in primary breast carcinomas. Clin Cancer Res. 2006, 12 (23): 6929-36. 10.1158/1078-0432.CCR-06-0788
Miller WR: Clinical, pathological, proliferative and molecular responses associated with neoadjuvant aromatase inhibitor treatment in breast cancer. The Journal of steroid biochemistry and molecular biology. J Steroid Biochem Mol Biol. 2010, 118 (4-5): 273-6. 10.1016/j.jsbmb.2009.10.005
Baumann CK, Castiglione-Gertsch M: Clinical use of selective estrogen receptor modulators and down regulators with the main focus on breast cancer. Minerva ginecologica. 2009, 61 (6): 517-39.
Sotiriou C, Pusztai L: Gene-expression signatures in breast cancer. N Engl J Med. 2009, 360 (8): 790-800. 10.1056/NEJMra0801289
Yoshida BA, Sokoloff MM, Welch DR, Rinker-Schaeffer CW: Metastasis-suppressor genes: a review and perspective on an emerging field. J Natl Cancer Inst. 2000, 92 (21): 1717-30. 10.1093/jnci/92.21.1717
Leuschner C, Enright FM, Gawronska B, Hansel W: Membrane disrupting lytic peptide conjugates destroy hormone dependent and independent breast cancer cells in vitro and in vivo. Breast cancer research and treatment. 2003, 78 (1): 17-27. 10.1023/A:1022169525521
Price JE, Polyzos A, Zhang RD, Daniels LM: Tumorigenicity and metastasis of human breast carcinoma cell lines in nude mice. Cancer research. 1990, 50 (3): 717-21.
Goldson TM, Vielhauer G, Staub E, Miller S, Shim H, Hagedorn CH: Eukaryotic initiation factor 4E variants alter the morphology, proliferation, and colony-formation properties of MDA-MB-435 cancer cells. Molecular carcinogenesis. 2007, 46 (1): 71-84. 10.1002/mc.20276
Grunert S, Jechlinger M, Beug H: Diverse cellular and molecular mechanisms contribute to epithelial plasticity and metastasis. Nat Rev Mol Cell Biol. 2003, 4 (8): 657-65. 10.1038/nrm1175
Waerner T, Alacakaptan M, Tamir I, Oberauer R, Gal A, Brabletz T, Schreiber M, Jechlinger M, Beug H: ILEI: a cytokine essential for EMT, tumor formation, and late events in metastasis in epithelial cells. Cancer Cell. 2006, 10 (3): 227-39. 10.1016/j.ccr.2006.07.020
Ribeiro AS, Albergaria A, Sousa B, Correia AL, Bracke M, Seruca R, Schmitt FC, Paredes J: Extracellular cleavage and shedding of P-cadherin: a mechanism underlying the invasive behaviour of breast cancer cells. Oncogene. 2009, 29 (3): 392-402. 10.1038/onc.2009.338
Denk C, Hulsken J, Schwarz E: Reduced gene expression of E-cadherin and associated catenins in human cervical carcinoma cell lines. Cancer letters. 1997, 120 (2): 185-93. 10.1016/S0304-3835(97)00308-X
Cavallaro U, Christofori G: Cell adhesion and signalling by cadherins and Ig-CAMs in cancer. Nature reviews. 2004, 4 (2): 118-32. 10.1038/nrc1276
Chan KS, Sano S, Kiguchi K, Anders J, Komazawa N, Takeda J, DiGiovanni J: Disruption of Stat3 reveals a critical role in both the initiation and the promotion stages of epithelial carcinogenesis. The Journal of clinical investigation. 2004, 114 (5): 720-8.
Yang J, Mani SA, Donaher JL, Ramaswamy S, Itzykson RA, Come C, Savagner P, Gitelman I, Richardson A, Weinberg RA: Twist, a master regulator of morphogenesis, plays an essential role in tumor metastasis. Cell. 2004, 117 (7): 927-39. 10.1016/j.cell.2004.06.006
Reichmann E, Schwarz H, Deiner EM, Leitner I, Eilers M, Berger J, Busslinger M, Beug H: Activation of an inducible c-FosER fusion protein causes loss of epithelial polarity and triggers epithelial-fibroblastoid cell conversion. Cell. 1992, 71 (7): 1103-16. 10.1016/S0092-8674(05)80060-1
Grille SJ, Bellacosa A, Upson J, Klein-Szanto AJ, van Roy F, Lee-Kwon W, Donowitz M, Tsichlis PN, Larue L: The protein kinase Akt induces epithelial mesenchymal transition and promotes enhanced motility and invasiveness of squamous cell carcinoma lines. Cancer research. 2003, 63 (9): 2172-8.
