Key summary points
Focus of prognostic factors in elderly covid19 patients admitted in long term unit.
AbstractSection FindingsNasal swab test at discharge, infection, age and frailty represented risk factors associated with increased mortality.
AbstractSection MessageAbsence of negativization of nasal swab test is the major risk factor for mortality.
Abstract
Methods
A limited amount of data is now available on prognostic factors and mortality among elderly people resident in Long-Term Care facilities and in post-acute units. These populations (in particular those with underlying chronic medical conditions) seem to have higher risk of morbidity and mortality related to COVID-19 disease, but further evidence is needed. The aim of our study is to investigate the impact of some well-known prognostic factors in elderly patients (≥ 65 years) with COVID-19 admitted in the Long-Term Care setting in AUSL Ferrara, Italy. We performed binary regression logistic analysis for some variables (demographic data, clinical data including nasal swab test (NST) at discharge and frailty assessments) to find potential predictors of mortality. We subsequently tested statistically significant variables using Kaplan–Meier curves and Cox-regression models to find survival outcomes and related hazard ratio.
Results
Risk factors associated with increased mortality resulted NST at discharge, infection, age and frailty. At a further secondary analysis carried out between NST at discharge, age and clinical frailty scale (CFS) < 5, we found a positive correlation between NST at discharge and CFS < 5. Kaplan–Meier curves showed a statistically significant difference regarding frailty and NST at discharge but not for age.
Conclusion
Our study showed that absence of negativization of NST at discharge and frailty are strong predictors for mortality in elderly COVID-19 patients admitted in Long-Term Care facilities, while age and the comorbidity burden are less important.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Aim
A severe respiratory disease was recently reported in Wuhan, Hubei province, China, with the first patient hospitalized on 12 December 2019 [1] and spreaded worldwide, officially being defined as a pandemic by WHO on 11 March 2020 [2]. Clinical severity of infection varies from asymptomatic or mildly symptomatic forms to critical situations with bilateral pneumonia to multiple organ failure [3]. It is crucial to identify prognostic factors related to the most severe forms of disease and mortality. The first data showed a particular vulnerability of the elderly [4, 5]. In fact, older adults have heterogeneous basic clinical conditions and often age and comorbidities do not really reflect the general health status of this kind of patients. For this reason, the concept of “frailty” has been introduced, including different dimensions of performance status and autonomy. Frailty is defined as a condition characterized by a progressive decline in physiological function and by a decrease in strength that leads to greater vulnerability to stress factors, resulting in increased risk of adverse outcomes [6].
Frailty was found to be an independent predictor for death in hospitalized patients with several clinical conditions as well as COVID-19 [7]. Similarly, disability also plays an important role in predicting mortality and adverse outcomes, especially in older people with COVID-19. Deterioration of functional status, as a sign of an augmented vulnerability state and a declining of biological reserves, is generally considered a strong predictor of poor outcome mainly, but not exclusively, in older people [8,9,10]. Case series have identified age as an independent prognostic factor for mortality. In addition, national registries have shown a high mortality rate among patients older than 80 years [5]. Despite this, studies specifically targeting older patients (≥ 75 years) are few and, though at the highest risk of mortality, information on factors associated with adverse outcome in this population is limited [11]. Similarly, a limited amount of information is available about the natural course of this pandemic and prognostic factors in patients admitted in Long-Term Care facilities [12].
The aim of this paper is to investigate the impact of some well-known prognostic factors in elderly patients (≥ 65 years) with COVID-19 admitted in the Long-Term Care setting in AUSL Ferrara, Italy.
Findings
A total of 471 individuals were admitted between March 2020 and March 2021 in Long-Term Care facilities of the AUSL Ferrara (in particular SS.Annunziata Hospital, Cento and Delta Hospital, Lagosanto). The chosen period includes the first pandemic wave in March 2020 and the second in October 2020. Patients had typical COVID diagnostic criteria: symptoms including respiratory failure and positive nasal swab test (NST) real-time reverse-transcriptase polymerase-chain-reaction (rRT-PCR). All of them were transferred from an Acute Internal Medicine Unit or from an Intensive/Sub-intensive Care Unit, with current or interrupted low-flow O2-support, in order to recover from the illness and improve their functional status. At the time of admission in the Long-Term Care Unit, patients were tested with routine blood sampling and chest X-rays. We recruited in this study 452 patients aged 65 and older, excluding 19 younger patients. Not a single person in our cohort underwent vaccination against Sars-cov2.
