Abstract
Background and Objectives
Fentanyl is a synthetic opioid commonly used as an anesthetic and also increasingly popular as a sedative agent in neonates. Initial dosage regimens in this population are often empirically derived from adults on a body weight basis. However, ontogenic maturation processes related to drug disposition are not necessarily always body weight correlates. We developed a predictive pharmacokinetic/pharmacodynamic model that includes growth and maturation physiologic changes for fentanyl in neonatal care.
Methods
Key pharmacokinetic variables and principles (protein binding, clearance, distribution) as related to fentanyl pharmacokinetic/pharmacodynamic behavior in adults (tricompartmental model) and to neonatal physiologic data (organ weights and blood flows, body composition, renal and hepatic function, etc.) were used to guide the building of a semi-physiologic ontogenic model. The model applies to a normal-term neonate without any other intervention. Then, extension to a pharmacokinetic/pharmacodynamic link model for fentanyl was made. The final model was evaluated by predicting the time course of plasma concentrations and the effect of a standard regimen of 10.5 μg/kg over a 1-h period followed by 1.5 μg/kg/h for 48 h.
Results
Hepatic clearance was linked to ontogeny of unbound fraction and of α1-acid glycoprotein. All parameters were reduced in the neonate compared to adults but in a differing proportion due to qualitative changes in physiology that are analyzed and accounted for. Systemic clearance (CLS), volume of the central compartment (V1) and steady-state volume of distribution predicted by the model were 0.028 L/min, 1.26 L, and 22.04 L, respectively. Weight-corrected parameters generally decreased in adults compared with neonates, but differentially, e.g., CLS = 0.0093 versus 0.0088 L/min/kg, while V1 = 0.42 versus 0.18 L/kg (neonates vs. adults). Under such complexity a pharmacokinetic/pharmacodynamic model is the appropriate method for rational efficacy targeting. Fentanyl pharmacodynamics in neonates were considered to be similar to those in adults except for the equilibrium rate constant, which was also scaled on an ontogenic basis. The model adequately predicted the reported mean expected concentration–time profiles for the standard regimen.
Conclusions
Integrated pharmacokinetic/pharmacodynamic modeling showed that the usually prescribed dosage regimens of fentanyl in neonates may not always provide the optimum degree of sedation. The model could be used in optimal design of clinical trials for this vulnerable population. Prospective clinical testing is the reasonable next step.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
1 Introduction
Fentanyl is a synthetic opioid that has traditionally served as a coadjutant in surgical anesthesia. Due to the analgesic and sedative effects attributed to fentanyl, its use as continuous infusion has expanded in recent years to the field of prolonged sedation in patients undergoing mechanical ventilation. In these circumstances, sedation is aimed at minimizing intubation-derived pain and stress, with the final objective of avoiding agitation, cardiopulmonary instability, patient-ventilator asynchrony, and/or accidental extubation [1–3].
Despite the existing controversy regarding selection of either morphine or fentanyl within this indication, the superiority of fentanyl seems to be supported by its relatively wide margin of safety, blockade of hormonal responses to stress, and preservation of hemodynamic stability, even at high doses [2]. Similarly, the differences in chemical characteristics (500-fold higher lipid solubility) and receptor binding of fentanyl, compared with morphine, enable easier access to the central nervous system (CNS) and a more rapid onset of both analgesic and sedative effects [4].
The need for mechanical ventilation is especially frequent in neonates and infants, who are more prone to diseases such as severe pulmonary immaturity, respiratory distress syndrome, bronchopulmonary dysplasia, or neonatal apnea [3]. However, the fentanyl indication does not include administration in infants. In clinical practice, initial dosing regimens are empirically derived from those employed in adults using linear extrapolations, generally based on body weight, but this can lead either to therapeutic failure or to an increase in adverse events. In their response to drugs, children do not differ from the adult population only because of weight, so they should not be considered simply as an adult ‘miniature model’.
Growth is accompanied by a series of physiologic changes associated with maturation of kidney and liver functions, body composition, and expression of receptors and proteins, among others. These developmental changes, which do not correlate solely with body weight due to their non-linear dynamic nature, may affect drug disposition by modifying either the relationship between dose and exposure (pharmacokinetics) and/or the relationship between exposure and response (pharmacodynamics) [5–7]. In order to predict drug disposition in children and estimate the appropriate initial doses for each pediatric subset prior to administration, the pharmacokinetic/pharmacodynamic information available in adults or in other age groups for the specific drug should be integrated with those developmental changes associated with growth and maturation (ontogeny) [7, 8].