Hulit J, Suyama K, Chung S, Keren R, Agiostratidou G, Shan W, Dong X, Williams TM, Lisanti MP, Knudsen K, Hazan RB: N-cadherin signaling potentiates mammary tumor metastasis via enhanced extracellular signal-regulated kinase activation. Cancer research. 2007, 67 (7): 3106-16. 10.1158/0008-5472.CAN-06-3401
Rasbridge SA, Gillett CE, Sampson SA, Walsh FS, Millis RR: Epithelial (E-) and placental (P-) cadherin cell adhesion molecule expression in breast carcinoma. The Journal of pathology. 1993, 169 (2): 245-50. 10.1002/path.1711690211
Kowalski PJ, Rubin MA, Kleer CG: E-cadherin expression in primary carcinomas of the breast and its distant metastases. Breast Cancer Res. 2003, 5 (6): R217-22. 10.1186/bcr651
Bukholm IK, Nesland JM, Borresen-Dale AL: Re-expression of E-cadherin, alpha-catenin and beta-catenin, but not of gamma-catenin, in metastatic tissue from breast cancer patients [seecomments]. The Journal of pathology. 2000, 190 (1): 15-9. 10.1002/(SICI)1096-9896(200001)190:1<15::AID-PATH489>3.0.CO;2-L
Rashid MG, Sanda MG, Vallorosi CJ, Rios-Doria J, Rubin MA, Day ML: Posttranslational truncation and inactivation of human E-cadherin distinguishes prostate cancer from matched normal prostate. Cancer research. 2001, 61 (2): 489-92.
Altomare DA, Testa JR: Perturbations of the AKT signaling pathway in human cancer. Oncogene. 2005, 24 (50): 7455-64. 10.1038/sj.onc.1209085
Bernards R, Weinberg RA: A progression puzzle. Nature. 2002, 418 (6900): 823- 10.1038/418823a
Borgquist S, Holm C, Stendahl M, Anagnostaki L, Landberg G, Jirstrom K: Oestrogen receptors alpha and beta show different associations to clinicopathological parameters and their co-expression might predict a better response to endocrine treatment in breast cancer. J Clin Pathol. 2008, 61 (2): 197-203. 10.1136/jcp.2006.040378
Dimri GP, Itahana K, Acosta M, Campisi J: Regulation of a senescence checkpoint response by the E2F1 transcription factor and p14(ARF) tumor suppressor. Molecular and cellular biology. 2000, 20 (1): 273-85. 10.1128/MCB.20.1.273-285.2000
Chung H, Jung JY, Cho SD, Hong KA, Kim HJ, Shin DH, Kim H, Kim HO, Shin DH, Lee HW, Jeong LS, Kong G: The antitumor effect of LJ-529, a novel agonist to A3 adenosine receptor, in both estrogen receptor-positive and estrogen receptor-negative human breast cancers. Mol Cancer Ther. 2006, 5 (3): 685-92. 10.1158/1535-7163.MCT-05-0245
Shao R, Bao S, Bai X, Blanchette C, Anderson RM, Dang T, Gishizky ML, Marks JR, Wang XF: Acquired expression of periostin by human breast cancers promotes tumor angiogenesis through up-regulation of vascular endothelial growth factor receptor 2 expression. Molecular and cellular biology. 2004, 24 (9): 3992-4003. 10.1128/MCB.24.9.3992-4003.2004
Acknowledgements
We are grateful to Prof. Vimla Band (Eppley Institute for Cancer and Allied Diseases, University of Nebraska Medical Center, Omaha, USA) for providing the cell lines. We appreciate the technical help from the Sun Yat-sen University Pathology Department. We wish to express warm thanks to Professor Wenjie Zhang from Tongji Medical University for review of the manuscript. We acknowledge the grants for this study from the National Natural Science Foundation of China (81025014 and 91019015), and Specialized Research Fund for the Doctoral Program of Higher Education (20070558270).
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
The authors declare that they have no competing interests.
Authors' contributions
BHG and YF were involved in the design, performed the experiments, and drafted the manuscript. RZ, LHX, MZL participated in sample collection. HFK and LBS reviewed the manuscript. MSZ conceived the idea for the study, contributed to the overall experiment design and revised the manuscript. All authors read and approved the final manuscript.
Bao-Hong Guo, Yan Feng contributed equally to this work.
Electronic supplementary material
12943_2010_843_MOESM3_ESM.PDF
Additional file 3:Table S3(PDF). Antigen retrieval method, recourse of antibody and developmental time in different studies. (PDF 12 KB)
Authors’ original submitted files for images
Below are the links to the authors’ original submitted files for images.
Rights and permissions
Open Access This article is published under license to BioMed Central Ltd. This is an Open Access article is distributed under the terms of the Creative Commons Attribution License ( https://creativecommons.org/licenses/by/2.0 ), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
About this article
Cite this article
Guo, BH., Feng, Y., Zhang, R. et al. Bmi-1 promotes invasion and metastasis, and its elevated expression is correlated with an advanced stage of breast cancer. Mol Cancer 10, 10 (2011). https://doi.org/10.1186/1476-4598-10-10
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/1476-4598-10-10