The following information were obtained from our computerized medical records and collected from all the individuals included in the study: demographic data (sex, age and residential setting before hospital admission), clinical data (comorbidities expressed with Charlson index, presence of hypertension, diabetes, history of solid or blood tumor, cognitive impairment, endocrinological disorders, obesity, rheumatological, cardiovascular, cerebrovascular, respiratory, hepatic, renal and musculoskeletal disease, necessity of total parenteral nutrition, presence of central venous or urinary catheter, hospital-acquired infections with positive blood cultures requiring antibiotic administration, length of hospital stay and positive/negative NST at discharge), and a frailty pre-admission assessment expressed by clinical frailty scale (CFS) ≥ 5, activities of daily living (ADL) ≤ 2 and polypharmacy (concomitant assumption of ≥ 5 drugs).
We performed NST in our patients at the time of admission and later every 7 days. If a test resulted negative, the patient was discharged. After 21 days of hospitalization, if the test remained positive, the patient was considered recovered from COVID and discharged (according to the decision of our Ministry of Health). Therefore, in our cohort, the number of days of hospitalization almost correspond to the number of days spent with a positive NST.
Patients were divided into two groups, based on the survival outcome from our hospital wards admission (group 1: survived on discharge and group 2: dead on discharge from our hospital wards).
In the descriptive data analysis, continuous variables (age, numbers of drugs, CFS, Charlson index) were expressed as median and standard deviation; p-values were derived using t-test. The categorical and dichotomous variables (sex, comorbidities, ADL < 2, presence of medical devices at admission, NST at discharge and infection during hospitalization) were expressed as absolute values or percentage. P values were obtained using Chi-square test. A p value < 0,05 was considered statistically significant (Table 1).
We compared our cohort to the patients admitted to our ward in the previous year (when Sars-cov2 was unknown), finding significant differences. Our cohort showed greater frailty, and this generated longer hospitalization (Table 2).
To analyze risk factors predicting mortality, a binary logistic regression analysis was performed for dichotomous variables and for continuous variables which were statistically significant at the preliminary analyses (Table 3).
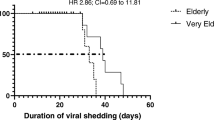
Kaplan–Meier curves (Figs. 1, 2) and Cox-regression models (Table 4) were used to process survival outcomes and related HR resulted statistically significant to binary logistic regression.
To evaluate any correlation between some significant risk factors for mortality to Cox-regression models (NST at discharge, age and CFS), a further binary logistic regression sub-analysis was performed (Table 5).
All the analyses were processed using SPPS software 21.
Patients consent was not necessary as the data were completely anonymous.
Our cohort of COVID-19-positive patients (452) had a median age of 83.3 years. 59% were female and 122 (27%) died. The mortality rate was 73% in female. Patients who died mostly came from home before being admitted to the acute care ward (53.3%). The average hospital stay was 22.89 days.
Statistically significant differences between the two groups were found for: age (p < 0,001); CFS (p < 0,001); sex (p = 0,001); NST at discharge (p < 0,001); other setting before admission (p < 0,001); ADL < 2 (p < 0,001); cardiovascular disease (p = 0,013); musculoskeletal diseases (p = 0,036); dementia (p < 0,001); infection (p < 0,001) (Table 1).
NST at discharge (OR 6,62; p < 0,001), infection (OR 2,32; p = 0,002), age (OR 1,06; p = 0,003) and frailty (OR 1,51; p < 0,001) represented risk factors associated with increased mortality according to binary logistic regression (Table 3).
Analyzing survival with Kaplan–Meier curves, we detected a statistically significant difference regarding frailty (p < 0,001) and NST at discharge (p < 0,001) (Figs. 1, 2).
The Cox-regression model confirmed these data for age (HR 1,05; p < 0,001), CFS (HR 1,32; p < 0,001) and NST at discharge (HR 6,64; p < 0,001) as well (Table 4).
A further binary logistic regression model between NST at discharge, age and CFS showed a positive relationship between NST at discharge and CFS (OR 1,19; p = 0,002) (Table 5).
Message
In our retrospective observational study on COVID-19 patients admitted in Long-Term Care facilities of the AUSL Ferrara between March 2020 and March 2021, we described population characteristics and looked for predictors of mortality. The mortality rate was 26,9%, with a slight increase, not statistically significant (p value 0,33), compared to the previous year (24,3%), and higher in female population. This is apparently in contrast with literature [13,14,15,16], where mortality is higher among men. But the majority of papers refer to acute or intensive care settings [17, 18], while in our paper, we refer to a post-acute setting with a prevalence of female survived patients, burned with greater clinical impairment.
