Abstract
Background
Hypertonic saline (HTS) reduces the severity of lung injury in ischemia-reperfusion, endotoxin-induced and ventilation-induced lung injury. However, the potential for HTS to modulate the resolution of lung injury is not known. We investigated the potential for hypertonic saline to modulate the evolution and resolution of oleic acid induced lung injury.
Methods
Adult male Sprague Dawley rats were used in all experiments. Series 1examined the potential for HTS to reduce the severity of evolving oleic acid (OA) induced acute lung injury. Following intravenous OA administration, animals were randomized to receive isotonic (Control, n = 12) or hypertonic saline (HTS, n = 12), and the extent of lung injury assessed after 6 hours. Series 2examined the potential for HTS to enhance the resolution of oleic acid (OA) induced acute lung injury. Following intravenous OA administration, animals were randomized to receive isotonic (Control, n = 6) or hypertonic saline (HTS, n = 6), and the extent of lung injury assessed after 6 hours.
Results
In Series I, HTS significantly reduced bronchoalveolar lavage (BAL) neutrophil count compared to Control [61.5 ± 9.08 versus 102.6 ± 11.89 × 103 cells.ml-1]. However, there were no between group differences with regard to: A-a O2 gradient [11.9 ± 0.5 vs. 12.0 ± 0.5 KPa]; arterial PO2; static lung compliance, or histologic injury. In contrast, in Series 2, hypertonic saline significantly reduced histologic injury and reduced BAL neutrophil count [24.5 ± 5.9 versus 46.8 ± 4.4 × 103 cells.ml-1], and interleukin-6 levels [681.9 ± 190.4 versus 1365.7 ± 246.8 pg.ml-1].
Conclusion
These findings demonstrate, for the first time, the potential for HTS to reduce pulmonary inflammation and enhance the resolution of oleic acid induced lung injury.
Similar content being viewed by others
Background
Hypertonic saline (7.5% saline, HTS) exhibits considerable potential as a therapeutic agent in diverse injury models. HTS has been demonstrated to inhibit acute lung injury (ALI) induced by systemic ischemia-reperfusion [1], hemorrhagic shock [2], and acute pancreatitis [3, 4] in experimental models. The mechanisms of action of hypertonic saline are increasingly well understood, and include inhibition of neutrophil adhesion molecule CD11b [5], reduced TNF-α and IL- l production [1], and reduced activation of MAP kinase p38 and ERK-1 [6]. Pulmonary neutrophil sequestration, which is central to the mechanism of injury in ALI, is attenuated by HTS in diverse ALI models [1–3, 7]. The therapeutic potential of HTS is demonstrated by its efficacy when used following initiation of the injury process, in both ischemia-reperfusion and pancreatitis induced ALI [1, 3]. HTS has also demonstrated efficacy in clinical human trials, in patients with post-traumatic cerebral oedema [7].
Oleic acid induced lung injury is a well characterized and clinically relevant model of ALI/ARDS [8–12]. In particular, it constitutes an excellent model of Fat Embolism Syndrome (FES) induced ALI [13], given that OA is a major component of the marrow-derived fat emboli released into the circulation following traumatic bone injury [14, 15]. Oleic acid produced a rapidly evolving lung injury [10], which features increased capillary permeability induced pulmonary edema [10] and alveolar infiltration of inflammatory cells [16]. The ALI produced by OA is relatively transient, and resolves over several hours [10]. This model therefore permits an evaluation of the therapeutic potential of HTS during both the injury and resolution phases of ALI [10].
The potential for HTS to modulate the resolution of lung injury is not known. We investigated the potential for hypertonic saline to modulate the evolution and resolution of oleic acid induced lung injury. Specifically, we hypothesized that HTS would modulate the severity of OA induced ALI, reducing lung injury and/or enhancing resolution of ALI. We used this model to determine the therapeutic potential of hypertonic saline in both evolving (Series 1) and resolving (Series 2) ALI.
Methods
All experimental work was reviewed and approved by the Research Ethics Committee at the National University of Ireland, Galway and conducted under license from the Department of Health and Children, Dublin, Ireland.
Animal Care
Specific pathogen free adult male Sprague Dawley rats (B&K Universal Ltd., U.K.) weighing 300 to 380 g were used in all experiments. Animals were housed for a minimum of 7 days prior to study, under controlled light/dark conditions where the light period was from 8:00 a.m. to 8:00 p.m. They were allowed access to ordinary rat chow and tap water ad libitum. Animals were maintained at constant ambient temperature of 21–22°C, while the humidity level was maintained between 45% and 55%.
Fat Embolism Syndrome Model
The experimental model was based on that previously reported, with several modifications [8–12]. Briefly, anesthesia was induced and maintained with Isoflurane (Abbott Laboratories, UK). After confirming depth of anesthesia by absence of response to paw compression, a tail vein was cannulated using a 24 gauge cannula (Becton Dickinson, NJ). Oleic acid (OA) (Sigma-Aldrich, United Kingdom), which was prepared as a 1:1 mixture with pure ethanol [17], was administered intravenously. Animals were then randomized to hypertonic saline (HTS) or control groups. The HTS group were then administered 4 ml.Kg-1 of 7.5% hypertonic saline and the control animals administered an equal volume of 0.9% saline. The animals were then allowed to recover from anesthesia, and then placed in their cages.
Preliminary Studies
Two preliminary series of experiments was carried out to determine the dose of OA and duration of time required to produce a significant evolving ALI, and to produce a model of resolving lung injury. A dose of 40 μl of OA was determined to produce a significant early lung injury over a 4 h period. In later studies, a dose of 9 μl per 100 g body weight was found to produce a lung injury of similar magnitude at 4 hours, and which was resolving at 6 hours following OA administration.
Series I – Evolving ALI
This series was carried out to determine the potential for HTS to attenuate evolving OA-induced injury. Following induction of anesthesia, 40 μl of OA was administered and each rat allowed to recover. Four hours following OA administration, the animals were re-anesthetized and the degree of ALI quantified.
Series II – Resolving ALI
This series was carried out to determine whether HTS could modulate the resolution of OA-induced injury. Following induction of anesthesia, 9 μl.100 g-1 body weight of OA was administered and each rat was allowed to recover. Six hours following OA administration, the animals were re-anesthetized and the extent of lung injury quantified.
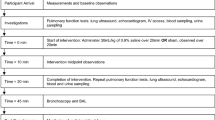
Assessment of Lung Injury
At four (Series I) or six (Series II) hours following OA administration, the animals were re-anesthetized with Isoflurane. After confirming depth of anesthesia by absence of response to paw compression, the dorsal penile vein and carotid artery were cannulated using 22G cannulae (Becton Dickinson, NJ). A tracheotomy was performed, and a tracheal tube was inserted to a depth of 2 cm and secured in place. Pancuronium (1 mg; Organon, The Netherlands) was administered intravenously and the lungs were then ventilated using a small animal ventilator (Model 683; Harvard Apparatus, United Kingdom) with a fractional inspired O2 (FiO2) of 0.21 (room air), respiratory rate 90 min.-1, tidal volume 4.5 ml.kg-1 and 2 cm H2O positive end-expiratory pressure (PEEP).
Systemic arterial pressure, peak airway pressures and temperature were measured throughout the protocol. Arterial blood samples then were drawn for assessment of systemic oxygenation, ventilation and acid-base status (ABL 710, Radiometer, United Kingdom). Static inflation lung compliance was measured immediately prior to a recruitment manoeuvre, ensuring a standardized lung volume history. Incremental 1 ml volumes of room air were injected via the tracheal cannula, and the pressure attained 3 seconds after each injection was measured, until a total volume of 5 ml was injected. At the end of the protocol, the inspired gas was altered to FiO2 of 1.0 for 5 minutes, and an arterial blood sample was then taken for calculation of alveolar-arterial oxygen gradient. The animals were then euthanized by exsanguination under anesthesia.
Sampling and Assay Protocol
Immediately post mortem, the heart-lung block was dissected from the thorax and bronchoalveolar lavage (BAL) performed. BAL was carried out by intratracheal instillation of 3 aliquots (5 ml each) of isotonic saline and collection of the returned fluid by free drainage. Total cell numbers per ml in BAL fluid were counted and differential cell counts were performed following staining with Diff-Quik (BDH, United Kingdom). Samples of BAL fluid were centrifuged, snap frozen in liquid N2 and stored at -80°C. The concentration of interleukin-6 (IL-6) in these BAL samples was determined using quantitative sandwich ELISA's (R&D Systems, United Kingdom). The BAL protein concentration was determined using a standard assay (Biorad Assay, Biorad, Hercules, CA).
The left lung was isolated and fixed with 4% paraformaldehyde [18, 19], and the extent of histologic lung damage determined using quantitative stereological techniques as previously described [20].
Statistical Analysis
Results are expressed as mean ± (SEM) for normally distributed data, and as median (interquartile range, IQR) if non-normally distributed. Data were analyzed by one-way ANOVA followed by Student-Newman-Keuls, t-test or Kruskalis-Wallis followed by Mann-Whitney U test with the Bonferroni correction for multiple comparisons, as appropriate. P < 0.05 was considered statistically significant.
Results
Series 1 – Evolving OA induced ALI
12 animals were entered into this study. All animals entered into the study survived the full duration of the protocol.
Physiologic Indices of Lung Damage
There was no difference between the groups with regard to arterial oxygen tension, or alveolar-arterial gradient at 21% or 100% oxygen [Table 1]. There was no difference in peak airway pressures or in static lung compliance between the groups [Table 1].
Lung Damage and Inflammation
HTS significantly reduced BAL neutrophil counts compared to control conditions [Figure 1]. BAL IL-6 [Figure 2], and BAL protein levels [Table 1] were reduced with HTS, although these differences were not statistically significant [Figure 3]. However, there was no between group difference in the degree of histologic injury. Quantitative stereological analysis demonstrated that there was no significant difference between HTS and Control in regard to the amount of tissue or airspace in the gas exchanging portion of the lung.
Series 2 – Resolving OA induced ALI
24 animals were entered into this study. All animals entered into the study survived the full duration of the protocol.
Physiologic indices of Lung Damage
There was no difference between the groups with regard to arterial oxygen tension, or alveolar-arterial gradient at 21% or 100% oxygen [Table 2]. There was no difference in peak airway pressures or in static lung compliance between the groups [Table 2].
Lung Damage and Inflammation
HTS significantly reduced BAL neutrophil counts [Figure 4], and BAL IL-6 concentrations [Figure 5] compared to control conditions. BAL protein levels were reduced with HTS, although these differences were not statistically significant [Table 2]. HTS significantly reduced the degree of histologic injury compared to isotonic saline [Figure 6]. Quantitative stereological analysis demonstrated that HTS significantly increased alveolar airspace, and significantly reduced alveolar tissue, indicating reduced histologic lung damage, compared to control conditions.
Discussion
We demonstrate for the first time the potential for hypertonic saline to modulate the resolution of acute lung injury. Hypertonic saline reduced alveolar neutrophil infiltration in both evolving and resolving oleic induced ALI. Of perhaps greater significance, HTS enhanced the resolution of OA induced lung injury, as evidenced by a reduced severity of histologic injury, and reduced indices of inflammation, compared to control conditions.
HTS – Therapeutic Potential in ALI
The neutrophil-endothelial cell interaction is central to the pathogenesis of ALI/ARDS. HTS is a potent inhibitor of neutrophil function, downregulating neutrophil oxidative burst activity [21], reducing neutrophil adhesion molecule expression [22] and suppressing neutrophil activation and the release of pro-inflammatory cytokines [5, 23]. HTS decreased lung neutrophil infiltration [24, 25] and ICAM-1 [25] expression in the setting of hemorrhagic shock.
HTS has been demonstrated to reduce pulmonary edema, histologic injury, and lung neutrophil infiltration following systemic ischemia-reperfusion injury [1]. HTS also reduced serum IL-6 and TNF-α cytokine levels in this study. HTS reduced the increase in lung permeability and lung neutrophil sequestration and activation following trauma-haemorrhagic shock [26]. HTS resuscitation also increased survival, and reduced lung injury, in a two-hit injury model of hemorrhage followed by cecal ligation and puncture in mice [27]. HTS transiently improved tissue oxygen delivery and increased oxygen consumption in a canine model of oleic acid-induced lung injury [28]. However, the potential for HTS to modulate oleic acid-induced ALI has not been assessed
Effect of HTS on evolving ALI
HTS did not reduce the severity of evolving oleic acid induced ALI. There was no difference between HTS and an equal volume of isotonic saline in terms of arterial oxygenation, pulmonary shunt or lung static or dynamic compliance. The degree of histologic injury on quantitative stereological analysis was similar with HTS versus isotonic saline, with no difference in the amount of tissue or airspace in the gas exchanging portion of the lung. In contrast to these findings, HTS did appear to reduce pulmonary inflammation, significantly reducing bronchoalveolar lavage neutrophil cell counts, in kee** with previous findings in hemorrhage-induced ALI models [22, 24, 25]. While the bronchoalveolar lavage protein and interleukin-6 levels showed a clear trend towards decrease in the HTS group, the results were not statistically significant. Therefore, while HTS reduced indices of pulmonary inflammation, it not attenuate the severity of oleic acid induced ALI.
HTS enhances resolution of ALI
A key feature of the oleic acid model of ALI is the fact that the injury is transient, permitting study of the effects of HTS on the resolution of the ALI. HTS did enhance the resolution of oleic acid induced ALI. Of importance, the degree of histologic injury on quantitative stereological analysis was clearly reduced by HTS. Specifically, there was a significantly reduced amount of tissue and a significantly greater amount of airspace in the gas exchanging portion of the lung. Furthermore, HTS reduced pulmonary inflammation, significantly reducing bronchoalveolar lavage neutrophil cell counts and interleukin-6 levels. Interestingly, HTS did not modulate physiologic indices of lung injury, in terms of arterial oxygenation, pulmonary shunt or lung static or dynamic compliance. This may reflect the fact that different parameters of lung injury and damage may resolve over differing time courses.
Limitations of findings
Our study has a number of limitations. In particular, it is not clear whether the effects seen are a function of the additional saline load, or the hypertonicity per se. We chose to use a control group of an equal volume of isotonic saline in order to compare the effects of equal infusion volumes. Additional studies, which compare the effects of HTS to an equi-osmolar load of isotonic saline, are required. The relatively short experimental time frames studied may have restricted the capacity to fully characterize the therapeutic potential of HTS, particularly during the recovery phase. However oleic acid injury is relatively transient and the time points utilized allowed characterisation of the effects of HTS during injury evolution and resolution.
Conclusion
In conclusion, we report for the first time that hypertonic saline enhances the resolution of oleic induced ALI. These findings further enhance the therapeutic potential of hypertonic saline in ALI/ARDS.
Abbreviations
- A-a O2 gradient:
-
Alveolar-arterial oxygen gradient
- ALI:
-
Acute Lung Injury
- ANOVA:
-
analysis of variance
- ARDS:
-
Acute Respiratory Distress Syndrome
- BAL:
-
Bronchoalveolar Lavage
- °C:
-
degrees centigrade
- ERK-1:
-
extracellular receptor kinase-1
- FiO2 :
-
Fractional inspired oxygen concentration
- g:
-
grams
- HTS:
-
Hypertonic saline
- ICAM:
-
Intercellular adhesion molecule
- IL:
-
Interleukin
- KPa:
-
KiloPascal
- MAP:
-
Mitogen activated protein
- μL:
-
microlitres
- ml.Kg-1 :
-
mililiters per kilogram
- min:
-
minutes
- OA:
-
Oleic acid
- PO2 :
-
Partial pressure of Oxygen
- SEM:
-
Standard error of the mean
- TNF-α:
-
Tumor necrosis alpha.
References
Shields CJ, Winter DC, Manning BJ, Wang JH, Kirwan WO, Redmond HP: Hypertonic saline infusion for pulmonary injury due to ischemia-reperfusion. Arch Surg. 2003, 138 (1): 9-14.
Murao Y, Loomis W, Wolf P, Hoyt DB, Junger WG: Effect of dose of hypertonic saline on its potential to prevent lung tissue damage in a mouse model of hemorrhagic shock. Shock. 2003, 20 (1): 29-34. 10.1097/01.shk.0000071060.78689.f1.
Shields CJ, Winter DC, Sookhai S, Ryan L, Kirwan WO, Redmond HP: Hypertonic saline attenuates end-organ damage in an experimental model of acute pancreatitis. Br J Surg. 2000, 87 (10): 1336-1340. 10.1046/j.1365-2168.2000.01626.x.
Machado MC, Coelho AM, Pontieri V, Sampietre SN, Molan NA, Soriano F, Matheus AS, Patzina RA, Cunha JE, Velasco IT: Local and systemic effects of hypertonic solution (NaCl 7.5%) in experimental acute pancreatitis. Pancreas. 2006, 32 (1): 80-86. 10.1097/01.mpa.0000191645.01926.8f.
Rizoli SB, Kapus A, Parodo J, Rotstein OD: Hypertonicity prevents lipopolysaccharide-stimulated CD11b/CD18 expression in human neutrophils in vitro: role for p38 inhibition. The Journal of trauma. 1999, 46 (5): 794-8; discussion 798-9.
Shields CJ, O'Sullivan AW, Wang JH, Winter DC, Kirwan WO, Redmond HP: Hypertonic saline enhances host response to bacterial challenge by augmenting receptor-independent neutrophil intracellular superoxide formation. Ann Surg. 2003, 238 (2): 249-257.
Vialet R, Albanese J, Thomachot L, Antonini F, Bourgouin A, Alliez B, Martin C: Isovolume hypertonic solutes (sodium chloride or mannitol) in the treatment of refractory posttraumatic intracranial hypertension: 2 mL/kg 7.5% saline is more effective than 2 mL/kg 20% mannitol. Crit Care Med. 2003, 31 (6): 1683-1687. 10.1097/01.CCM.0000063268.91710.DF.
Guimaraes CL, Trentin PG, Rae GA: Endothelin ET(B) receptor-mediated mechanisms involved in oleic acid-induced acute lung injury in mice. Clin Sci (Lond). 2002, 103 Suppl 48: 340S-344S.
Hussain N, Wu F, Zhu L, Thrall RS, Kresch MJ: Neutrophil apoptosis during the development and resolution of oleic acid-induced acute lung injury in the rat. Am J Respir Cell Mol Biol. 1998, 19 (6): 867-874.
Davidson KG, Bersten AD, Barr HA, Dowling KD, Nicholas TE, Doyle IR: Lung function, permeability, and surfactant composition in oleic acid-induced acute lung injury in rats. Am J Physiol Lung Cell Mol Physiol. 2000, 279 (6): L1091-102.
Weiner RE, Sasso DE, Gionfriddo MA, Thrall RS, Syrbu S, Smilowitz HM, Vento J: Early detection of oleic acid-induced lung injury in rats using (111)In-labeled anti-rat intercellular adhesion molecule-1. J Nucl Med. 2001, 42 (7): 1109-1115.
Dickey BF, Thrall RS, McCormick JR, Ward PA: Oleic-acid-induced lung injury in the rat. Failure of indomethacin treatment or complement depletion to ablate lung injury. Am J Pathol. 1981, 103 (3): 376-383.
King EG, Wagner WW, Ashbaugh DG, Latham LP, Halsey DR: Alterations in pulmonary microanatomy after fat embolism. In vivo observations via thoracic window of the oleic acid-embolized canine lung. Chest. 1971, 59 (5): 524-530. 10.1378/chest.59.5.524.
Boyd HM, Peltier LF, Scott JR, Wheeler DH: Fat embolism. II. The chemical composition of fat obtained from human long bones and subcutaneous tissue. Surgery. 1956, 40 (4): 661-664.
Van den Bergen CJ, d'Hollander AA, Malmendier CL: The chemical composition of circulating fat emboli released during total hip prosthesis. Surg Gynecol Obstet. 1976, 142 (2): 189-192.
He X, Han B, Mura M, **a S, Wang S, Ma T, Liu M, Z. L: Angiotensin-converting enzyme inhibitor captopril prevents oleic acid-induced severe acute lung injury in rats. Shock. 2007, 28 (1): 106-111. 10.1097/SHK.0b013e3180310f3a.
Young JS, Rayhrer CS, Edmisten TD, Cephas GA, Tribble CG, Kron IL: Sodium nitroprusside mitigates oleic acid-induced acute lung injury. Ann Thorac Surg. 2000, 69 (1): 224-227. 10.1016/S0003-4975(99)01130-3.
Laffey JG, Honan D, Hopkins N, Hyvelin JM, Boylan JF, McLoughlin P: Hypercapnic acidosis attenuates endotoxin-induced acute lung injury. Am J Respir Crit Care Med. 2004, 169 (1): 46-56. 10.1164/rccm.200205-394OC.
Howell K, Preston RJ, McLoughlin P: Chronic hypoxia causes angiogenesis in addition to remodelling in the adult rat pulmonary circulation. J Physiol. 2003, 547 (Pt 1): 133-145. 10.1113/jphysiol.2002.030676.
Hopkins N, Cadogan E, Giles S, McLoughlin P: Chronic airway infection leads to angiogenesis in the pulmonary circulation. J Appl Physiol. 2001, 91: 919 -9928.
Angle N, Hoyt DB, Cabello-Passini R, Herdon-Remelius C, Loomis W, Junger WG: Hypertonic saline resuscitation reduces neutrophil margination by suppressing neutrophil L selectin expression. The Journal of trauma. 1998, 45 (1): 7-12; discussion 12-3.
Rizoli SB, Kapus A, Fan J, Li YH, Marshall JC, Rotstein OD: Immunomodulatory effects of hypertonic resuscitation on the development of lung inflammation following hemorrhagic shock. J Immunol. 1998, 161 (11): 6288-6296.
Junger WG, Coimbra R, Liu FC, Herdon-Remelius C, Junger W, Junger H, Loomis W, Hoyt DB, Altman A: Hypertonic saline resuscitation: a tool to modulate immune function in trauma patients?. Shock. 1997, 8 (4): 235-241. 10.1097/00024382-199710000-00001.
Fernandes TR, Pontieri V, Moretti AI, Teixeira DO, Abatepaulo F, Soriano FG, Negri EM, Velasco IT, Souza HP: Hypertonic saline solution increases the expression of heat shock protein 70 and improves lung inflammation early after reperfusion in a rodent model of controlled hemorrhage. Shock. 2007, 27 (2): 172-178. 10.1097/01.shk.0000238062.46708.a5.
Yada-Langui MM, Anjos-Valotta EA, Sannomiya P, Rocha e Silva M, Coimbra R: Resuscitation affects microcirculatory polymorphonuclear leukocyte behavior after hemorrhagic shock: role of hypertonic saline and pentoxifylline. Exp Biol Med (Maywood). 2004, 229 (7): 684-693.
Homma H, Deitch EA, Feketeova E, Lu Q, Berezina TL, Zaets SB, Machiedo GW, Xu DZ: Small volume resuscitation with hypertonic saline is more effective in ameliorating trauma-hemorrhagic shock-induced lung injury, neutrophil activation and red blood cell dysfunction than pancreatitic protease inhibition. The Journal of trauma. 2005, 59 (2): 266-272.
Coimbra R, Hoyt DB, Junger WG, Angle N, Wolf P, Loomis W, Evers MF: Hypertonic saline resuscitation decreases susceptibility to sepsis after hemorrhagic shock. The Journal of trauma. 1997, 42 (4): 602-6; discussion 606-7.
Johnston WE, Alford PT, Prough DS, Howard G, Royster RL: Cardiopulmonary effects of hypertonic saline in canine oleic acid-induced pulmonary edema. Crit Care Med. 1985, 13 (10): 814-817. 10.1097/00003246-198510000-00008.
Pre-publication history
The pre-publication history for this paper can be accessed here:http://www.biomedcentral.com/1471-2466/8/9/prepub
Acknowledgements
This study was jointly supported by the Millennium Research Fund, NUI Galway and by the Yamanouchi European Research Foundation. Dr Higgins is a research fellow supported by funding from the Yamanouchi European Research Foundation and Health Research Board [Ireland]. The funding agencies played no role in study design, in the collection, analysis, and interpretation of data, in the writing of the manuscript, or in the decision to submit the manuscript for publication.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
The authors declare that they have no competing interests.
Authors' contributions
MTK conceived of the study, and participated in its design and execution and helped to draft the manuscript. BDH participated in the study execution and the histologic analysis, and helped to draft the manuscript. JFC participated in the histologic analysis and helped to draft the manuscript. JGL participated in the design and coordination of the study, performed the statistical analysis, and helped to draft the manuscript. All authors read and approved the final manuscript.
Muiris T Kennedy, Brendan D Higgins contributed equally to this work.
Authors’ original submitted files for images
Below are the links to the authors’ original submitted files for images.
Rights and permissions
Open Access This article is published under license to BioMed Central Ltd. This is an Open Access article is distributed under the terms of the Creative Commons Attribution License ( https://creativecommons.org/licenses/by/2.0 ), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
About this article
Cite this article
Kennedy, M.T., Higgins, B.D., Costello, J.F. et al. Hypertonic saline reduces inflammation and enhances the resolution of oleic acid induced acute lung injury. BMC Pulm Med 8, 9 (2008). https://doi.org/10.1186/1471-2466-8-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/1471-2466-8-9