Among the various approaches available for extrapolating or predicting pharmacokinetics in the pediatric population, semi-physiologically based modeling combines all these factors as a more mechanistic and accurate option than allometry based on weight or body surface area, even when corrected by enzyme maturation [9–11]. The semi-physiologic method not only includes the subject’s demographic, physiologic and biologic information and physicochemical properties of the drug, but also makes the most of in vitro-obtained data. As all of the interferences between developmental changes and the aspects involved in drug disposition (organ weight and blood perfusion, body composition, membrane permeability, protein binding, renal maturation, enzyme and transporter ontogeny, etc.) are considered, it is possible to examine the existing differences from adults to each pediatric age range with regard to the absorption, distribution, metabolism, and elimination (ADME) processes [8, 12]. The greatest advantage derived from the use of such models is that studies in children become more confirmatory and less exploratory, thus contributing to providing safe and effective treatments for this vulnerable population [13].
To date, there is no report applying the semi-physiologic approach to fentanyl, although this kind of model has already been developed for other commonly used analgesic and sedative agents, such as morphine [14], midazolam [10], and propofol [15].
The objective of this work was to integrate fentanyl compartmental pharmacokinetic/pharmacodynamic model structures with a pharmacologically guided selection of components associated with postnatal age and known to affect the maturation dependence of the model’s structural parameters. The final purpose was to build a maturation physiology based predictive model for fentanyl disposition and clinical outcome when administered for analgesia and/or sedation in neonates.
2 Methods
2.1 Estimation of Neonatal Pharmacokinetic and Pharmacodynamic Parameters
Pharmacologic principles taken from our experience were used to guide the focus on the key intrinsic processes affecting fentanyl disposition, which are linked to maturation. Age-dependent scales were then built. The system of relations was expected to be intrinsically explicative of less physiologic, compartmental pharmacokinetic parameters in adults. The link to pharmacodynamics was similarly performed based on pharmacology.
All model building was performed within a mixed-effects framework (NONMEM®, version 6.2, GloboMax LLC, Hanover, MD, USA) so as to permit maximum flexibility in separating sources of variability (inter and within patient) crucial for the individualization effort based on intrinsic processes and parameters. This kind of industry-standard pharmacostatistical modeling platform is essential for future confirmation of the model with observational data in neonatal fentanyl treatment.
2.1.1 Pharmacokinetics
A three-compartment pharmacokinetic model previously defined for adults [16–18] was assumed to best describe fentanyl disposition at all ages (Fig. 1).
Tricompartmental mammillary pharmacokinetic model representation describing the time course of fentanyl plasma concentrations, Cp(t) [measured in the central compartment]. CL S systemic clearance, CL d intercompartmental (distributional) clearance, k 10 elimination rate constant, k 12 transfer rate constant from the central compartment to the peripheral distribution compartment, k 21 transfer rate constant from the peripheral distribution compartment to the central compartment, k 13 transfer rate constant from the central compartment to the deep distribution compartment, k 31 transfer rate constant from the deep distribution compartment to the central compartment, Q 1–2 and Q 1–3 intercompartmental clearances, V 1 volume of the central compartment, V 2 volume of the peripheral distribution compartment, V 3 volume of the deep distribution compartment, V ss steady-state volume of distribution
The procedure followed in this study to estimate the pharmacokinetic parameters for fentanyl in neonates is schematically depicted in Fig. 2. The parameters and relations created for each component of disposition were compared with the literature at each step.
2.1.2 Pharmacodynamics
Pharmacodynamic models relate blood concentration with the pharmacologic effect, which can generally be done in a direct or linear fashion for the majority of drugs. The sigmoid maximum effect (Emax) model is the most commonly used for opioids. However, when pharmacologic effects show a temporal delay with respect to plasma concentrations, it is necessary to introduce an ‘indirect link’ pharmacokinetic/pharmacodynamic model (also known as the effect-compartment model) describing the movement of drug from plasma to the biophase through a first-order equilibrium rate constant (ke0) [19]. The effect compartment is a separate pharmacokinetic compartment where drug concentration (Ce), although not readily measurable, is directly proportional to the pharmacologic effect. The steady-state equilibration half-life between plasma and the effect compartment (t½_ke0) quantifies the temporal lag or hysteresis between concentration and effect [17].
