Abstract
Background
Cancer serum protein profiling by mass spectrometry has uncovered mass profiles that are potentially diagnostic for several common types of cancer. However, direct mass spectrometric profiling has a limited dynamic range and difficulties in providing the identification of the distinctive proteins. We hypothesized that distinctive profiles may result from the differential expression of relatively abundant serum proteins associated with the host response.
Methods
Eighty-four antibodies, targeting a wide range of serum proteins, were spotted onto nitrocellulose-coated microscope slides. The abundances of the corresponding proteins were measured in 80 serum samples, from 24 newly diagnosed subjects with lung cancer, 24 healthy controls, and 32 subjects with chronic obstructive pulmonary disease (COPD). Two-color rolling-circle amplification was used to measure protein abundance.
Results
Seven of the 84 antibodies gave a significant difference (p < 0.01) for the lung cancer patients as compared to healthy controls, as well as compared to COPD patients. Proteins that exhibited higher abundances in the lung cancer samples relative to the control samples included C-reactive protein (CRP; a 13.3 fold increase), serum amyloid A (SAA; a 2.0 fold increase), mucin 1 and α-1-antitrypsin (1.4 fold increases). The increased expression levels of CRP and SAA were validated by Western blot analysis. Leave-one-out cross-validation was used to construct Diagonal Linear Discriminant Analysis (DLDA) classifiers. At a cutoff where all 56 of the non-tumor samples were correctly classified, 15/24 lung tumor patient sera were correctly classified.
Conclusion
Our results suggest that a distinctive serum protein profile involving abundant proteins may be observed in lung cancer patients relative to healthy subjects or patients with chronic disease and may have utility as part of strategies for detecting lung cancer.
Similar content being viewed by others
Background
Lung cancer remains the leading cause of cancer mortality in the United States for both men and women [1, 2]. Despite significant advances in understanding its biology and causes, the overall incidence of lung cancer is increasing, and improvements in outcome are not apparent [3]. As treatment is efficacious only for those patients who are diagnosed sufficiently early in the disease process, a significant reduction in patient mortality may result from earlier detection of lung cancer, including combinations of biomarkers with spiral CT imaging [2].
Identification of protein biomarkers in blood or serum may have utility for noninvasive disease detection and classification. Biomarker identification would be greatly enhanced by methodological improvements in protein detection. Direct serum protein profiling by matrix assisted laser desorption ionization (MALDI) mass spectrometry [22]. We took the negative of the base-2 logarithm of the "median of ratios" computed by the software, and averaged the triplicate measures for each bait, not including the excluded dots. This gave the average of the log-ratio of the sample (Cy3) to the standard pool (Cy5), hereafter referred to as the values.
We first performed a normalization in which the median value for each array was subtracted from all the values for that sample. Some antibodies displayed biases in favor of either the Cy3 or Cy5 channel, or showed large differences between groups. Consequently, we selected a subset of 48 antibodies that did not have large differences between groups, and had small within-group standard deviations in order to perform a normalization that would be less affected by antibodies with variable data or channel biases. We computed the average of the raw values for each antibody using the 80 arrays, and normalized the individual slides to this standard. For each slide, the median of the 48 differences for the array minus the corresponding values on the standard was subtracted from the array, subtraction being used rather than division because the values were already log-transformed. The averaged raw and normalized data are available as supplemental information [22].
Western blot analysis
We used Western blots to analyze the level of C-reactive protein (CRP) and serum-amyloid A (SAA) in sera of eight selected lung cancer patients and eight healthy controls. Subsequently, in order to validate our findings, we also analyzed the CRP and SAA levels in an independent set of 30 additional lung cancer patients and 30 additional healthy controls. Briefly, 5 μl of serum (from each patient) was resolved by 15% SDS-PAGE, and then transferred to a PVDF membrane. Following incubation in blocking buffer (PBST0.1 containing 2% nonfat dry milk (Bio-Rad)) for 2 h, the membrane was hybridized in blocking buffer containing either anti-CRP or anti-SAA mouse monoclonal antibodies at 0.5 μg/ml and 0.25 μg/ml for 1 h. The membrane was then washed and incubated with a horseradish peroxidase-conjugated sheep anti-mouse IgG (Amersham) at a 1:1000 dilution for 1 h. After washing, the membrane was briefly incubated in ECL (Enhanced Chemiluminescence, Amersham), then exposed to imaging film (Amersham). Integrated intensity measurements were made of the respective bands and the measurements were further analyzed statistically.