Our study population had an important level of comorbidities (medium Charlson index was 5). In the comparison between dead and survived patients, we found significative some illnesses considered singularly: dementia, obesity, cardiovascular and musculoskeletal disease. These associations were not confirmed with binary analysis in predicting mortality.
In dead group, we found an higher CFS score. In March 2020, the National Institute for Health and Care Excellence (NICE) designed CFS as a first choice in evaluation of frailty in adults patients hospitalized with COVID [19]. We know that frail older adults are more susceptible to a higher risk of develo** a severe form of COVID-19, adverse outcomes, mortality and a different response to vaccination for different mechanisms (inflamm-aging, immunosenescence and reduced microbiota diversity) [20]. Our binary and Cox analysis confirmed the link between frailty and mortality regardless of age and comorbidities burden.
According to the literature, age and frailty are strongly linked with mortality [21, 22] and age is considered an absolute risk factor for death in COVID-19 patients [23,24,25,26]. We also tried to verify the association between these two variables and found a poor correlation. Moreover, age showed no statistical significance in Kaplan–Meier curve (log rank p = 0,07), confirming that greater age, in the over-65 population, does not correlate with greater mortality and frailty, as confirmed by the other authors [15].
Another interesting result in our analysis was the correlation between mortality and the absence of negativization of NST at discharge. We know that immune response to COVID-19 determines susceptibility to the progression of infection as well as being a major determinant of recovery orchestrated by innate immune and adaptive immune responses [27]. Studies have shown that poor outcomes can be predicted where levels of CD8 + T cells and B cells decrease or CD4 + /CD8 + ratio increases [28, 29]. With aging, we have a shift in T cell subpopulations leading to a decline in naïve T cells and a growth in memory T cells, limiting the response against novel infectious agents [30]. We hypothesized that this immunosenescence is the basis of increased persistence of the virus within the host, which means absence of negativization of NST. This, in our study, was a predictive factor for mortality, correlated with frailty and not with disability or comorbidity burden.
Lastly, we found a correlation with the presence of infection, as confirmed by the other authors [[31, 32]]. Cox analysis did not confirm this correlation, meaning that frailty maintains a key role.
Our study shows that frailty and absence of negativization of NST at discharge are strongly predictive factors for mortality in COVID patients admitted in Long-Term Care facilities, while comorbidities burden and advanced age are less important. Immunosenescence could be an important factor explaining these findings. We underline the crucial role of the comprehensive geriatric assessment and specifically the CFS in clinical and prognostic evaluation in the elderly.
Further studies are needed about NST and Long-Term Care facilities, on which to our knowledge information are lacking. We can probably not generalize our results given the present situation showing different variants of Sars-cov2 and the spreading of vaccination. We hope to see new papers on greater populations, different hospital centers, and considering these new variables.
References
Wu F, Zhao S, Yu B, Chen YM, Wang W, Song ZG, Hu Y, Tao ZW, Tian JH, Pei YY, Yuan ML, Zhang YL, Dai FH, Liu Y, Wang QM, Zheng JJ, Xu L, Holmes EC, Zhang YZ (2020) A new coronavirus associated with human respiratory disease in China. Nature 579(7798):265–269
Fumagalli C, Rozzini R, Vannini M, Coccia F, Cesaroni G, Mazzeo F, Cola M, Bartoloni A, Fontanari P, Lavorini F, Marcucci R, Morettini A, Nozzoli C, Peris A, Pieralli F, Pini R, Poggesi L, Ungar A, Fumagalli S, Marchionni N (2020) Clinical risk score to predict in-hospital mortality in COVID-19 patients: a retrospective cohort study. BMJ Open 10(9):e040729
Wu Z, McGoogan JM (2020) Characteristics of and important lessons from the coronavirus disease 2019 (COVID-19) outbreak in China: summary of a report of 72 314 cases from the Chinese Center for disease control and prevention. JAMA 323:1239