2.1.3 Parameter Pharmacology
The validity of the pharmacokinetic and pharmacodynamic parameters as obtained for neonates is analyzed from a physiologic and pharmacologic perspective, compared with adult physiology and with literature.
2.2 Model Evaluation
A preliminary comparison of two global output pharmacokinetic parameters, systemic clearance (CLS) and steady-state volume of distribution (Vss), was performed with the fentanyl literature. It was not possible to compare with the remaining parameters because of the lack of compartmental models in neonates.
Simulations using the physiology-dependent pharmacokinetic/pharmacodynamic model were compared with fentanyl concentration and effect time evolution profiles in the literature. The fentanyl plasma concentration (Cp) and sedative effect time course were simulated for 150 neonates under a standard dosing regimen (10.5 μg/kg over a 1-h period followed by 1.5 μg/kg/h for 48 h) [20]. The simulation reproduces the expected variability due to variation in the pharmacokinetic parameters only (no sampling noise included) for 2-day-old term newborns of 3-kg body weight. The variability applied to physiologic variables and calculated mean pharmacokinetic (CLS and Vss) and pharmacodynamic parameters (concentration producing 50 % maximum effect [EC50] and ke0) was taken from published reports [21, 22]. The 95 % confidence interval of the simulated concentration–time profiles of fentanyl were calculated and displayed in comparison with the target EC50.
3 Results
3.1 Estimation of Neonatal Pharmacokinetic and Pharmacodynamic Parameters
The fentanyl pharmacokinetic characteristics and parameters in adults are listed in Table 1. Physiologic variables involved in fentanyl disposition (organ weights and blood flows, body composition, renal and hepatic function, etc.) for the average 2-day-old term newborn and for the average adult are shown in Table 2.
3.1.1 Pharmacokinetics
As depicted in Fig. 2, the CLS of fentanyl is an additive function of the mechanisms involved in its elimination from the body, i.e., hepatic (cytochrome P450 [CYP] 3A4) clearance (CLH), which metabolizes 94 % of the dose in adults (CLH = 0.94 × CLS) and renal clearance (CLR), which accounts for the remaining 6 % (CLR = 0.06 × CLS); CLS = CLH + CLR [33]. Implied routes are thought to be conserved across ages because fentanyl seems not to be a substrate for the fetal isoform CYP3A7 [24]. This allowed calculation of CLS in neonates by combining the adult data that served as a starting point with developmental changes [10].
Fentanyl is not subject to active tubular secretion or reabsorption; hence, CLR is proportional to the glomerular filtration rate (GFR). CLR was scaled from adults to neonates, as shown in Eq. 1 [34]:
where fu is the unbound fraction of fentanyl, described as 0.160 in adults [23] (see also Table 2).
The fu for neonates was calculated as a function of the α1-acid glycoprotein (AAG) plasma concentration, as in Eq. 2 [12, 23]:
The affinity of AAG for fentanyl was assumed to be constant and independent of age, while drug binding to other plasma proteins such as albumin or lipoprotein was disregarded, due to their minimal contribution. AAG is known to be 0.77 g/L [29, 30] in adults (see also Table 2) and was calculated for neonates according to Eq. 3 [12], where AAG is in g/L and age is in days:
CLH is proportional to intrinsic clearance (CLint), to liver blood flow (QH), and to the degree of protein binding as only the free fraction is able to cross cellular membranes [13, 33, 35]. CLint is a measure of enzyme activity and QH accounts for arrival of drug to the liver.
The predictive relationship of CLH in adults is shown in Eq. 4 [10, 12, 34], where, for fentanyl, blood clearance was considered to be equivalent to plasma clearance under the assumption that the blood:plasma ratio is equal to unity.
Each of the terms follows its own maturation pattern during development. Here, CLint (the unbound clearance) depends on liver weight and is one of the variables subject to developmental changes. The adult intrinsic clearance (CLint_adult) was obtained by solving Eq. 4. CLint_adult was then normalized by liver weight (L/min/g of liver) in order to allow scaling to neonates.