Results
Using microarrays containing 84 antibodies printed in triplicate on slides, we measured the amount of target protein bound from 80 individual sera, with each sample being compared to a pooled reference sample (consisting of a mixture of all of the sera) in a two-color assay. Figure 1 shows a representative image of antibody arrays from one slide. Eighty arrays with 24 sera from lung cancer patients, 24 normal sera, or 32 sera from patients with COPD were analyzed. The values determined were the normalized average of base-2 logarithms of the intensity arising from the individual sample divided by the intensity arising from the pooled sample, which was measured as Cy3 and Cy5 fluorescence, respectively. Values from triplicate antibody dots from the same array were quite reproducible, with average standard deviations of 0.14, corresponding to approximately 10% variation in the ratios.
Scanned fluorescence image of an antibody microarray detected by two-color RCA. 96 baits including 84 antibodies were spotted onto microscope slides coated with nitrocellulose. 12 identical arrays were printed on each of seven slides. Each antibody was printed in triplicate on each array in order to form an 18 by 16 array of dots. A test sample labeled with biotin and a pooled reference sample labeled with digoxigenin were co-incubated on the microarray, and bound proteins from both samples were detected by RCA. The microarray was scanned for Cy3 fluorescence (from the test sample) and Cy5 fluorescence (from the reference sample).
Figure 2 depicts the first three principal components obtained using all 84 antibodies. While lung cancer patients were largely separated from the other two groups of patients, there was no clear separation between COPD and normal. This completely unsupervised view of the data indicates that the distinction between lung tumor patients' sera and the two other groups of sera was likely the largest source of variation in the data set (Figure 2A). The somewhat outlying samples were not associated with a particular microarray slide (Figure 2B) or brightness of the signals for either fluorescence. The first principal component was most highly correlated with C-reactive protein (CRP) and serum amyloid A (SAA).
The first 3 principal components from normalized log-base-2 ratios of sample to reference pool intensities, using all 84 antibodies. The full 3-dimensional figures that can be rotated are available in the supplementary materials. In A, normal, COPD and lung cancer patients are marked with yellow, blue and red, respectively. The first three principal components account for 43% of the variance. In B, seven slides are marked separately with blue, black, yellow, green, purple, brown and red.
In order to determine which antibodies distinguished sera of lung tumor patients from the other sera, we fit a 1-way analysis of variance model to the three groups of samples. Cancer patient sera gave significantly different mean values for 7/84 antibodies when compared to normal sera, and for 8/84 of the antibodies when compared to the COPD sera (both at p < 0.01). The 7 antibodies that yielded differences in the abundance of their corresponding proteins between tumor and normal sera were common to the group of 8 antibodies that yielded differences in the abundance of their corresponding proteins between tumor and COPD sera. The additional protein identified by the COPD comparison is troponin 1. We found increased levels of CRP, SAA, α-1-antitrypsin (AAT) by two distinct antibodies, and MUC1, and decreased levels of transferrin and gelsolin, in lung cancer sera (Table 1). Results obtained for the entire set of antibodies are available as supplemental data [22]. To assess the significance of these findings, we randomly permutated the sample labels 1000 times and performed the identical analysis on each resulting data set. On average this yielded only 0.1 antibodies for which the tumor samples were increased or decreased (at p < 0.1) compared to both other groups, with 1 or more significant antibody found in only 8.1% of the permuted data sets. Therefore, it is very unlikely that the occurrence of differences in levels of proteins for the 7 antibodies observed in the actual data is due to chance. The correlation within the group of lung cancer patients between the CRP, SAA, AAT, MUC1, transferrin and gelsolin data values are summarized in Table 2, and the two-dimensional log-scale plots for CRP and MUC1, and SAA and AAT are shown in Figure 3. The expression levels of CRP, SAA and AAT but not MUC1 were correlated with each other (r > 0.4, p < 0.05). The two AAT measurements, each derived from a different antibody, were significantly correlated (r = 0.72, p < 0.001).
We performed a leave-one-out validation of a Diagonal Linear Discriminant Analysis (DLDA) classifier that discriminates tumor vs. non-tumor samples [23]. We left out one sample at a time, then used the remaining 79 samples to select the 5 antibodies with values increased in tumor patient samples according to the p-values for 2-sample T-tests of tumor vs. non-tumor samples, and constructed the resulting discriminant function based on the 79 samples. When using all of the data CRP, SAA, MUC1, and 2 AAT antibodies would be selected as the top antibodies, in that order. The value of this function was then computed for the left out sample. Figure 4 shows the resulting Receiver Operating Characteristic (ROC) curve that was obtained. The calculations were also repeated using only the best 3 antibodies. Using 5 antibodies, the correct classification of all 56 of the non-tumor samples was associated with the correct classification of 15 of 24 cancer patient sera. We obtained the same result with a different classifier that used majority voting among the 5 closest neighboring samples, where the distances were computed after scaling each antibody's values by the pooled estimate of the standard deviation (in analogy to DLDA). Analogous results from cross-validating this simpler classifier using only the 3 best antibodies correctly classified 17 of 24 cancer patient sera, while misclassifiying 4 of 56 non-tumor samples, which also corresponds approximately to a point on the ROC curve for the DLDA classifier when it used 3 antibodies. This illustrates that the results obtained with DLDA classifiers were not particularly better than could be obtained with other simple methods.
