Abstract
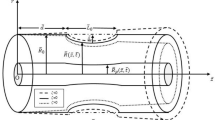
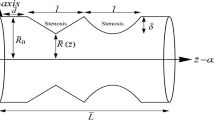
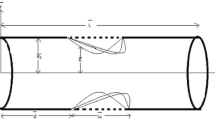
This study analyses the rheological characteristics of non-Newtonian Carreau fluid model for nanoparticles suspended flow of blood through constricted arteries in the presence of stenosis, thrombosis and catheters. Analytical expressions, such as, velocity distribution, temperature, pressure gradient, wall shear stress and resistive impedance to flow are obtained by implementing the perturbation method and through the extensive use of MATLAB and MATHEMATICA programming tools, the results are presented graphically and tabularly. It is found that temperature of the fluid lessens with the increase in stenosis shape parameter and depth of stenosis which results in the reduction of flow of blood in the artery. It is discovered that a rise in Weissenberg number results in the decrease of fluid’s velocity and skin friction. The magnitude of resistance to blood flow reduces with the upsurge of flow rate and stenosis shape parameter and the reverse character is recognized when Weissenberg number, the depth and axial displacement of blood clot increases. When the angioplasty catheter of radius 0.3 is inserted to the clear the constrictions in the artery, the resistance to flow surges considerably in the range of 6.75–8.78 when the stenosis position extends in the axial direction from 0.1 to 0.3. It is also recorded that when the catheter guidewire radius is 0.18, the pressure gradient in blood flow is found to vary in the range of 1.21–1.43 when the axial variable z varies from 0.2 to 0.8 and it decreases from 1.36 to 1.32 when the blood clot position displaces from 0.2 to 0.6.









Similar content being viewed by others
Availability of data and material
Not applicable.
Abbreviations
- L:
-
Length of the artery
- R:
-
Non-stenotic radius of outer tube
- K :
-
Thermal conductivity
- T :
-
Temperature
- S :
-
Stress tensor
- Q:
-
Flow rate
- Gr:
-
Grashof number
- We:
-
Weissenberg number
- \(\left( {{\bar{r}},{\bar{z}}} \right) \) :
-
Cylindrical Coordinates
- \(\left( {{\bar{u}},{\bar{w}}} \right) \) :
-
Radial, Axial velocity
- \(n\left( { \ge 2} \right) \) :
-
Multiple stenosis shape parameter
- \(q/\frac{{\partial p}}{{\partial z}}\) :
-
Pressure gradient
- a:
-
Location of the stenosis
- b:
-
Length of the stenosis
- c:
-
Catheter radius
- m:
-
Power law index
- \(\delta \) :
-
Maximum stenotic depth
- g:
-
Gravity
- p:
-
Fluid’s pressure
- \(\Pi \) :
-
Second invariant of stress tensor
- \(\eta \) :
-
Outer wall of artery
- \(\epsilon \) :
-
Inner wall of artery
- \(\beta \) :
-
Dimensionless heat source or sink parameter
- \(\theta \) :
-
Temperature
- \(\zeta \) :
-
Maximum height attained by the clot
- \(\gamma \) :
-
Thermal expansion coefficient
- \(\rho \) :
-
Density
- \(\mu \) :
-
Viscosity
- \(\phi \) :
-
Nanofluid volume fraction
- nf:
-
Nanofluid
- f:
-
Base fluid
- s:
-
Metallic nanoparticles
- d:
-
Displacement
- \({c_p}\) :
-
Heat capacity
References
Sweed, N., Mekheimer, K.S., EL-Kholy, A., Abdelwahab, A.: Alterations in pulsatile bloodstream with the heat and mass transfer through asymmetric stenosis artery: erythrocytes suspension model. Heat Transf. 50(3), 2259–2287 (2021)
Ponalagusamy, R.: Blood flow through stenosed tube. Ph.D. Dissertation, Ph.D Thesis, IIT, Bombay, India (1986)