Zhou F, Yu T, Du R (2020) Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet 395:1054–1062
Bonanad C, García-Blas S, Tarazona-Santabalbina F, Sanchis J, Bertomeu-González V, Fácila L, Ariza A, Núñez J, Cordero A (2020) The effect of age on mortality in patients with COVID-19: a meta-analysis with 611,583 subjects. J Am Med Dir Assoc. 21(7):915–918. https://doi.org/10.1016/j.jamda.2020.05.045 (Epub 2020 May 25. PMID: 32674819; PMCID: PMC7247470)
Vermeiren S, Vella-Azzopardi R, Beckwée D (2016) Gerontopole brussels study group frailty and the prediction of negative health outcomes: a meta-analysis. J Am Med Dir Assoc 17:1163.e1-1163.e17
Covino M, Russo A, Salini S, De Matteis G, Simeoni B, Della Polla D, Sandroni C, Landi F, Gasbarrini A, Franceschi F (2021) Frailty assessment in the emergency department for risk stratification of COVID-19 patients aged ≥80 years. J Am Med Dir Assoc 22(9):1845-1852.e1
Castro-Rodrìguez M, Carnicero JA, Garcia-Garcia FJ (2016) Frailty as a major factor in the increased risk of death and disability in older people with diabetes. J Am Med Dir Assoc 17:949–955
Abizanda P, Romero L, Sánchez-Jurado PM (2014) Age, frailty, disability, institutionalization, multimorbidity or comorbidity. Which are the main targets in older adults? J Nutr Health Aging 18:622–627
Laosa O, Pedraza L, Álvarez-Bustos A, Carnicero JA, Rodriguez-Artalejo F, Rodriguez-Mañas L (2020) Rapid assessment at hospital admission of mortality risk from COVID-19: the role of functional status. J Am Med Dir Assoc 21(12):1798-1802.e2. https://doi.org/10.1016/j.jamda.2020.10.002 (Epub 2020 Oct 8. PMID: 33160872; PMCID: PMC7543696)
Fumagalli C, Ungar A, Rozzini R, Vannini M, Coccia F, Cesaroni G, Mazzeo F, D’Ettore N, Zocchi C, Tassetti L, Bartoloni A, Lavorini F, Marcucci R, Olivotto I, Rasero L, Fattirolli F, Fumagalli S, Marchionni N (2021) Predicting mortality risk in older hospitalized persons with COVID-19: a comparison of the COVID-19 mortality risk score with frailty and disability. J Am Med Dir Assoc 22(8):1588-1592.e1. https://doi.org/10.1016/j.jamda.2021.05.028 (Epub 2021 Jul 2. PMID: 34334160; PMCID: PMC8249822)
Heras E, Garibaldi P, Boix M, Valero O, Castillo J, Curbelo Y, Gonzalez E, Mendoza O, Anglada M, Miralles JC, Llull P, Llovera R, Piqué JM (2021) COVID-19 mortality risk factors in older people in a long-term care center. Eur Geriatr Med 12(3):601–607. https://doi.org/10.1007/s41999-020-00432-w (Epub 2020 Nov 27. PMID: 33245505; PMCID: PMC7693854)
Bienvenu LA, Noonan J, Wang X, Peter K (2020) Higher mortality of COVID-19 in males: sex differences in immune response and cardiovascular comorbidities. Cardiovasc Res 116(14):2197–2206. https://doi.org/10.1093/cvr/cvaa284.PMID:33063089;PMCID:PMC7665363
Pradhan A, Olsson PE (2020) Sex differences in severity and mortality from COVID-19: are males more vulnerable? Biol Sex Differ 11(1):53. https://doi.org/10.1186/s13293-020-00330-7.PMID:32948238;PMCID:PMC7498997
Aliberti MJR, Szleif C, Avelino-Silva VI, Suemoto CK, Apolinario D, Dias MB, Garcez FB, Trindade CB, Do Amaral ATJR, De Melo LRS, De Aguiar RC, Coelho PL, Hojaij NHSL, Saraiva MD, Da Silva FCA, Jacob-Filho W, Avelino-Silva TJ, COVID HCFMUSP Study Group (2021) COVID-19 is not over and age is not enough: using frailty for prognostication in hospitalized patients. J Am Geriatr Soc 69(5):1116–1127
Rutten JJS, van Kooten J, van Loon AM, van Buul LW, Joling KJ, Smalbrugge M, Hertogh CMPM (2021) Dementia and Parkinson’s disease: risk factors for 30-day mortality in nursing home residents with COVID-19. J Alzheimers Dis 84(3):1173–1181. https://doi.org/10.3233/JAD-210319.PMID:34542068;PMCID:PMC8673527
Tian W, Jiang W, Yao J, Nicholson CJ, Li RH, Sigurslid HH, Wooster L, Rotter JI, Guo X, Malhotra R (2020) Predictors of mortality in hospitalized COVID-19 patients: a systematic review and meta-analysis. J med virol. https://doi.org/10.1002/JMV.26050
Matta S, Chopra KK, Arora VK (2020) Morbidity and mortality trends of Covid 19 in top 10 countries. Indian J Tuberc 67(4):S167–S172 (Published online 2020 Oct 8)
NICE Guideline. (2020) COVID-19 rapid guideline: critical care in adults. Natl Inst Heal Care Excell. https://www.nice.org.uk/guidance/ng159. Accessed 30 Jul 2020
Hussien H, Nastasa A, Apetrii M, Nistor I, Petrovic M, Covic Adrian (2021) Different aspects of frailty and COVID-19: points to consider in the current pandemic and future ones. BMC Geriatr 21:389 (Published online 2021 Jun 27)
Chinnadurai R, Ogedengbe O, Agarwal P, Money-Coomes S, Abdurrahman AZ, Mohammed S, Kalra PA, Rothwell N, Pradhan S (2020) Older age and frailty are the chief predictors of mortality in COVID-19 patients admitted to an acute medical unit in a secondary care setting- a cohort study. BMC Geriatr 20(1):409
Zhou F, Yu T, Du R, Fan G, Liu Y, Liu Z, **ang J, Wang Y, Song B, Gu X, Guan L, Wei Y, Li H, Wu X, Xu J, Tu S, Zhang Y, Chen H, Cao B (2020) Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet 395(10229):1054–1062
Godaert L, Proye E, Demoustier-Tampere D, Coulibaly PS, Hequet F, Draméb M (2020) Clinical characteristics of older patients: the experience of a geriatric short-stay unit dedicated to patients with COVID-19 in France. J Infect. 81(1):e93–e94 (Published online 2020 Apr 17)
Yu T, Cai S, Zheng Z, Cai X, Liu Y, Yin S et al (2020) Association between clinical manifestations and prognosis in patients with COVID-19. Clin Ther 42(6):964–972
Chen R, Liang W, Jiang M, Guan W, Zhan C, Wang T et al (2020) Risk factors of fatal outcome in hospitalized subjects with coronavirus disease 2019 from a nationwide analysis in China. Chest 158(1):97–105
Lithander FE, Neumann S, Tenison E, Lloyd K, Welsh TJ, Rodrigues JCL, Higgins JPT, Scourfield L, Christensen H, Haunton VJ, Henderson EJ (2020) COVID19 in older people: a rapid clinical review. Age Ageing 49(4):501–515
Lokugamage KG, Hage A, de Vries M, Valero-Jimenez AM, Schindewolf C, Dittmann M et al (2020) Type I interferon susceptibility distinguishes SARS-CoV-2 from SARS-CoV. J Virol 94:e01410-e1420
Grifoni A, Weiskopf D, Ramirez SI, Mateus J, Dan JM, Moderbacher CR, Rawlings SA, Sutherland A, Premkumar L, Jadi RS, Marrama D, de Silva AM, Frazier A, Carlin AF, Greenbaum JA, Peters B, Krammer F, Smith DM, Crotty S, Sette A (2020) Targets of T Cell Responses to SARS-CoV-2 Coronavirus in Humans with COVID-19 Disease and Unexposed Individuals. Cell 181(7):1489-1501.e15
Lu W, Mehraj V, Vyboh K, Cao W, Li T, Routy JP (2015) CD4:CD8 ratio as a frontier marker for clinical outcome, immune dysfunction and viral reservoir size in virologically suppressed HIV-positive patients. J Int AIDS Soc 18:20052
Triggle CR, Bansal D, Hong Ding MD, Islam M, Farag EABA, Hadi HA, Ali A, Sultan A (2021) Comprehensive review of viral characteristics, transmission, pathophysiology, immune response, and management of SARS-CoV-2 and COVID-19 as a basis for controlling the pandemic. Front Immunol 12:631139
Mirzaei R, Goodarzi P, Asadi M, Soltani A, Aljanabi HAA, Jeda AS, Dashtbin S, Jalalifar S, Mohammadzadeh R, Teimoori A, Tari K, Salari M, Ghiasvand S, Kazemi S, Yousefimashouf R, Keyvani H, Karampoor S (2020) Bacterial co-infections with SARS-CoV-2. IUBMB Life 72(10):2097–2111
Manohar P, Loh B, Nachimuthu R, Hua X, Welburn SC, Leptihn S (2020) Secondary bacterial infections in patients with viral pneumonia. Front Med (Lausanne) 5(7):420
Acknowledgements
The study is non-profit and is aimed at improving clinical practice and as such is considered an integral part of health care. The ownership of the data related to the study, its execution and its results belong to the structure that acts as promoter and the results of the study will be published by autonomous decision of the same.
Funding
No external source of funding was received for the present article.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All the authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human partecipants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
For this type of study formal consent is not required.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Pagliuca, R., Cupido, M.G., Mantovani, G. et al. Absence of negativization of nasal swab test and frailty as risk factors for mortality in elderly COVID-19 patients admitted in long-term care facilities. Eur Geriatr Med 13, 933–939 (2022). https://doi.org/10.1007/s41999-022-00657-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s41999-022-00657-x