Two dimensionless correction factors related to hepatic ontogeny were used to scale the intrinsic clearance in neonates (CLint_neonate). One factor accounted for liver weight (growth) (GLW) and another described the percentage of adult CYP3A4 enzyme activity (FCYP) estimated to be present in neonates [27, 34, 35]. The calculation was as shown in Eq. 5:
where GLW = 130/1,800 = 0.072 (where 130 and 1,800 g are the newborn and adult liver weights, respectively [28]; see also Table 2) and FCYP = 20 % [27, 34].
The neonatal CLH was then calculated using the values in Table 2, and the neonatal fu from Eq. 2 and CLint from Eq. 5 (see also Table 2 for specific predictor parameter values). Finally, the neonatal CLS was obtained using Eq. 6:
Regarding apparent volume of distribution (Vd), semi-physiologic methods relate changes in Vd from birth to adulthood to the changes in body composition. In line with this, and based on observations made in adults, volumes of the central (V1) and peripheral distribution (V2) compartments were assumed to resemble extracellular water content and total body water, respectively, at all ages. The remaining distribution parameters, volume of the deep distribution compartment (V3) and Vss, were approached from the estimated value for V1 and V2, under the assumption that both the (V1 + V2)/Vss and V3/Vss ratios are age independent.
Intercompartmental clearances (Q1–2 and Q1–3, which are equivalent to Q2–1 and Q3–1, respectively) were related to cardiac output in adults. This is justified by the fact that they ultimately depend on blood perfusion. The observed proportion (close to 70 and 30 % of cardiac output for Q1–2 and Q1–3, respectively) was considered to age-independently serve as a basis for calculation of these parameters in neonates.
3.1.2 Pharmacodynamics
The ke0 and t½_ke0 described for fentanyl in adults are 0.11 min−1 and 6.3 min, respectively [36–38]. After contrasting the ke0 in adults against physiologic parameters, it was found that it may be approached using the ratio between brain-blood flow and cardiac output. The ratio was then applied to scale the magnitude of ke0 in neonates.
After hysteresis minimization, the relationship between biophase concentration (Ce) and effect (E) was analyzed with the Hill relation, as shown in Eq. 7:
where E0 represents the baseline value of the effect measure (in this case, 0 for the degree of sedation) and Emax the maximum possible effect (100 % was considered in this case). EC50 is the steady-state concentration value, thus equivalent in plasma and biophase, that leads to half the maximum effect, hence serving to define the intrinsic potency of the drug, and γ is the Hill exponent that determines the steepness or slope of the concentration–response curve and is related to the number of receptor binding sites.
Based on the evidence suggesting that endogenous opioid receptors may be completely functional in the immature nervous system and, consequently, at birth [2], the pharmacodynamics were considered to be independent of age, so that the same Emax, EC50 and γ values described for fentanyl in adults, i.e., 100 %, 3 μg/L, and 2, respectively, were applied to neonates. The EC50 value [18, 39, 40] was supported by the previous finding that the mean morphine concentration required to produce adequate sedation in 50 % of neonates is 125 ng/mL [14], given that the potency of fentanyl is known to be around 50 times that of morphine as an opioid receptor agonist. For the Hill exponent, despite being described as close to 4 when fentanyl is utilized for anesthetic purposes, a γ = 2 was assumed when used as an analgesic/sedative agent [17, 18]. The decision was also on the basis of previous knowledge of the drug and preclinical data considered to correlate well with behavior in humans [41, 42].
3.2 Parameter Pharmacology
The physiologic variables and parameters calculated according to our approach for a typical neonate (2 days) and used in building the maturation-dependent pharmacokinetic/pharmacodynamic model for fentanyl are shown in Table 3. The equivalent body weight parameters for adults and neonates are listed in Table 4.
The estimated fu of fentanyl in neonatal blood (0.31) is higher than that in adults (0.16), as a consequence of the lower circulating concentration of AAG, the main fentanyl binding protein at all ages. AAG concentrations in term neonates are about half of those in adults (0.32 vs. 0.77 g/L, respectively). The affinity constant has been assumed to be similar in infants and adults, which appears to be well founded for most drugs [12, 23].