Liepsch, D., Singh, M., Lee, M.: Experimental analysis of the influence of stenotic geometry on steady flow. Biorheology 29(4), 419–431 (1992)
Al-Saad, M., Suarez, C., Obeidat, A., Bordas, S., Kulasegaram, S.: Application of smooth particle hydrodynamics method for modelling blood flow with thrombus formation. Comput. Model. Eng. Sci. 122(3), 831–862 (2020)
Jackson, S.P.: Arterial thrombosis—insidious, unpredictable and deadly. Nat. Med. 17(11), 1423–1436 (2011)
Elnaqeeb, T., Mekheimer, K.S., Alghamdi, F.: Cu-blood flow model through a catheterized mild stenotic artery with a thrombosis. Math. Biosci. 282, 135–146 (2016)
Young, D.F., Tsai, F.Y.: Flow characteristics in models of arterial stenoses—I. Steady flow. J. Biomech. 6(4), 395–410 (1973)
MacDonald, D.: On steady flow through modelled vascular stenoses. J. Biomech. 12(1), 13–20 (1979)
Chaturani, P., Samy, R.P.: Pulsatile flow of Casson’s fluid through stenosed arteries with applications to blood flow. Biorheology 23(5), 499–511 (1986)
Afiqah, W.S., Sankar, D.S.: Effects of porosity in four-layered non-linear blood rheology in constricted narrow arteries with clinical applications. Comput. Methods Progr. Biomed. 199, 105907 (2021)
Kumawat, C., Sharma, B.K., Mekheimer, K.S.: Mathematical analysis of two-phase blood flow through a stenosed curved artery with hematocrit and temperature dependent viscosity. Phys. Scr. 96(12), 125277 (2021)
Karino, T., Goldsmith, H.L.: Flow behaviour of blood cells and rigid spheres in an annular vortex. Philos. Trans. R. Soc. Lond. B Biol. Sci. 279(967), 413–445 (1977)
Kapur, J.N.: Mathematical Models in Biology and Medicine. East-West Press Pvt. Ltd., New Delhi (1992)
Mann, K.G., Butenas, S., Brummel, K.: The dynamics of thrombin formation. Arterioscler. Thromb. Vasc. Biol. 23(1), 17–25 (2003)
Sankar, D.S.: Two-phase non-linear model for blood flow in asymmetric and axisymmetric stenosed arteries. Int. J. Non Linear Mech. 46(1), 296–305 (2011)
Choi, S.U.: Nanofluids: from vision to reality through research. J. Heat Transf. 131(3), 033106 (2009)
Tyler, T., Shenderova, O., Cunningham, G., Walsh, J., Drobnik, J., McGuire, G.: Thermal transport properties of diamond-based nanofluids and nanocomposites. Diam. Relat. Mater. 15(11–12), 2078–2081 (2006)
Das, S.K., Choi, S.U., Patel, H.E.: Heat transfer in nanofluids—a review. Heat Transf. Eng. 27(10), 3–19 (2006)
Liu, M.S., Lin, M.C.C., Huang, I.T., Wang, C.C.: Enhancement of thermal conductivity with carbon nanotube for nanofluids. Int. Commun. Heat Mass Transf. 32(9), 1202–1210 (2005)
Nsofor, E.C.: Recent patents on nanofluids (nanoparticles in liquids) heat transfer. Recent Pat. Mech. Eng. 1(3), 190–197 (2008)
Afiqah, W.S., Sankar, D.S.: Two-phase nonlinear rheological analysis of blood flow in small diameter blood vessels with constriction. ARPN J. Eng. Appl. Sci. 15(10), 1129–1143 (2020)
Khan, M.I., Alzahrani, F., Hobiny, A.: Heat transport and nonlinear mixed convective nanomaterial slip flow of Walter-B fluid containing gyrotactic microorganisms. Alex. Eng. J. 59(3), 1761–1769 (2020)
Bugliarello, G., Hayden, J.W.: Detailed characteristics of the flow of blood in vitro. Trans. Soc. Rheol. 7(1), 209–230 (1963)
Bugliarello, G., Sevilla, J.: Velocity distribution and other characteristics of steady and pulsatile blood flow in fine glass tubes. Biorheology 7(2), 85–107 (1970)
Cokelet, G.: The rheology of human blood. In: Biomechanics: Its Foundations and Objectives (1972)
Shukla, J., Parihar, R., Rao, B.: Effects of stenosis on non-Newtonian flow of the blood in an artery. Bull. Math. Biol. 42(3), 283–294 (1980)
Priyadharshini, S., Ponalagusamy, R.: Computational model on pulsatile flow of blood through a tapered arterial stenosis with radially variable viscosity and magnetic field. Sadhana 42(11), 1901–1913 (2017)
Yilmaz, F., Gundogdu, M.Y.: A critical review on blood flow in large arteries; relevance to blood rheology, viscosity models, and physiologic conditions. Korea Aust. Rheol. J. 20(4), 197–211 (2008)
Zaman, A., Ali, N., B’eg, O.A.: Unsteady magnetohydrodynamic blood flow in a porous-saturated overlap** stenotic artery-numerical modeling. J. Mech. Med. Biol. 16(4), 1650049 (2016)
Haghighi, A.R., Asl, M.S., Kiyasatfar, M.: Mathematical modeling of unsteady blood flow through elastic tapered artery with overlap** stenosis. J. Braz. Soc. Mech. Sci. 37(2), 571–578 (2015)
Barnes, H.A., Hutton, J.F., Walters, K.: An Introduction to Rheology, vol. 3. Elsevier, Amsterdam (1989)
Zaman, A., Ali, N., Sajid, M., Hayat, T.: Effects of unsteadiness and nonnewtonian rheology on blood flow through a tapered time-variant stenotic artery. AIP Adv. 5(3), 037129 (2015)
Nadeem, S., Ijaz, S., Akbar, N.S.: Nanoparticle analysis for blood flow of Prandtl fluid model with stenosis. Int. Nano Lett. 3(1), 1–13 (2013)
Ellahi, R., Rahman, S., Nadeem, S., Akbar, N.S.: Blood flow of nanofluid through an artery with composite stenosis and permeable walls. Appl. Nanosci. 4(8), 919–926 (2014)
Ahmed, A., Nadeem, S.: The study of (Cu, TiO2, Al2O3) nanoparticles as antimicrobials of blood flow through diseased arteries. J. Mol. Liq. 216, 615–623 (2016)
Mekheimer, K.S., Elnaqeeb, T., El Kot, M., Alghamdi, F.: Simultaneous effect of magnetic field and metallic nanoparticles on a micropolar fluid through an overlap** stenotic artery: blood flow model. Phys. Essays 29(2), 272–283 (2016)
Mekheimer, K.S., Mohamed, M.S., Elnaqeeb, T.: Metallic nanoparticles influence on blood flow through a stenotic artery. Int. J. Pure. Appl. Math. 107(1), 201 (2016)
Nadeem, S., Ijaz, S.: Influence of metallic nanoparticles on blood flow through arteries having both stenosis and aneurysm. IEEE Trans. Nanobiosci. 14(6), 668–679 (2015)
Akbar, N.S.: Metallic nanoparticles analysis for the blood flow in tapered stenosed arteries: application in nanomedicines. Int. J. Biomath. 9(1), 1650002 (2016)
Nadeem, S., Ijaz, S.: Study of radially varying magnetic field on blood flow through catheterized tapered elastic artery with overlap** stenosis. Commun. Theor. Phys. 64(5), 537 (2015)
Zidan, A., McCash, L., Akhtar, S., Saleem, A., Issakhov, A., Nadeem, S.: Entropy generation for the blood flow in an artery with multiple stenosis having a catheter. Alex. Eng. J. 60(6), 5741–5748 (2021)
Ramadan, S.F., Mekheimer, Kh.S., Bhatti, M.M., Moawad, A.M.A.: Phan-Thien-Tanner nanofluid flow with gold nanoparticles through a stenotic electrokinetic aorta: a study on the cancer treatment. Heat Transf. Res. 52(16), 87–99 (2021)
Elogail, M.A., Mekheimer, Kh.S.: Modulated viscosity-dependent parameters for MHD blood flow in microvessels containing oxytactic microorganisms and nanoparticles. Symmetry 12(12), 2114 (2020)
Zhang, L., Bhatti, M.M., Marin, M., Mekheimer, Kh.S.: Entropy analysis on the blood flow through anisotropically tapered arteries filled with magnetic zinc-oxide (ZnO) nanoparticles. Entropy 22(10), 1070 (2020)
Abdelsalam, S.I., Mekheimer, Kh.S., Zaher, A.Z.: Alterations in blood stream by electroosmotic forces of hybrid nanofluid through diseased artery: aneurysmal/stenosed segment. Chin. J. Phys. 67, 314–329 (2020)
Ramadan, S.F., Mekheimer, K.S.: New insight into gyrotactic microorganisms in anti-infection agents through wavy deformable catheter/endoscope with non-linear thermal radiation: numerical study. J. Adv. Res. Fluid Mech. Therm. Sci. 75(3), 25–42 (2020)
Ijaz, S., Nadeem, S.: Transportation of nanoparticles investigation as a drug agent to attenuate the atherosclerotic lesion under the wall properties impact. Chaos Solitons Fractals 112, 52–65 (2018)
Nadeem, S., Fuzhang, W., Alharbi, F.M., Sajid, F., Abbas, N., El-Shafay, A.S., Al-Mubaddel, F.S.: Numerical computations for Buongiorno nano fluid model on the boundary layer flow of viscoelastic fluid towards a nonlinear stretching sheet. Alex. Eng. J. 61(2), 1769–1778 (2022)
Ahmad, S., Khan, M.N., Nadeem, S.: Unsteady three dimensional bioconvective flow of Maxwell nanofluid over an exponentially stretching sheet with variable thermal conductivity and chemical reaction. Int. J. Ambient. (2022). https://doi.org/10.1080/01430750.2022.2029765
Muhammad, N., Nadeem, S., Khan, U., Sherif, E.-S.M., Issakhov, A.: Insight into the significance of Richardson number on two-phase flow of ethylene glycol-silver nanofluid due to Cattaneo–Christov heat flux. Waves Random Complex Media (2021). https://doi.org/10.1080/17455030.2021.2011470
Nadeem, S., Haq, R.U., Khan, Z.H.: Heat transfer analysis of waterbased nanofluid over an exponentially stretching sheet. Alex. Eng. J. 53(1), 219–224 (2014)
Nadeem, S., Ijaz, S.: Theoretical analysis of metallic nanoparticles on blood flow through stenosed artery with permeable walls. Phys. Lett. A 379(6), 542–554 (2015)
Sheikholeslami, M., Ganji, D.D., Javed, M.Y., Ellahi, R.: Effect of thermal radiation on magnetohydrodynamics nanofluid flow and heat transfer by means of two phase model. J. Magn. Magn. Mater. 374, 36–43 (2015)
Back, L.: Estimated mean flow resistance increase during coronary artery catheterization. J. Biomech. 27(2), 169–175 (1994)
Sankar, D.S.: A two-fluid model for pulsatile flow in catheterized blood vessels. Int. J. Non Linear Mech. 44(4), 337–351 (2009)
Funding
Not applicable.
Author information
Authors and Affiliations
Contributions
AWS perceived the research problem, formulated it as mathematical model and contributed in obtaining the analytical solutions and also take part in develo** MATLAB code for generating data for plotting the graphs and then analyzing the results. DSS contributed in obtaining the expressions for rheological quantities and involved in generating the data for plotting the graphs through MATLAB programming and analysed and validated the results. AKN analysed and validated the results. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Code availability
Not applicable.
Conflict of interest
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Wajihah, S.A., Sankar, D.S. & Nagar, A.K. Effects of Catheter, Stenosis and Thrombosis in Non-Newtonian Blood Flow Through Narrow Arteries with Clinical Applications: A Mathematical Model. Int. J. Appl. Comput. Math 8, 136 (2022). https://doi.org/10.1007/s40819-022-01335-z
Accepted:
Published:
DOI: https://doi.org/10.1007/s40819-022-01335-z