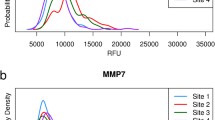
CRP and SAA were selected for Western blot analysis in order to validate the specificity of antibody microarrays. Eight lung cancer sera and 8 normal sera were resolved by SDS-PAGE, then transferred to PVDF membranes. The membranes were probed with anti-CRP or anti-SAA antibodies. As shown in Figure 5, all of the sera from patients with lung cancer showed much higher levels of CRP and SAA compared to the sera from healthy controls. Subsequently, in order to validate our findings, we also analyzed the CRP and SAA levels in an independent set of 30 additional lung cancer patients and 30 additional healthy controls. Integrated intensity measurements were made of the respective bands and the measurements were further analyzed statistically. The distribution of integrated intensity measurement values obtained from the two groups of samples for both assays are shown in Figure 6. The number of tumor samples with values greater than the largest value for normal samples was 17/30 for CRP (p = 3.1 × 10-7) and 13/30 for SAA (p = 2.3 × 10-5).
A scatter plot of integrated intensity measurements derived from western blots of an independent set of sera from 30 additional lung cancer patients and 30 additional healthy controls, probed for SAA and CRP. Values are base two logarithms of the relative band intensities after adding 0.1 to each value (to force values to be greater than 0).
Discussion
Four proteins were found to be more abundant in the lung cancer samples than those of the controls, namely CRP (13.3 fold), SAA (2.0 fold), AAT (1.4 fold) and MUC1 (1.4 fold). There were no significant protein expression differences observed in serum between the various lung cancer subtypes examined (adenocarcinoma, squamous and small cell carcinomas: data not shown). The significant increases in CRP and SAA protein levels found in the serum of lung cancer patients by protein microarray were confirmed by immunoassay. The increased levels of AAT in lung cancer patient sera (1.4 fold) were observed using two different antibodies, each obtained from a separate source.
The pattern of increased abundances of CRP, SAA, AAT and MUC1 in lung cancer patient sera that were observed in our microarray-based study is concordant with previous studies of individual proteins. An increased C-reactive protein level is part of the acute-phase response to most forms of inflammation, infection, tissue damage, and malignant neoplasia [25–27]. CRP [Uniprot PO2741] forms homopentamers (pentaxins); it promotes phagocytosis and complement fixation through calcium-dependent binding (two per 23 kDa subunit) to phosphorylcholine. CRP also interacts with DNA and histones to scavenge nuclear material from damaged circulating cells. The expression of CRP is induced by IL-1 and IL-6. While CRP itself is likely not useful as a single assay, it may have clinical utility as part of a panel of diagnostic biomarkers, especially in evaluating results from spiral CT imaging [2]. CRP is mainly expressed in hepatocytes; cytokines, especially interleukin-6, induce the expression and release of CRP [28, 29]. CRP has been suggested as a useful prognostic indicator in esophageal carcinoma [30]. Studies also showed that CRP was an independent determinant of survival in non-small-cell lung cancer [31] and could be useful in the initial evaluation of patients with small cell lung cancer and in monitoring response to therapy [32].
Serum amyloid A [Uniprot PO2735] is an acute-phase protein that occurs in various isoforms in a molecular mass range of 11–14 kDa. SAA is produced by hepatocytes [33], secreted into serum and rapidly binds to high-density lipoprotein, with 90% occurring in the bound form [34]. SAA occurs at low levels in sera of healthy individuals [35]. Patients with neoplastic disease, including lung [36], renal [37], colorectal [38], prostate [39] and nasopharyngeal cancers [40] exhibit a dramatic elevation of serum SAA. However, SAA is not a cancer-specific marker per se. Its elevation in serum has been reported also in association with trauma, infection, inflammation, rheumatoid arthritis, and amyloidosis [41]. A study of 621 subjects with cancer found substantial increases of SAA levels in >95% (281 of 289) of patients with metastatic solid tumors, all myelocytic leukemia patients and all advanced lymphoma patients [42]. Interestingly, SAA was not elevated in the group of 32 COPD patients included in this study, suggesting a potential utility of SAA in distinguishing between the two conditions possibly due to a different cytokine profile between the two groups.
α-1-antitrypsin [A1AT/SERPINA1, Uniprot PO1009] is a secretory glycoprotein of molecular weight 44 kDa produced in the liver. It neutralizes the effects of proteases in several organ systems, mainly in the lung. The major physiological role of AAT in the lung is to bind and inhibit elastase released from leucocytes in the lower respiratory tract, thereby preventing the destruction of lung tissue [43, 44]. The normal range of serum or plasma AAT concentrations is 1200–2000 mg/L, with large increases in inflammatory conditions, infections, cancer, liver disease, or pregnancy [43]. It was previously reported that the serum concentration of AAT increased with tumor growth and could be utilized following tumor resection as an indicator of relapse [45, 46]. The prognostic significance of AAT expression in lung adenocarcinomas has been evaluated using immunohistochemistry [47]; strongly AAT-positive cases had a worse prognosis than weak-to-moderately AAT-positive or AAT-negative cases, suggesting that increased AAT expression in lung adenocarcinoma patients may be a prognostic indicator. The biological basis for the association of acute-phase proteins, including CRP, SAA, and AAT, with lung cancer remains largely unknown. The correlation between CRP, SAA, and AAT levels was significant (r > 0.4), likely reflecting a host response. Significantly higher levels occur in patients with metastatic disease compared to patients with limited disease [48].
We found serum MUC1 levels to be modestly elevated in lung cancer compared to controls. MUC1 [P15941] is a membrane-bound mucin of 122 kDa molecular weight with several interacting isozymes, polymorphic tandem repeats, and an extensively O-glycosylated core protein [49]. In vitro studies suggested that MUC1 reduces E-cadherin-mediated cell-cell adhesion by steric hindrance, which increases metastatic ability [50]. High MUC1 levels also reduces the integrin-mediated cell adhesion to the extracellular matrix [51]. The clinical importance of the MUC1 glycoprotein, however, is not clear. Previous studies have reported that MUC1 was developmentally regulated and aberrantly expressed by carcinomas, and a high level of MUC1 mRNA expression in adenocarcinoma has been associated with poor prognosis [52–58]. MUC1 was also found to be up-regulated in non-small-cell lung cancer [59–61]. MUC1 is shed into the blood stream and thus has a potential as a tumor marker, as demonstrated in breast cancer [62–64]. Consistent with this finding, we observed higher MUC1 expression levels in the sera of lung cancer patients than in either healthy subjects or patients with COPD. Additionally, MUC1 expression levels did not show significant correlation with CRP, SAA, or AAT, suggesting that the increased MUC1 levels might be due to a different biological process. Interestingly, MUC1 serum levels in breast cancer patients were not concordant with the levels observed in tumor tissues by immunohistochemistry [64, 65], so the increased serum MUC1 expression may correspond to a specific isoform expressed by cancer cells. Thus, expression levels of the different MUC1 isoforms and their epitopes may need to be evaluated to fully explain the increased levels in serum of lung cancer patients.
Other acute-phase reactant serum proteins that have been reported as significantly elevated in certain cancers were not increased in this study of sera from lung cancer patients. Most notably, the alpha sub-unit of haptoglobin (MW 11.7 kDa) and isoforms of the haptoglobin-1 precursor (HAP1) have been reported to be increased in serum of patients with ovarian and other gynecologic cancers [66, 67].
Conclusion
Our results suggest that a distinctive serum protein profile involving relatively abundant proteins may be observed in cancer patients relative to healthy subjects or patients with chronic disease. It is therefore likely that distinctive mass peak profiles observed by mass spectrometry in cancer sera relative to control and that may be predictive of outcome include a significant component related to host response to tumors and acute phase reactants. The extent to which such indicators of host response have clinical utility as a group, together with other tumor biomarkers remains to be determined. The use of antibody microarrays directed against a broad range of serum and lung tumor proteins would have utility for elucidating those proteins with the greatest diagnostic utility.
References
Society, AC Cancer Facts and Figures 2004. Atlanta, GA. 2004
Omenn GS: Human lung cancer chemoprevention strategies: Parker B. Francis Lecture. Chest. 2004, 125 (5 Suppl): 123S-127S. 10.1378/chest.125.5_suppl.123S.
Carbone DP: The biology of lung cancer. Semin Oncol. 1997, 24 (4): 388-401.
**ao X, Liu D, Tang Y, Guo F, **a L, Liu J, He D: Development of proteomic patterns for detecting lung cancer. Dis Markers. 2003, 19 (1): 33-39.
Zhukov TA, Johanson RA, Cantor AB, Clark RA, Tockman MS: Discovery of distinct protein profiles specific for lung tumors and pre-malignant lung lesions by SELDI mass spectrometry. Lung Cancer. 2003, 40 (3): 267-279.
Knezevic V, Leethanakul C, Bichsel VE, Worth JM, Prabhu VV, Gutkind JS, Liotta LA, Munson PJ, Petricoin EF, Krizman DB: Proteomic profiling of the cancer microenvironment by antibody arrays. Proteomics. 2001, 1 (10): 1271-1278. 10.1002/1615-9861(200110)1:10<1271::AID-PROT1271>3.3.CO;2-Y.
Sreekumar A, Nyati MK, Varambally S, Barrette TR, Ghosh D, Lawrence TS, Chinnaiyan AM: Profiling of cancer cells using protein microarrays: discovery of novel radiation-regulated proteins. Cancer Res. 2001, 61 (20): 7585-7593.
Joos TO, Schrenk M, Hopfl P, Kroger K, Chowdhury U, Stoll D, Schorner D, Durr M, Herick K, Rupp S, Sohn K, Hammerle H: A microarray enzyme-linked immunosorbent assay for autoimmune diagnostics. Electrophoresis. 2000, 21 (13): 2641-2650. 10.1002/1522-2683(20000701)21:13<2641::AID-ELPS2641>3.0.CO;2-5.
MacBeath G, Schreiber SL: Printing proteins as microarrays for high-throughput function determination. Science. 2000, 289 (5485): 1760-1763.
Ge H: UPA, a universal protein array system for quantitative detection of protein-protein, protein-DNA, protein-RNA and protein-ligand interactions. Nucleic Acids Res. 2000, 28 (2): e3-10.1093/nar/28.2.e3.
Lueking A, Horn M, Eickhoff H, Bussow K, Lehrach H, Walter G: Protein microarrays for gene expression and antibody screening. Anal Biochem. 1999, 270 (1): 103-111. 10.1006/abio.1999.4063.
Zhu H, Bilgin M, Bangham R, Hall D, Casamayor A, Bertone P, Lan N, Jansen R, Bidlingmaier S, Houfek T, Mitchell T, Miller P, Dean RA, Gerstein M, Snyder M: Global analysis of protein activities using proteome chips. Science. 2001, 293 (5537): 2101-2105. 10.1126/science.1062191.
Haab BB, Dunham MJ, Brown PO: Protein microarrays for highly parallel detection and quantitation of specific proteins and antibodies in complex solutions. Genome Biol. 2001, 2 (2): RESEARCH0004-10.1186/gb-2001-2-2-research0004.
Mendoza LG, McQuary P, Mongan A, Gangadharan R, Brignac S, Eggers M: High-throughput microarray-based enzyme-linked immunosorbent assay (ELISA). Biotechniques. 1999, 27 (4): 778-780. 782–776,788.
de Wildt RM, Mundy CR, Gorick BD, Tomlinson IM: Antibody arrays for high-throughput screening of antibody-antigen interactions. Nat Biotechnol. 2000, 18 (9): 989-994. 10.1038/79494.
Arenkov P, Kukhtin A, Gemmell A, Voloshchuk S, Chupeeva V, Mirzabekov A: Protein microchips: use for immunoassay and enzymatic reactions. Anal Biochem. 2000, 278 (2): 123-131. 10.1006/abio.1999.4363.
Huang RP, Huang R, Fan Y, Lin Y: Simultaneous detection of multiple cytokines from conditioned media and patient's sera by an antibody-based protein array system. Anal Biochem. 2001, 294 (1): 55-62. 10.1006/abio.2001.5156.
Haab BB: Methods and applications of antibody microarrays in cancer research. Proteomics. 2003, 3 (11): 2116-2122. 10.1002/pmic.200300595.
Haab BB, Zhou H: Multiplexed protein analysis using spotted antibody microarrays. Methods Mol Biol. 2004, 264: 33-45.
Zhou H, Bouwman K, Schotanus M, Verweij C, Marrero JA, Dillon D, Costa J, Lizardi P, Haab BB: Two-color, rolling-circle amplification on antibody microarrays for sensitive, multiplexed serum-protein measurements. Genome Biol. 2004, 5 (4): R28-10.1186/gb-2004-5-4-r28.
Schweitzer B, Wiltshire S, Lambert J, O'Malley S, Kukanskis K, Zhu Z, Kingsmore SF, Lizardi PM, Ward DC: Inaugural article: immunoassays with rolling circle DNA amplification: a versatile platform for ultrasensitive antigen detection. Proc Natl Acad Sci U S A. 2000, 97 (18): 10113-10119. 10.1073/pnas.170237197.
Detailed antibody, patient serum and experimental information. [http://dot.ped.med.umich.edu:2000/pub/AbMicro/index.htm]
Miller JC, Zhou H, Kwekel J, Cavallo R, Burke J, Butler EB, Teh BS, Haab BB: Antibody microarray profiling of human prostate cancer sera: antibody screening and identification of potential biomarkers. Proteomics. 2003, 3 (1): 56-63. 10.1002/pmic.200390009.
Dudoit S, Fridlyand J, Speed TP: Comparison of discrimination methods for the classification of tumors using gene expression data. Journal of the American Statistical Association. 2002, 97: 77-87. 10.1198/016214502753479248.
Pepys MB, Hirschfield GM: C-reactive protein: a critical update. J Clin Invest. 2003, 111 (12): 1805-1812. 10.1172/JCI200318921.
Danesh J, Wheeler JG, Hirschfield GM, Eda S, Eiriksdottir G, Rumley A, Lowe GD, Pepys MB, Gudnason V: C-reactive protein and other circulating markers of inflammation in the prediction of coronary heart disease. N Engl J Med. 2004, 350 (14): 1387-1397. 10.1056/NEJMoa032804.
Tall AR: C-reactive protein reassessed. N Engl J Med. 2004, 350 (14): 1450-1452. 10.1056/NEJMe048020.
McKeown DJ, Brown DJ, Kelly A, Wallace AM, McMillan DC: The relationship between circulating concentrations of C-reactive protein, inflammatory cytokines and cytokine receptors in patients with non-small-cell lung cancer. Brit J Cancer. 2004, 91: 1993-1995. 10.1038/sj.bjc.6602248.
Scott HR, McMillan DC, Crilly A, McArdle CS, Milroy R: The relationship between weight loss and interleukin 6 in non-small-cell lung cancer. Brit J Cancer. 1996, 73 (12): 1560-1562.
Nozoe T, Saeki H, Sugimachi K: Significance of preoperative elevation of serum C-reactive protein as an indicator of prognosis in esophageal carcinoma. Am J Surg. 2001, 182 (2): 197-201. 10.1016/S0002-9610(01)00684-5.
Kato K, Hitsuda Y, Kawasaki Y, Igishi T, Yasuda K, Mikami M, Watanabe M, Miyata M, Sasaki T, Shimizu E: [The value of serum C-reactive protein as a survival determinant in patients with advanced non-small-cell lung cancer]. Nihon Kokyuki Gakkai Zasshi. 2000, 38 (8): 575-580.
Arpin D, Trillet-Lenoir V, Lasset C, Souquet PJ, Riou R, Yoanidis I, Guidollet J, Cordier JF, Brune J: [Value of C-reactive protein determination in small cell lung cancer]. Bull Cancer. 1993, 80 (12): 1063-1068.
Raynes JG, Eagling S, McAdam KP: Acute-phase protein synthesis in human hepatoma cells: differential regulation of serum amyloid A (SAA) and haptoglobin by interleukin-1 and interleukin-6. Clin Exp Immunol. 1991, 83 (3): 488-491.
Bausserman LL, Herbert PN, Rodger R, Nicolosi RJ: Rapid clearance of serum amyloid A from high-density lipoproteins. Biochim Biophys Acta. 1984, 792 (2): 186-191.
d'Eril GM, Anesi A, Maggiore M, Leoni V: Biological variation of serum amyloid A in healthy subjects. Clin Chem. 2001, 47 (8): 1498-1499.
Biran H, Friedman N, Neumann L, Pras M, Shainkin-Kestenbaum R: Serum amyloid A (SAA) variations in patients with cancer: correlation with disease activity, stage, primary site, and prognosis. J Clin Pathol. 1986, 39 (7): 794-797.
Kimura M, Tomita Y, Imai T, Saito T, Katagiri A, Ohara-Mikami Y, Matsudo T, Takahashi K: Significance of serum amyloid A on the prognosis in patients with renal cell carcinoma. Cancer. 2001, 92 (8): 2072-2075. 10.1002/1097-0142(20011015)92:8<2072::AID-CNCR1547>3.0.CO;2-P.
Glojnaric I, Casl MT, Simic D, Lukac J: Serum amyloid A protein (SAA) in colorectal carcinoma. Clin Chem Lab Med. 2001, 39 (2): 129-133. 10.1515/CCLM.2001.022.
Kaneti J, Winikoff Y, Zimlichman S, Shainkin-Kestenbaum R: Importance of serum amyloid A (SAA) level in monitoring disease activity and response to therapy in patients with prostate cancer. Urol Res. 1984, 12 (5): 239-241. 10.1007/BF00256147.
Cho WC, Yip TT, Yip C, Yip V, Thulasiraman V, Ngan RK, Yip TT, Lau WH, Au JS, Law SC, Cheng WW, Ma VW, Lim CK: Identification of serum amyloid a protein as a potentially useful biomarker to monitor relapse of nasopharyngeal cancer by serum proteomic profiling. Clin Cancer Res. 2004, 10 (1 Pt 1): 43-52.
Benson MD, Cohen AS: Serum amyloid A protein in amyloidosis, rheumatic, and enoplastic diseases. Arthritis Rheum. 1979, 22 (1): 36-42.
Rosenthal CJ, Sullivan LM: Serum amyloid A to monitor cancer dissemination. Ann Intern Med. 1979, 91 (3): 383-390.
Crystal RG: The alpha 1-antitrypsin gene and its deficiency states. Trends Genet. 1989, 5 (12): 411-417. 10.1016/0168-9525(89)90200-X.
Sun Z, Yang P: Role of imbalance between neutrophil elastase and alpha 1-antitrypsin in cancer development and progression. Lancet Oncol. 2004, 5 (3): 182-190. 10.1016/S1470-2045(04)01414-7.
Homolka J, Voslarova Z, Malbohan I: [Significance of alpha-1-antitrypsin and alpha-2-pregnancy-associated glycoprotein in the serum of patients with bronchial carcinoma]. Z Erkr Atmungsorgane. 1987, 169 (1): 38-43.
Di Martino G, Iannucci F, Bizzarro A, Iacono G: [Association of serum tumor markers in solid neoplasms (CEA, ferritin, alpha 1-antitrypsin, parathormone and calcitonin)]. Boll Ist Sieroter Milan. 1982, 61 (5): 411-422.
Higashiyama M, Doi O, Kodama K, Yokouchi H, Tateishi R: An evaluation of the prognostic significance of alpha-1-antitrypsin expression in adenocarcinomas of the lung: an immunohistochemical analysis. Br J Cancer. 1992, 65 (2): 300-302.
Weinstein PS, Skinner M, Sipe JD, Lokich JJ, Zamcheck N, Cohen AS: Acute-phase proteins or tumour markers: the role of SAA, SAP, CRP and CEA as indicators of metastasis in a broad spectrum of neoplastic diseases. Scand J Immunol. 1984, 19 (3): 193-198.
Gendler SJ, Spicer AP: Epithelial mucin genes. Annu Rev Physiol. 1995, 57: 607-634. 10.1146/annurev.ph.57.030195.003135.
Wesseling J, van der Valk SW, Hilkens J: A mechanism for inhibition of E-cadherin-mediated cell-cell adhesion by the membrane-associated mucin episialin/MUC1. Mol Biol Cell. 1996, 7 (4): 565-577.
Wesseling J, van der Valk SW, Vos HL, Sonnenberg A, Hilkens J: Episialin (MUC1) overexpression inhibits integrin-mediated cell adhesion to extracellular matrix components. J Cell Biol. 1995, 129 (1): 255-265. 10.1083/jcb.129.1.255.
Wolman SR, Pauley RJ, Mohamed AN, Dawson PJ, Visscher DW, Sarkar FH: Genetic markers as prognostic indicators in breast cancer. Cancer. 1992, 70 (6 Suppl): 1765-1774.
Sasaki M, Nakanuma Y, Shimizu K, Izumi R: Pathological and immunohistochemical findings in a case of mucinous cholangiocarcinoma. Pathol Int. 1995, 45 (10): 781-786.
Ajioka Y, Allison LJ, Jass JR: Significance of MUC1 and MUC2 mucin expression in colorectal cancer. J Clin Pathol. 1996, 49 (7): 560-564.
McGuckin MA, Walsh MD, Hohn BG, Ward BG, Wright RG: Prognostic significance of MUC1 epithelial mucin expression in breast cancer. Hum Pathol. 1995, 26 (4): 432-439. 10.1016/0046-8177(95)90146-9.
Nakamori S, Ota DM, Cleary KR, Shirotani K, Irimura T: MUC1 mucin expression as a marker of progression and metastasis of human colorectal carcinoma. Gastroenterology. 1994, 106 (2): 353-361.
Gendler SJ, Lancaster CA, Taylor-Papadimitriou J, Duhig T, Peat N, Burchell J, Pemberton L, Lalani EN, Wilson D: Molecular cloning and expression of human tumor-associated polymorphic epithelial mucin. J Biol Chem. 1990, 265 (25): 15286-15293.
Ohgami A, Tsuda T, Osaki T, Mitsudomi T, Morimoto Y, Higashi T, Yasumoto K: MUC1 mucin mRNA expression in stage I lung adenocarcinoma and its association with early recurrence. Ann Thorac Surg. 1999, 67 (3): 810-814. 10.1016/S0003-4975(99)00041-7.
Nguyen PL, Niehans GA, Cherwitz DL, Kim YS, Ho SB: Membrane-bound (MUC1) and secretory (MUC2, MUC3, and MUC4) mucin gene expression in human lung cancer. Tumour Biol. 1996, 17 (3): 176-192.
Guddo F, Giatromanolaki A, Koukourakis MI, Reina C, Vignola AM, Chlouverakis G, Hilkens J, Gatter KC, Harris AL, Bonsignore G: MUC1 (episialin) expression in non-small cell lung cancer is independent of EGFR and c-erbB-2 expression and correlates with poor survival in node positive patients. J Clin Pathol. 1998, 51 (9): 667-671.
Ho SB, Niehans GA, Lyftogt C, Yan PS, Cherwitz DL, Gum ET, Dahiya R, Kim YS: Heterogeneity of mucin gene expression in normal and neoplastic tissues. Cancer Res. 1993, 53 (3): 641-651.
Devine PL, McGuckin MA, Ramm LE, Ward BG, Pee D, Long S: Serum mucin antigens CASA and MSA in tumors of the breast, ovary, lung, pancreas, bladder, colon, and prostate. A blind trial with 420 patients. Cancer. 1993, 72 (6): 2007-2015.
Hayes DF, Sekine H, Ohno T, Abe M, Keefe K, Kufe DW: Use of a murine monoclonal antibody for detection of circulating plasma DF3 antigen levels in breast cancer patients. J Clin Invest. 1985, 75 (5): 1671-1678.
Croce MV, Isla-Larrain MT, Demichelis SO, Gori JR, Price MR, Segal-Eiras A: Tissue and serum MUC1 mucin detection in breast cancer patients. Breast Cancer Res Treat. 2003, 81 (3): 195-207. 10.1023/A:1026110417294.
Cannon PM, Ellis IO, Blamey RW, Bell J, Elston CW, Robertson JF: Expression of tumour-associated antigens in breast cancer primary tissue compared with serum levels. Eur J Surg Oncol. 1993, 19 (6): 523-527.
Ahmed N, Barker G, Oliva KT, Hoffmann P, Riley C, Reeve S, Smith AI, Kemp BE, Quinn MA, Rice GE: Proteomic-based identification of haptoglobin-1 precursor as a novel circulating biomarker of ovarian cancer. Brit J Cancer. 2004, 91: 129-140. 10.1038/sj.bjc.6601882.
Ye B, Cramer DW, Skates SJ, Gygi SP, Pratomo V, Fu L, Horick NK, Licklider LJ, Schorge JO, Berkowitz RS, Mok SC: Haptoglobin-alpha subunit as potential serum biomarker in ovarian cancer: identification and characterization using proteomic profiling and mass spectrometry. Clin Cancer Res. 2003, 9: 2904-2911.
Pre-publication history
The pre-publication history for this paper can be accessed here:http://www.biomedcentral.com/1471-2407/5/110/prepub
Acknowledgements
This work was supported by grant MTTC GR356.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
The author(s) declare that they have no competing interests.
Authors' contributions
W-MG carried out the antibody microarray studies, participated in the statistical treatment of the data and drafted the manuscript. RK performed the statistical analysis of the data and in drafting the manuscript. RPO participated in the antibody microarray studies. DEM participated in the design of the study, helped coordinate serum acquisition/usage and in drafting the manuscript. JQ carried out the independent validation of CRP and SAA quantitation. AKG and WNR participated in the acquisition of the COPD serum. DEB participated in the acquisition of both the normal and control serum. GSO participated in the design of the study and helped to draft the manuscript. BBH participated in the design of the study and its coordination, and helped to draft the manuscript. SMH conceived of the study, participated in its design, and helped to draft the manuscript. All authors read and approved the final manuscript.
Authors’ original submitted files for images
Below are the links to the authors’ original submitted files for images.
Rights and permissions
Open Access This article is published under license to BioMed Central Ltd. This is an Open Access article is distributed under the terms of the Creative Commons Attribution License ( https://creativecommons.org/licenses/by/2.0 ), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
About this article
Cite this article
Gao, WM., Kuick, R., Orchekowski, R.P. et al. Distinctive serum protein profiles involving abundant proteins in lung cancer patients based upon antibody microarray analysis. BMC Cancer 5, 110 (2005). https://doi.org/10.1186/1471-2407-5-110
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/1471-2407-5-110