The estimated CLS corresponds to the sum of CLR and hepatic CLH. Despite its insignificant contribution to the overall CLS in adults, it was decided to include CLR because it is subject to ontogenic changes that are independent of the hepatic maturation. As observed in Tables 1 and 3, the CLS (L/min) estimated from the neonatal model was lower than that in adults (i.e., 4.5 % of the adult value), whereas Vss is in the order of 6 % of the adult value, this percentage reaching 9.6 % in the case of V1. Regarding intercompartmental clearances, both Q1–2 and Q1–3 showed a comparable trend with respect to adults (i.e., around 8 % of the adult value). However, body weight-corrected parameters showed the opposite trend (decreasing with increasing age) (Table 4).
As fast receptor association/dissociation kinetics have been observed in vitro for fentanyl [43], the delay between the fentanyl Cp and pharmacologic effect is due to biophase distribution kinetics. The calculated value for ke0 in neonates was 0.31 min−1 as compared with 0.11 min−1 in adults, whereas the corresponding value for t½_ke0 was 2.23 min, far less than that in adults (6.3 min). In neonates, where brain–blood flow represents a larger fraction of cardiac output, faster fentanyl access to the CNS is expected as reflected in the reduced t½_ke0.
3.3 Model Evaluation
Global pharmacokinetic parameters CLS and Vss calculated for the model were in the range of those described for fentanyl in the scarce neonatal literature (Table 5).
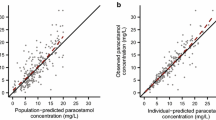
Figure 3 shows the simulated pharmacokinetic profile range from 150 neonatal patients using the pharmacokinetic portion of the developed physiology-based model and a standard regimen. The parameters are those shown in Table 3. The average Cp curve from the neonatal literature is very close to the average profile predicted by the physiology-dependent model, thus confirming the predictive capacity of the model within this population. It should be noted, however, that those averages are below the putative EC50 target of 3 μg/L fentanyl (at equilibrium with the effect site) most of the time. Interestingly, the pharmacodynamic portion of the simulations (Fig. 4) shows that, after the same standard protocol, an important percentage of neonates would not achieve the desired degree of sedation (50 % Emax) for prolonged periods of time.
Simulation from parameter variability of the time course of fentanyl plasma concentrations (Cp) after a standard dosing regimen of 10.5 μg/kg over a 1-h period followed by 1.5 μg/kg/h for 48 h. The mean (solid curve), upper and lower 95 % confidence interval (shaded region) for 150 term newborns of 3 kg weight is shown. The typical average observed concentrations [20] for the same regimen is overlaid (black dots). The vertical dash-dot line marks the stop of infusion and the horizontal dashed line is the putative target concentration producing 50 % maximum effect
Simulation of the effect–time course corresponding to the plasma concentrations depicted in Fig. 3. The mean analgesia/sedation effect (solid curve) and upper and lower 95 % confidence interval (shaded region) for 150 term newborns of 3 kg weight are shown. E max maximum effect
4 Discussion
It has been widely acknowledged that neonates may experience adverse short- and long-term consequences of pain and distress associated with procedures in the intensive care setting [1, 3]. In order to reduce behavioral, biochemical, and physiologic responses to these stimuli, pharmacologic intervention producing analgesia or sedation is crucial. Drugs such as fentanyl, whose appropriate dosage can be predicted, are preferable [47].
In this context, given the high inherent vulnerability of neonates, any model that provides greater insight into the dose–response relationship in this subpopulation is of interest. This is more so due to the common practice of extrapolating regimens from adults on a body weight basis [1–3].
No semi-physiologic model has been developed for fentanyl—to the best of our knowledge—although this kind of model has already been developed for other commonly used analgesic and sedative agents such as morphine [14]. This may reflect the historically more frequent use of morphine in neonatal units as compared with fentanyl. However, morphine is being displaced by fentanyl due to fentanyl’s favorable pharmacologic characteristics, i.e., higher predictability of outcomes, wider margin of safety, preservation of hemodynamic stability, and lack of tolerance development [2, 4, 20].
The core pharmacokinetics in neonates were assumed to be represented by a three-compartment model. Earlier observational studies have shown such intermediate complex structure in plasma concentration–time profiles [48]. The assumption is also supported by preclinical data showing that well-perfused brain, heart, liver, lung, kidneys, and spleen are first exposed to fentanyl, with a posterior redistribution to skeletal muscle and a much slower tertiary distribution to relatively under-perfused tissues, i.e., adipose tissue [49]. Although some reports utilize the bicompartmental model to describe fentanyl pharmacokinetics in children [46, 50], that may be due to the inability of detecting the third compartment (third slope of elimination), probably as a result of the combination of low doses, non-sensitive analytical technique, and/or too short a sampling period [51]. The secondary peaks observed in subjects of a wide range of ages are most likely due to the accumulation of fentanyl in peripheral tissues and the subsequent return to the central compartment [48, 52], and can be attributed to a third modeled compartment.
An extension of the simple compartmental model by including age maturation and physiology-dependent relationship for the model parameters is presented. Thus, a maturation-predictive model is derived for neonates with fentanyl. The method started with basic pharmacokinetic principles regarding those physiologic processes affecting clearance, first distinguishing CLS into its two hepatic and renal components. The clearance components were then expressed as functions of key physiologic variables such as CLint that, in turn, was predicted by fu, AAG, and liver weight. Conscious attention is paid to AAG and binding fraction maturation for fentanyl is linked to that plasma protein, rather than the typically used albumin.
The procedure followed in the development of the model relied on several assumptions corresponding to a term, intervention-free, term newborn. For CLH, these assumptions include the following: (a) microsomal protein per gram of liver (MPPGL) is not influenced by maturation [12, 31, 53] and, therefore, CLint was normalized by liver weight rather than by MPPGL; (b) enzyme kinetics are within the linearity range, so that no saturation process takes place; (c) fentanyl kinetics are not affected by any enzyme inhibitor or inducer; (d) extrahepatic CYP3A4 enzymes do not affect fentanyl metabolism when it is intravenously administered; (e) other isoforms of CYP3A (3A5 and 3A7) do not contribute to fentanyl metabolism; and (f) CLint conversion ratios concern the 100 % active CYP3A4 in adults and neonates.
These assumptions seem to be confirmed by the fact that the predicted pattern for CLint is quite similar to that reported for other active substances primarily metabolized via CYP3A4, such as midazolam [10]. Nevertheless, the CLS values of the two drugs do not match because of their distinct pattern of plasma protein binding and subsequent different repercussions of developmental changes.
While fentanyl is primarily bound to AAG, which is extremely diminished in neonates, midazolam is predominantly bound to albumin, whose percentage of change with respect to adults is considerably less important [23]. Moreover, fentanyl extraction is lower in neonates than in adults (employing the basic relation CLS = Q × E, where Q is blood flow and E is the extraction ratio, Eneonate = 0.14 while Eadult = 0.36). The unbound or free fraction can then be decisive in defining the extent of clearance. Indeed, measurement of the Cp of AAG might help improve clinical practice significantly.
Concerning CLR, calculations performed in this study on the basis of age-related differences in fu and GFR suggest an increased relevance of urinary excretion in neonates, as CLR would account for 14 % of the fentanyl dose compared to 6 % in adults, thus compensating in part the underdeveloped metabolizing activity at birth. However, this should be further evaluated in vivo before a conclusion can be drawn, because, to our knowledge, no report has mentioned the role of CLR in the pharmacokinetics of pediatric fentanyl so far. This finding, together with a proportionally larger liver, higher QH, increased fu, and decreased adipose tissue sequestration in neonates compared with adults [45, 47, 48, 54], may offer a plausible explanation for the predicted CLS that is similar in both neonate and adult populations once normalized for body weight (about 0.008 L/min/kg), despite the enzymatic immaturity in the former.
Notwithstanding, the complexity inherent in the three-compartment model and in this particular drug precludes dosing of fentanyl based on body weight. Unlike other drugs, for which the pharmacokinetics are viewed as monocompartmental, fentanyl disposition is not influenced solely by CLS since the volumes of distribution and elimination half-lives of the additional compartments exert an impact on disposition as well.
Regarding volumes of distribution, the physiology-dependent model calculated values for V1 and Vss (in both cases higher in neonates than in adults when normalized by body weight) are consistent with previous observations described for fentanyl in the literature [45, 48, 54], and also with those published for other lipid-soluble drugs of a similar octanol–water partition coefficient (logP), such as propofol [15, 55, 56]. In these cases, a higher body weight-normalized volume of distribution is found in neonates. This is explained by the decrease in volume/kg of blood and extra- and intra-cellular fluids that occurs with increasing age [45, 55].
Interestingly, V3/V1 ≈ 15 and V3/V2 ≈ 7, indicating higher distribution in the deeper compartment. In fact, the transfer rate constant from the deep distribution compartment to the central compartment (k31) is much slower than the transfer rate constant from the central compartment to the deep distribution compartment (k13) (Table 3), reflecting binding to lipid components. A practical consequence of this is that a tricompartimental representation should be used to correctly predict release and equilibrium with such compartments.
When comparing the model development variables with published reports on fentanyl in neonates, several aspects should be taken into consideration. First, the scarcity of public domain sources in relation to the neonatal pharmacokinetics of fentanyl is remarkable. Also, existing methodologic differences between reports may influence the estimates and complicate comparison. Subjective measures of effect (facial expression, motor activity) are still widely used instead of standardized measures such as EEG.
Importantly, the heterogeneity of the neonatal patient population can also significantly affect any reported pharmacokinetics or pharmacodynamics. Sources of heterogeneity include, among others, patients’ gestational and postnatal age, underlying diseases, co-medication, previous exposure to opioids, dosage schedule, sampling times, fentanyl clinical use (coadjutant in anesthesia, analgesic and/or sedative), and the analytical method employed for determination of fentanyl in plasma. One of the ramifications of the heterogeneity in reporting is that, although the present model is applicable to normal term neonates, some of the values in the literature used for parameter comparison refer to population samples that also included preterm newborns since the relevant reports did not provide individual data [20, 40]. Comparing data is also complicated due to lack of consensus when presenting parameters as either whole or body weight corrected estimates. We have presented both formats here (Table 4).
5 Conclusions
Part of the uncertainty in the therapeutic outcome of fentanyl can be reduced by using a model that takes into account the sources of variability linked to the differential maturation of physiologic parameters. Unlike allometric scaling, the advantage of semi-physiologic approaches when predicting drug disposition (ADME) in children is that they integrate the multiple and complex developmental changes that accompany growth (enzymes, proteins, organ weights, blood flows, etc.). Furthermore, as these models are built on a physiologic basis, they can be refined and expanded (with a consequent improvement in their predictive capacity) as new data become available (e.g., a new metabolic pathway, a new carrier, definitive evidence supporting the role of P-glycoprotein, genetic polymorphisms, etc.).
The proposed semi-physiologic approach represents the first step towards the development of a model that describes the ontogeny of all of the processes involved in fentanyl ADME. Although the model specifically addresses the neonatal period and concerns normal term newborns, it could be extended to the entire pediatric population. Furthermore, as the present model is built entirely within a mixed-effects framework, inclusion of subpopulation-related predictors such as co-medication, intervention, and others can be achieved by applying formal statistics.
Particularly because of the model’s limitations, as discussed, and prior to clinical application, the model should be validated in comparison with observed pharmacokinetic and pharmacodynamic responses to fentanyl from clinical practice in neonatology. Our group is currently completing a test of the model in the neonatal piglet with promising results. The model is also being applied in optimization of the sampling protocol for an observational trial in routine care of neonates. The semi-physiologic and pharmacokinetic parameters will be assessed and reported.
References
Aranda JV, Carlo W, Hummel P, Thomas R, Lehr VT, Anand KJS. Analgesia and sedation during mechanical ventilation in neonates. Clin Ther. 2005;27(6):877–99.
Tobias JD. Sedation and analgesia in paediatric intensive care units: a guide to drug selection and use. Paediatr Drugs. 1999;1(2):109–26.
Jacqz-Aigrain E, Burtin P. Clinical pharmacokinetics of sedatives in neonates. Clin Pharmacokinet. 1996;31(6):423–43.
Playfor S, Jenkins I, Boyles C, Choonara I, Davies G, Haywood T, et al. Consensus guidelines on sedation and analgesia in critically ill children. Intensive Care Med. 2006;32(8):1125–36.
Knibbe CAJ, Danhof M. Individualized dosing regimens in children based on population PKPD modelling: are we ready for it? Int J Pharm. 2011;415(1–2):9–14.
Bellanti F, Della Pasqua O. Modelling and simulation as research tools in paediatric drug development. Eur J Clin Pharmacol. 2011;67(Suppl 1):75–86.
Manolis E, Osman TE, Herold R, Koenig F, Tomasi P, Vamvakas S, et al. Role of modeling and simulation in pediatric investigation plans. Paediatr Anaesth. 2011;21(3):214–21.
Tod M, Jullien V, Pons G. Facilitation of drug evaluation in children by population methods and modelling. Clin Pharmacokinet. 2008;47(4):231–43.
Anderson BJ, Holford NHG. Mechanistic basis of using body size and maturation to predict clearance in humans. Drug Metab Pharmacokinet. 2009;24(1):25–36.
Björkman S. Prediction of drug disposition in infants and children by means of physiologically based pharmacokinetic (PBPK) modelling: theophylline and midazolam as model drugs. Br J Clin Pharmacol. 2005;59(6):691–704.
Baber N, Pritchard D. Dose estimation for children. Br J Clin Pharmacol. 2003;56(5):489–93.
Johnson TN, Rostami-Hodjegan A, Tucker GT. Prediction of the clearance of eleven drugs and associated variability in neonates, infants and children. Clin Pharmacokinet. 2006;45(9):931–56.
Rostami-Hodjegan A, Tucker GT. Simulation and prediction of in vivo drug metabolism in human populations from in vitro data. Nat Rev Drug Discov. 2007;6(2):140–8.
Chay PC, Duffy BJ, Walker JS. Pharmacokinetic–pharmacodynamic relationships of morphine in neonates. Clin Pharmacol Ther. 1992;51(3):334–42.
Allegaert K, de Hoon J, Verbesselt R, Naulaers G, Murat I. Maturational pharmacokinetics of single intravenous bolus of propofol. Paediatr Anaesth. 2007;17(11):1028–34.
Hughes MA, Glass PSA, Jacobs JR. Context-sensitive half-time in multicompartment: pharmacokinetic models for intravenous anesthetic drugs. Anesthesiology. 1992;76(3):334–41.
Shafer SL, Varvel JR. Pharmacokinetics, pharmacodynamics, and rational opioid selection. Anesthesiology. 1991;74(1):53–63.
Scott JC, Stanski DR. Decreased fentanyl and alfentanil dose requirements with age. A simultaneous pharmacokinetic and pharmacodynamic evaluation. J Pharmacol Exp Ther. 1987;240(1):159–66.
Verotta D, Beal SL, Sheiner LB. Semiparametric approach to pharmacokinetic–pharmacodynamic data. Am J Physiol. 1989;256(4 Pt 2):R1005–10.
Saarenmaa E, Neuvonen PJ, Fellman V. Gestational age and birth weight effects on plasma clearance of fentanyl in newborn infants. J Pediatr. 2000;136(6):767–70.
Bouillon-Pichault M, Jullien V, Bazzoli C, Pons G, Tod M. Pharmacokinetic design optimization in children and estimation of maturation parameters: example of cytochrome P450 3A4. J Pharmacokinet Pharmacodyn. 2011;38(1):25–40.
Anderson BJ. Pediatric models for adult target-controlled infusion pumps. Paediatr Anaesth. 2010;20(3):223–32.
McNamara PJ, Alcorn J. Protein binding predictions in infants. AAPS PharmSci. 2002;4(1):E4.
Feierman DE, Lasker JM. Metabolism of fentanyl, a synthetic opioid analgesic, by human liver microsomes: role of CYP3A4. Drug Metab Dispos. 1996;24(9):932–9.
Labroo RB, Paine MF, Thummel KE, Kharasch ED. Fentanyl metabolism by human hepatic and intestinal cytochrome P450 3A4: implications for interindividual variability in disposition, efficacy, and drug interactions. Drug Metab Dispos. 1997;25(9):1072–80.
Edginton AN, Schmitt W, Willmann S. Development and evaluation of a generic physiologically based pharmacokinetic model for children. Clin Pharmacokinet. 2006;45(10):1013–34.
Bouzom F, Walther B. Pharmacokinetic predictions in children by using the physiologically based pharmacokinetic modelling. Fundam Clin Pharmacol. 2008;22(6):579–87.
International Commission on Radiological Protection. Basic anatomical and physiological data for use in radiological protection: reference values. ICRP Publication 89. Ann ICRP. 2002;32(3–4):5–265.
Booker PD, Taylor C, Saba G. Perioperative changes in alpha 1-acid glycoprotein concentrations in infants undergoing major surgery. Br J Anaesth. 1996;76(3):365–8.
Blain PG, Mucklow JC, Rawlins MD, