Abstract
Background
Vitamin A (VA) deficiency induces a type 1 cytokine response and exogenously provided retinoids can induce a type 2 cytokine response both in vitro and in vivo. The precise mechanism(s) involved in this phenotypic switch are inconsistent and have been poorly characterized in humans. In an effort to determine if retinoids are capable of inducing Th2 cytokine responses in human T cell cultures, we stimulated human PBMCs with immobilized anti-CD3 mAb in the presence or absence of all-trans retinoic acid (ATRA) or 9-cis-RA.
Results
Stimulation of human PBMCs and purified T cells with ATRA and 9-cis-RA increased mRNA and protein levels of IL-4, IL-5, and IL-13 and decreased levels of IFN-γ, IL-2, IL-12p70 and TNF-α upon activation with anti-CD3 and/or anti-CD28 mAbs. These effects were dose-dependent and evident as early as 12 hr post stimulation. Real time RT-PCR analysis revealed a dampened expression of the Th1-associated gene, T-bet, and a time-dependent increase in the mRNA for the Th2-associated genes, GATA-3, c-MAF and STAT6, upon treatment with ATRA. Besides Th1 and Th2 cytokines, a number of additional proinflammatory and regulatory cytokines including several chemokines were also differentially regulated by ATRA treatment.
Conclusion
These data provide strong evidence for multiple inductive roles for retinoids in the development of human type-2 cytokine responses.
Similar content being viewed by others
Background
An uncommitted precursor T helper (pTh) cell can be induced to differentiate into at least two distinct subsets of effector cells, T helper type 1 (Th1) and T helper type 2 (Th2) cells [1, 2]. Th1 cells secrete IFN-γ, TNF-α, and TNF-β and are important for the development of delayed type hypersensitivity (DTH) reactions and protective responses to intracellular pathogens [1, 2]. These cells also contribute to the pathology of autoimmune disease and graft rejection. Th2 cells express and secrete IL-4, IL-5, and/or IL-13 and are essential for the development of humoral and allergic reactions [1, 2]. During T cell activation, the relative cytokine milieu within the local microenvironment is a major determinant of the direction of pTh cell differentiation. Cytokines such as IL-12 and to a lesser extent IFN-γ directly induce pTh cell differentiation into type 1 cells [1]. In contrast, IL-4 stimulates pTh cell differentiation into type 2 cells even in the presence of moderate levels of IL-12 and IFN-γ [2]. In addition to IFN-γ, IL-12 and IL-4, recent evidence also suggests an important role for cytokines such as IFN-(, IL-1α/β, IL-15, and IL-18 in stimulating type 1 responses [2] and IL-10 and IL-13 in stimulating type 2 responses [1, 3]. Additional factors including hormones, growth factors and co-stimulatory molecules have also been shown to influence T cell development of type 1 or type 2 responses [1].
Vitamin A (VA) or VA-like analogs known as retinoids, are potent hormonal modifiers of rodent type 1 or type 2 responses but a definitive description of their mechanism(s) of action is lacking [4–16]. Several early studies using models of pathogen-challenged rodents indicated that VA deficiency induced a dominant Th1 response that interfered with the development of a protective humoral response [17]. These researchers proposed several potential mechanisms to account for these observations including the direct downregulation of T cell IFN-γ synthesis, direct promotion of Th2-cell differentiation, and/or alteration of accessory or antigen presenting cell function toward a Th2-inducing phenotype [18]. Recent evidence from interventional studies show that VA supplementation of VA-deficient infants and children reduces morbidity and/or mortality from measles, malaria, and certain forms of diarrhea [16]. These studies have stimulated renewed interest in elucidating VA's role in the immune response, particularly in modification of human Th1 or Th2 response development.
There are a number of contradictory findings in the literature examining the effects of retinoids on type 1 and 2 cytokine production in rodent models and cells. Several reports using murine and rat models of VA deficiency have demonstrated diminished type 1 reactions including DTH and anti-viral responses [7, 19–21]. Exogenous administration of VA or RA have also been shown to increase DTH reactions and augment immune responses to viruses suggesting that these compounds potentiate type 1 reactions [21, 22]. Several additional published studies using in vitro and in vivo systems of VA or retinoid deficiency and rodents and humans have also demonstrated either inhibitory, stimulatory or no effects on IFN-γ production [4–15, 23, 24]. As for Th2 cytokines, to date only one study has described a decrease in IL-4 production in VA deficiency [18], while several recent studies have demonstrated that retinoids induce IL-4 synthesis during in vitro murine T cell activation [9, 25, 26]. The majority of rodent studies have failed to demonstrate any effect of exogenous retinoids on IL-4 production but have observed a type 2-promoting effect of RA only when exogenous IL-4 was added to the cultures [12, 22, 27–29]. However, a recent study by Iwata et al. [29] demonstrated the direct effects of ATRA and 9-cis-RA on Th2 cytokine production by murine T cells derived from TCR transgenic mice. These authors also demonstrate the ability of RA to inhibit Th1 cytokine responses, while enhancing IL-4 production by Th2-polarized cells. In contrast, RA has also been shown to inhibit IL-4 production by a antigen-stimulated rat mast cell line [30] and inhibited IL-4-induced IgE synthesis from CD40-stimulated B cells [31, 32]. Moreover, additional studies have suggested that VA or retinoids possess limited direct type 2 differentiating effects on purified T cells but appear to act primarily at the level of the APC by reducing type 1 cytokine synthesis [28, 33]. Obviously, given all the variations in these findings, the selective differentiating effects of VA and retinoids on cytokine synthesis by T cells remains controversial. Despite all of this work, little to no detailed data exists utilizing purified human T cells and T cell subsets in such studies. In the current manuscript, we provide the first systematic analysis of the effects of the retinoids, ATRA and 9-cis-RA, on the development of a Th2 cytokine response as well as several cytokines and chemokines using an in vitro model of human T cell activation.
Results
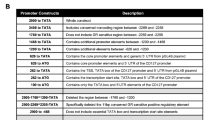
ATRA and 9-cis-RA inhibit Th1 and promote Th2 reactions by human T cells and peripheral blood mononuclear cells (PBMC)
Given the multiple reports describing the effects of retinoids on cytokine production by murine splenocytes and T cells, we initially examined the effects of various concentrations of ATRA and 9-cis-RA on the production of Th1- and Th2-associated cytokines by anti-CD3-stimulated human T cells and PBMC in vitro. Culture supernatants were examined 48 hrs after stimulation for cytokine levels. The results in Figure 1 demonstrate a representative dose response curve of ATRA and 9-cis-RA on the expression of IL-4, IL-5 and IFN-γ by human T cells and PBMC. These data reveal that the Th2 cytokines, IL-4 and IL-5, are induced in T cells and PBMC in a dose-dependent manner, while the production of the Th1 cytokine, IFN-γ, is inhibited in response to increasing concentrations of ATRA and 9-cis-RA. These findings were highly reproducible in greater than 95% of the PBMC and T cells donors examined (n > 20). Based on the above curves, ATRA and 9-cis-RA were utilized in subsequent experiments at the 10-7 M (100 nM) concentration, a dose range that we and others [48]. This would allow the cells to survive for the 10–14 days in serum-free media it takes to deplete them of endogenous retinoids [35]. However, the time spent ex vivo greatly adds to the potential for artifactual data generation. Perhaps for these reasons, most recent studies, including many human studies on the potential immunoregulatory mechanisms of retinoids in primary T cells or PBMCs generally use unadulterated FBS and cells from vitamin A sufficient animals or humans [13, 65]. STAT-6 also induces the expression of Ets-1, MAF and GATA-3 and reduces the expression of IL-12R∃2 message independently of IL-4 production [65]. Here, through the use of real time RT-PCR using several of the retinoid-treated T cells and PBMCs, we also observed increases in the gene expression of the Th2 factors, cMAF, GATA-3, and STAT-6, using ATRA and a concomitant decrease in the expression of the Th1 factor, T-bet, 4–12 hours post stimulation (Figure 6). These data strongly support a specific role for retinoids in the development of Th2 cells.
Conclusion
In conclusion, we have demonstrated that ATRA and 9-cis-RA increase the expression of IL-4, IL-5 and IL-13 but not IL-10 mRNA and protein from activated human T cells. ATRA acts early and directly polarizes T cells towards type 2 responses even in the presence of type 1-inducing signals or in the absence of CD28-costimulation. Although ATRA decreased IL-12 synthesis within PBMC cultures, this was not obligatory as RA directly induced type 2 cytokine production by highly purified human T cells in the absence of APCs. A better understanding of the type 2 cytokine promoting activity of ATRA and 9-cis-RA in human T cells would provide better clinical interventions to boost vaccine efficacy to certain antigens or to reduce various types of pro-inflammatory and autoimmune pathologies [66].
Methods
Reagents
ATRA, 9-cis-RA were purchased from Sigma, St. Louis, MO. Retinoids were dissolved at various concentrations in 100% ETOH, overlayered with argon gas and stored at -80°C in the dark until used. Recombinant human IFN-γ, IL-4, IL-12 and IL-18 were obtained from R & D Systems (Minneapolis, MN). Recombinant IFN-γ was obtained from Biosource Int. (Camarillo, CA). Neutralizing monoclonal antibodies (mAbs) to human IFN-γ (clone 25718.111) IL-4 (clone 34019.111), and IL-12 (clone 24910.1) were also obtained from R & D Systems. Based upon manufacturer's testing lot-specific testing, 1 :g of anti-IFN-γ, anti-IL-4, and anti-IL-12 will neutralize 5 ng/ml, 300 pg/ml and 700 pg/ml of rhIFN-γ, rhIL-4, and rhIL-12, respectively.
Cell preparation
Whole blood was acquired from healthy human volunteers between the ages of 21–55 years who provided informed consent. PBMC were isolated by Ficoll Paque (Amersham Pharmacia Biotech, Piscataway, NJ) density gradient centrifugation followed by treatment with ammonium chloride (ACK) lysis solution (Biofluids, Gaithersburg, MD) to eliminate the remaining erythrocytes. The isolated cells were subsequently washed 2 times in PBS and resuspended in RPMI 1640 (Biofluids) supplemented with 10% heat-inactivated FBS (Sigma), 2% heat-inactivated pooled human AB serum (Sigma), 50 μM mercaptoethanol (Gibco BRL Gaithersburg, MD), 1 mM sodium pyruvate (Biofluids), 2 mM glutamine, 1 × non-essential amino acid solution (Biofluids), 1 mg/ml gentamicin (Biowhittaker, Walkersville, MD), 100 U/ml penicillin (Biofluids), 100 :g/ml streptomycin (Biofluids), and 20 mM HEPES buffer (Biofluids). T cells, CD4+ T cells and CD8+ T cells were isolated by negative selection using enrichment columns according to manufacturer's instructions (R & D Systems). All of these cells were typically > 93% pure as assessed by flow cytometric analysis. The contaminating cell population was largely CD8+ cells. Most likely, these cells were NK cells based on their size and granularity.
Cell culture and harvest
PBMC (2.5 × 10 6 cells/ml) were activated with 200 ng/ml of immobilized anti-CD3ε OKT-3, Ortho, Raritan, NJ) ± 0.001 to 1 μM of various retinoids or ETOH vehicle control for 48 h. IL-2 (Teceleukin, Hoffman LaRoche, Nutley, NJ) at 10 U/ml was added where indicated. Where indicated, 1 μg/ml of neutralizing anti-cytokine mAb was added to the cultures. Alternatively, T cells (1.0 × 10 6 cells/ml) were activated with 200 ng/ml of immobilized anti-CD3 and 0.1 to 1 μg of soluble anti-CD28 (clone 28.2, Pharmingen) or IL-2 at 10 U/ml was added where indicated to provide co-activation or costimulatory signals. PBMCs or T cells were harvested at various times after incubation at 37° and 5% CO2. The 48 hr time interval was selected for many of the studies shown based on the optimal and reproducible cytokine expression in response to anti-CD3 mAb. Non-adherent cells were decanted from the flasks and centrifuged to obtain supernatants. The flasks were then treated with Enzyme-Free cell disassociation solution (Specialty Media, Phillipsburg, NJ) to remove the adherent cells (a typical result of cell activation and the anti-CD3 coated flasks) and were gently scraped to remove and harvest the cells. Viable cells from the decanted cells and cell removal mixture were isolated by Ficoll Paque density gradient centrifugation (as described above). Cell viability was not significantly affected by this enzyme treatment process (viability >95%).
It should be noted that we have also utilized the serum free medium AIMV in these various cultures and observed similar effects to serum containing medium (data not shown).
Cytokine ELISA
ELISA (Biosource) and Bio-Plex Human Cytokine 17-Plex (Biorad, Hercules, CA) were utilized to examine the following human-specific cytokines: IFN-α, IFN-γ, IL-1α, IL-1β, IL-4, IL-5, IL-6, IL-7, IL-8, IL-10, IL-12 p70, IL-13, IL-15, IL-17, G-CSF, GM-CSF, MIP-1∀, MIP-1∃, RANTES, MCP-1 and TNF-α. The IL-18 ELISA was obtained from R & D Systems (Minneapolis, MN). All of the ELISAs and multiplex assays were performed according to the manufacturer's instructions. The results are expressed as pg/ml or ng/ml and all assays were run in duplicate with at least three separate experiments being examined.
Real Time PCR
Cytoplasmic RNA was extracted and purified using a commercially available kit (RNAeasy, Qiagen, Valencia, CA). Purified RNA was electrophoresed on a 1% agarose gel to assess the integrity of the purified RNA. One :g of RNA was reverse transcribed into cDNA using a commercial available kit (Applied Biosystems, Foster City, CA). One hundred pg RNA equivalent of this cDNA was used for PCR amplification. PCR reactions were performed in special optical tubes in a 96 well microtiter plate format on an ABI PRISM 7700 Sequence Detector System (PE Applied Biosystems) using pre-developed FAM- and TAMRA-labeled internal oligonucleotide probes and primers for IFN-γ, IL-4, IL-5, IL-10, IL-12p30, IL-12p40, IL-15, and TNF-α (PE Applied Biosystems). Each reagent also contains VIC- and TAMRA-labeled internal oligonucleotide probes and primers specific for the 18S RNA ribosomal subunit. Amplification conditions were as follows 25°C for two min; 95°C for 10 min; 40 cycles of 95°C 15 s and 60°C for 1 min. Fluorescence signals measured during amplification were processed post-amplification and were regarded as positive if the fluorescence intensity was ten fold greater than the standard deviation of the baseline fluorescence. This level is defined as the threshold cycle (Ct). The Ct value for 18S ribosomal subunit was subtracted from the Ct value for each cytokine message to normalize for RNA content. This value is defined as ΔCT. To evaluate the effects of retinoids, ΔCTtreatment was subtracted from ΔCtcontrol. This value is defined as ΔΔCT. The relative folds increase or decrease was then calculated as 2 -ΔΔCT.
The PCR was also set up using SYBR green Master Mix (Applied Biosystems), 1 μl cDNA and gene-specific primers at a final concentration of 0.3 μM. Thermal cycling was carried out on the Applied Biosystems GeneAmp 7700 Sequence Detector and SYBR green dye intensity was analyzed using GeneAmp 7700 SDS software. Primers for human GATA3, STAT6, C-MAF, and T-bet genes and glyceraldehyde-3-phosphate dehydrogenase (GAPDH) as control were designed using ABI prism software (PE Applied Biosystems). Primers are available upon request. Similar amplification procedures and data computation were followed as described above. No PCR products were generated from genomic versus cDNA template.
Intracellular Flow Cytometry and ELISPOT analysis
Mouse anti-human CD3-Cy-Chrome®, anti-human IL-4-phycoerytrin (PE), anti-human IFN-(-fluorescein isothiocyanate (FITC) anti-human TNF-∀-FITC, and the appropriately labeled isotype control mAbs were obtained from Pharmingen. PBMCs were cultured for 36 hrs as described above after which the cells were treated with 2 :M monensin (Sigma) and subsequently harvested as described above. Cells (0.25 × 106) were suspended in 50 :L of staining buffer (1% FCS, 1% goat serum, 2.5 :g of mouse IgG/50 μL) in round-bottom 96-well plates at 4°C for 15 min. 5 :L of the appropriate dilution of each antibody was then added. Cells were then incubated for 30–40 min at 4°C. Cells were pelleted and medium was aspirated carefully. Cells were then washed with 100 :L of PBS/FBS buffer twice. Cells were fixed and permeabilized with Cytofix/Cytoperm® solution (Pharmingen). Various combinations of labeled anti-human cytokines were used to stain cells. Cytochrome-conjugated mouse IgG1 mAb and PE mouse-IgG were used as isotype controls at the same concentrations as the anti-cytokine antibody. Additional controls in which the labeled mAbs and 10 fold saturating recombinant cytokine proteins were pre-incubated for 30 min at room temperature before staining (IL-4). Alternatively, cells were pretreated with unlabeled mAb (IFN-γ). Three-color cytofluorometry was performed using a FacScan (Becton Dickinson, San Diego, CA). A minimum of 10,000 CD3+ cells were analyzed in these experiments. Data are expressed as the % of CD3+ cells expressing the marker of interest or the mean channel number (MCN) of the marker's fluorescent intensity.
The ELISPOT assays (BD Biosciences) used to quantify IFN-γ-, IL-4, and IL-5-producing T cells were performed according to the manufacturer's instructions. Briefly, T cells were prepared at different cell densities ranging from 1 × 105, 1 × 106, and 2.5 × 106 cells per ml and 100 :l of the suspensions were added to each well of mouse anti-human cytokine antibody-coated BD ELISPOT plates. The cells were stimulated using ATRA or 9-cis-RA and/or soluble anti-CD3 and CD28 antibodies described above under cell culture. The plates were then incubated at 37°C in a 5% CO2 humidified incubator for 24 hr after which the cell suspension were aspirated, the wells were washed with various combinations of deionized water and wash buffer, and subsequently developed using the proper antibody, conjugate and substrate pairs defined by the manufacturer. The plates were air-dried overnight at room temperature and the plates were stored in a sealed bag in the dark until analyzed. Spots were then enumerated using an ImmunoSpot® Series 2 Analyzer (Cellular Technology Limited, Cleveland, Ohio) and the supporting ImmunoSpot® Software. Spots were counted by an automated system using a defined set of parameters for size, intensity, and gradient. The background (the mean numbers of spots in wells without stimulation) was subtracted from each well on each cytokine plate. A response was considered positive if the average number of cytokine-producing cells (CPC) per triplicate wells exceeded background +/- 2SD. The data are shown as the average number of CPC per 106 cells.
Statistical analysis
Data were analyzed for equality of variance using Fischer's F test (Statview 5.0 for Macintosh, Abacus Concepts, Berkeley, CA). If the variance was heterogeneous, the appropriate transformation of the data was performed. A two-tailed paired T test was then used to determine statistical significance. A P < 0.05 was considered statistically significant for all analysis.
Abbreviations
- ATRA:
-
all-trans retinoic acid
- 9-cis-RA:
-
9-cis- retinoic acid
- DTH:
-
delayed type hypersensitivity
- pTh:
-
precursor T helper
- RARs:
-
retinoic acid receptors
- RXRs:
-
retinoid X receptors
- VA:
-
Vitamin A
References
Seder RA, Mosmann T: Differentiation of effector phenotypes of CD4+ and CD8+ T cells. Fundamental Immunology. Edited by: Paul WE. 1998, Philadelphia: Lippincott, Williams and Wilkins, 525-
Murphy KM, Ouyang W, Farrar JD, Yang J, Ranganath S, Asnagli H, Afkarian M, Murphy TL: Signaling and transcription in T helper development. Annu Rev Immunol. 2000, 18: 451-94. 10.1146/annurev.immunol.18.1.451.
McKenzie AN: Regulation of T helper type 2 cell immunity by interleukin-4 and interleukin-13. Pharmacol Ther. 2000, 88: 143-51. 10.1016/S0163-7258(00)00088-7.
Abb J, Abb H, Deinhardt F: Retinoic acid suppression of human leukocyte interferon production. Immunopharmacology. 1982, 4: 303-10. 10.1016/0162-3109(82)90051-0.
Carman JA, Hayes CE: Abnormal regulation of IFN-gamma secretion in vitamin A deficiency. J Immunol. 1991, 147: 1247-52.
Carman JA, Pond L, Nashold F, Wassom L, Hayes CE: Immunity to Trichinella spiralis infection in vitamin A-deficient mice. J Exp Med. 1992, 175: 111-20. 10.1084/jem.175.1.111.
Wiedermann U, Hanson LA, Kahu H, Dahlgren UI: Aberrant T-cell function in vitro and impaired T-cell dependent antibody response in vivo in vitamin A-deficient rats. Immunology. 1993, 80: 581-6.
Ikeda K, Matsuo S, Asano K, Okamoto K: Modulation of cytokine secretion by mesenteric lymph node cells from vitamin A-deficient mice during Hymenolepis nana infection. In Vivo. 1994, 8: 1015-7.
Racke MK, Burnett D, Pak SH, Albert PS, Cannella B, Raine CS, McFarlin DE, Scott DE: Retinoid treatment of experimental allergic encephalomyelitis. IL-4 production correlates with improved disease course. J Immunol. 1995, 154: 450-8.
Cippitelli M, Ye J, Viggiano V, Sica A, Ghosh P, Gulino A, Santoni A, Young HA: Retinoic acid-induced transcriptional modulation of the human interferon-gamma promoter. J Biol Chem. 1996, 271: 26783-93. 10.1074/jbc.271.43.26783.
Wiedermann U, Chen XJ, Enerback L, Hanson LA, Kahu H, Dahlgren UI: Vitamin A deficiency increases inflammatory responses. Scand J Immunol. 1996, 44: 578-84. 10.1046/j.1365-3083.1996.d01-351.x.
Frankenburg S, Wang X, Milner Y: Vitamin A inhibits cytokines produced by type 1 lymphocytes in vitro. Cell Immunol. 1998, 185: 75-81. 10.1006/cimm.1998.1268.
Wauben-Penris PJ, Cerneus DP, van den Hoven WE, Leuven PJ, den Brok JH, Hall DW: Immunomodulatory effects of tretinoin in combination with clindamycin. J Eur Acad Dermatol Venereol. 1998, 11 (Suppl 1): S2-7. 10.1111/j.1468-3083.1998.tb00900.x. discussion S28–9
Fox FE, Kubin M, Cassin M, Niu Z, Trinchieri G, Cooper KD, Rook AH: Retinoids synergize with interleukin-2 to augment IFN-gamma and interleukin-12 production by human peripheral blood mononuclear cells. J Interferon Cytokine Res. 1999, 19: 407-15. 10.1089/107999099314117.
Cui D, Moldoveanu Z, Stephensen CB: High-level dietary vitamin A enhances T-helper type 2 cytokine production and secretory immunoglobulin A response to influenza A virus infection in BALB/c mice. J Nutr. 2000, 130: 1132-9.
Villamor E, Fawzi WW: Vitamin A supplementation: implications for morbidity and mortality in children. J Infect Dis. 2000, 182 (Suppl 1): S122-33. 10.1086/315921.
Cantorna MT, Nashold FE, Hayes CE: Vitamin A deficiency results in a priming environment conducive for Th1 cell development. Eur J Immunol. 1995, 25: 1673-9.
Cantorna MT, Nashold FE, Hayes CE: In vitamin A deficiency multiple mechanisms establish a regulatory T helper cell imbalance with excess Th1 and insufficient Th2 function. J Immunol. 1994, 152: 1515-22.
Smith SM, Levy NS, Hayes CE: Impaired immunity in vitamin A-deficient mice. J Nutr. 1987, 117: 857-65.
Ahmed F, Jones DB, Jackson AA: Effect of vitamin A deficiency on the immune response to epizootic diarrhoea of infant mice (EDIM) rotavirus infection in mice. Br J Nutr. 1991, 65: 475-85. 10.1079/BJN19910106.
Ross AC, Stephensen CB: Vitamin A and retinoids in antiviral responses. Faseb J. 1996, 10: 979-85.
Niwa S, Ochi T, Hirano Y, Wang T, Inagaki N, Shudo K, Nagai H: Effect of Am-80, a retinoid derivative, on 2, 4-dinitrofluorobenzene-induced contact dermatitis in mice. Pharmacology. 2000, 60: 208-14. 10.1159/000028371.
Matikainen S, Lehtonen A, Sareneva T, Julkunen I: Regulation of IRF and STAT gene expression by retinoic acid. Leuk Lymphoma. 1998, 30: 63-71.
Austenaa LM, Ross AC: Potentiation of interferon-gamma-stimulated nitric oxide production by retinoic acid in RAW 264.7 cells. J Leukoc Biol. 2001, 70: 121-9.
Stephensen CB, Jiang X, Freytag T: Vitamin A deficiency increases the in vivo development of IL-10-positive Th2 cells and decreases development of Th1 cells in mice. J Nutr. 2004, 134: 2660-6.
Stephensen CB, Rasooly R, Jiang X, Ceddia MA, Weaver CT, Chandraratna RA, Bucy RP: Vitamin A enhances in vitro Th2 development via retinoid X receptor pathway. J Immunol. 2002, 168: 4495-503.
Nagai H, Matsuura S, Bouda K, Takaoka Y, Wang T, Niwa S, Shudo K: Effect of Am-80, a synthetic derivative of retinoid, on experimental arthritis in mice. Pharmacology. 1999, 58: 101-12. 10.1159/000028272.
Hoag K, Nashold F, Goverman J, Hayes C: Retinoic acid enhances the Th2-stimulating ability of the antigen presenting cell. Experimental Biology 2000. 2000, Federation of American Societies for Experimental Biology, 14: A627-
Iwata M, Eshima Y, Kagechika H: Retinoic acids exert direct effects on T cells to suppress Th1 development and enhance Th2 development via retinoic acid receptors. Int Immunol. 2003, 15: 1017-25. 10.1093/intimm/dxg101.
Hirasawa N, Kagechika H, Shudo K, Ohuchi K: Inhibition by retinoids of antigen-induced IL-4 production in rat mast cell line RBL-2H3. Life Sci. 2001, 68: 1287-94. 10.1016/S0024-3205(00)01034-1.
Worm M, Krah JM, Manz RA, Henz BM: Retinoic acid inhibits CD40 + interleukin-4-mediated IgE production in vitro. Blood. 1998, 92: 1713-20.
Hoag KA, Nashold FE, Goverman J, Hayes CE: Retinoic acid enhances the T helper 2 cell development that is essential for robust antibody responses through its action on antigen-presenting cells. J Nutr. 2002, 132: 3736-9.
Kang BY, Chung SW, Kim SH, Kang SN, Choe YK, Kim TS: Retinoid-mediated inhibition of interleukin-12 production in mouse macrophages suppresses Th1 cytokine profile in CD4(+) T cells. Br J Pharmacol. 2000, 130: 581-6. 10.1038/sj.bjp.0703345.
Ballow M, **ang S, Greenberg SJ, Brodsky L, Allen C, Rich G: Retinoic acid-induced modulation of IL-2 mRNA production and IL-2 receptor expression on T cells. Int Arch Allergy Immunol. 1997, 113: 167-9.
Cantorna MT, Nashold FE, Chun TY, Hayes CE: Vitamin A down-regulation of IFN-gamma synthesis in cloned mouse Th1 lymphocytes depends on the CD28 costimulatory pathway. J Immunol. 1996, 156: 2674-9.
Reiner SL: Helper T cell differentiation, inside and out. Curr Opin Immunol. 2001, 13: 351-5. 10.1016/S0952-7915(00)00226-0.
Loots GG, Locksley RM, Blankespoor CM, Wang ZE, Miller W, Rubin EM, Frazer KA: Identification of a coordinate regulator of interleukins 4, 13, and 5 by cross-species sequence comparisons. Science. 2000, 288: 136-40. 10.1126/science.288.5463.136.
Elson LH, Nutman TB, Metcalfe DD, Prussin C: Flow cytometric analysis for cytokine production identifies T helper 1, T helper 2, and T helper 0 cells within the human CD4+CD27-lymphocyte subpopulation. J Immunol. 1995, 154: 4294-301.
de Boer BA, Fillie YE, Kruize YC, Yazdanbakhsh M: Antigen-stimulated IL-4, IL-13 and IFN-gamma production by human T cells at a single-cell level. Eur J Immunol. 1998, 28: 3154-60. 10.1002/(SICI)1521-4141(199810)28:10<3154::AID-IMMU3154>3.0.CO;2-A.
Verhagen CE, van der Pouw Kraan TC, Buffing AA, Chand MA, Faber WR, Aarden LA, Das PK: Type 1- and type 2-like lesional skin-derived Mycobacterium leprae-responsive T cell clones are characterized by coexpression of IFN-gamma/TNF-alpha and IL-4/IL-5/IL-13, respectively. J Immunol. 1998, 160: 2380-7.
Urban J, Fang H, Liu Q, Ekkens MJ, Chen SJ, Nguyen D, Mitro V, Donaldson DD, Byrd C, Peach R, et al.: IL-13-mediated worm expulsion is B7 independent and IFN-gamma sensitive. J Immunol. 2000, 164: 4250-6.
Kim JI, Ho IC, Grusby MJ, Glimcher LH: The transcription factor c-Maf controls the production of interleukin-4 but not other Th2 cytokines. Immunity. 1999, 10: 745-51. 10.1016/S1074-7613(00)80073-4.
Mori A, Kaminuma O, Mikami T, Inoue S, Okumura Y, Akiyama K, Okudaira H: Transcriptional control of the IL-5 gene by human helper T cells: IL-5 synthesis is regulated independently from IL-2 or IL-4 synthesis. J Allergy Clin Immunol. 1999, 103: S429-36. 10.1016/S0091-6749(99)70158-2.
Rafiq K, Bullens DM, Kasran A, Lorre K, Ceuppens JL, Van Gool SW: Differences in regulatory pathways identify subgroups of T cell-derived Th2 cytokines. Clin Exp Immunol. 2000, 121: 86-93. 10.1046/j.1365-2249.2000.01273.x.
Engedal N, Gjevik T, Blomhoff R, Blomhoff HK: All-trans retinoic acid stimulates IL-2-mediated proliferation of human T lymphocytes: early induction of cyclin D3. J Immunol. 2006, 177 (5): 2851-61.
Garbe A, Buck J, Hammerling U: Retinoids are important cofactors in T cell activation. J Exp Med. 1992, 176 (1): 109-17. 10.1084/jem.176.1.109.
Buck J, Myc A, Garbe A, Cathomas G: Differences in the action and metabolism between retinol and retinoic acid in B lymphocytes. J Cell Biol. 1991, 115 (3): 851-9. 10.1083/jcb.115.3.851.
Ep**er TM, Buck J, Hammerling U: Growth control or terminal differentiation: endogenous production and differential activities of vitamin A metabolites in HL-60 cells. J Exp Med. 1993, 178 (6): 1995-2005. 10.1084/jem.178.6.1995.
Iwata M, Hirakiyama A, Eshima Y, Kagechika H, Kato C, Song SY: Retinoic acid imprints gut-homing specificity on T cells. Immunity. 2004, 21 (4): 527-38. 10.1016/j.immuni.2004.08.011.
Allende LM, Corell A, Madrono A, Gongora R, Rodriguez-Gallego C, Lopez-Goyanes A, Rosal M, Arnaiz-Villena A: Retinol (vitamin A) is a cofactor in CD3-induced human T-lymphocyte activation. Immunology. 1997, 90 (3): 388-96. 10.1111/j.1365-2567.1997.00388.x.
Napoli JL: Quantification of physiological levels of retinoic acid. Meth Enzymology. 1986, 123: 112-124.
Kojima R, Fujimori T, Kiyota N, Toriya Y, Fukuda T, Ohashi T, Sato T, Yoshizawa Y, Takeyama K, Mano H: In vivo isomerization of retinoic acids. Rapid isomer exchange and gene expression. J Biol Chem. 1994, 269 (51): 32700-07.
Kurlandsky SB, Gamble MV, Ramakrishnan R, Blaner WS: Plasma delivery of retinoic acid to tissues in the rat. J Biol Chem. 1995, 270: 17850-57. 10.1074/jbc.270.30.17850.
Adamson PC: Pharmacokinetics of all-trans-retinoic acid: clinical implications in acute promyelocytic leukemia. Semin Hematol. 1994, 31 (4 Suppl 5): 14-7.
Chen Q, Ross AC: Inaugural Article: Vitamin A and immune function: retinoic acid modulates population dynamics in antigen receptor and CD38-stimulated splenic B cells. Proc Natl Acad Sci USA. 2005, 102 (40): 14142-9. 10.1073/pnas.0505018102.
DeCicco KL, Zolfaghari R, Li N, Ross AC: Retinoic acid and polyriboinosinic acid act synergistically to enhance the antibody response to tetanus toxoid during vitamin A deficiency: possible involvement of interleukin-2 receptor-beta, signal transducer and activator of transcription-1, and interferon regulatory factor-1. J Infect Dis. 2000, 182 (Suppl 1): S29-36. 10.1086/315908.
Na SY, Kang BY, Chung SW, Han SJ, Ma X, Trinchieri G, Im SY, Lee JW, Kim TS: Retinoids inhibit interleukin-12 production in macrophages through physical associations of retinoid X receptor and NFkappaB. J Biol Chem. 1999, 274: 7674-80. 10.1074/jbc.274.12.7674.
Stephensen CB, Rasooly R, Jiang X, Ceddia MA, Weaver CT, Chandraratna RAS, Bucy RP: Retinoic acid modulates ex vivo Th1/Th2 phenotype development of naïve T-cells from DO11.10 T cell receptor transgenic mice. Experimental Biology 2001. 2001, Federation of American Societies for Experimental Biology, 15: A1093-
Lanvers C, Hempel G, Blaschke G, Boos J: Chemically induced isomerization and differential uptake modulate retinoic acid disposition in HL-60 cells. Faseb J. 1998, 12: 1627-33.
Grenningloh R, Gho A, di Lucia P, Klaus M, Bollag W, Ho IC, Sinigaglia F, Panina-Bordignon P: Cutting Edge: Inhibition of the retinoid X receptor (RXR) blocks T helper 2 differentiation and prevents allergic lung inflammation. J Immunol. 2006, 176 (9): 5161-6.
King CL, Stupi RJ, Craighead N, June CH, Thyphronitis G: CD28 activation promotes Th2 subset differentiation by human CD4+ cells. Eur J Immunol. 1995, 25: 587-95.
Oki S, Otsuki N, Kohsaka T, Azuma M: Stat6 activation and Th2 cell differentiation [correction of proliferation] driven by CD28 [correction of CD28 signals]. Eur J Immunol. 2000, 30: 1416-24. 10.1002/(SICI)1521-4141(200005)30:5<1416::AID-IMMU1416>3.0.CO;2-M.
Raouf A, Li V, Kola I, Watson DK, Seth A: The Ets1 proto-oncogene is upregulated by retinoic acid: characterization of a functional retinoic acid response element in the Ets1 promoter. Oncogene. 2000, 19: 1969-74. 10.1038/sj.onc.1203505.
Liu TX, Zhang JW, Tao J, Zhang RB, Zhang QH, Zhao CJ, Tong JH, Lanotte M, Waxman S, Chen SJ, et al.: Gene expression networks underlying retinoic acid-induced differentiation of acute promyelocytic leukemia cells. Blood. 2000, 96: 1496-504.
Kurata H, Lee HJ, O'Garra A, Arai N: Ectopic expression of activated Stat6 induces the expression of Th2-specific cytokines and transcription factors in develo** Th1 cells. Immunity. 1999, 11: 677-88. 10.1016/S1074-7613(00)80142-9.
Nozaki Y, Yamagata T, Yoo BS, Sugiyama M, Ikoma S, Kinoshita K, Funauchi M, Kanamaru A: The beneficial effects of treatment with all-trans-retinoic acid plus corticosteroid on autoimmune nephritis in NZB/WF mice. Clin Exp Immunol. 2005, 139: 74-83. 10.1111/j.1365-2249.2005.02654.x.
Acknowledgements
The content of this publication does not reflect the views or policies of the Department of Health and Human Services, nor does mention of trade names, commercial products or organizations imply endorsement by the U.S. Government. This research was supported in part by the Intramural Research Program of the National Institute on Aging, National Institutes of Health. We would like to thank the members of the GRC Flow Cytometry Laboratory and the Pheresis Unit for assistance with the flow cytometric analysis presented herein. We would like to thank Drs. Eric Schaffer, Paritosh Ghosh, and Dan L. Longo for their thoughtful review and comments on this manuscript. In addition, we would also like to thank Ms. Angie Feehley for her assistance in the preparation of this manuscript and Mr. Gregory Maher for his excellent technical assistance.
Author information
Authors and Affiliations
Corresponding author
Additional information
Authors' contributions
HD, GC, RP, MLK, AW, VDD, CN and DDT did the experiments. HD and DDT prepared the figures and co-wrote the paper. DDT supervised the work and edited the manuscript. All authors have read and approved the final version of the manuscript.
Authors’ original submitted files for images
Below are the links to the authors’ original submitted files for images.
Rights and permissions
Open Access This article is published under license to BioMed Central Ltd. This is an Open Access article is distributed under the terms of the Creative Commons Attribution License ( https://creativecommons.org/licenses/by/2.0 ), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
About this article
Cite this article
Dawson, H.D., Collins, G., Pyle, R. et al. Direct and indirect effects of retinoic acid on human Th2 cytokine and chemokine expression by human T lymphocytes. BMC Immunol 7, 27 (2006). https://doi.org/10.1186/1471-2172-7-27
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/1471-2172-7-27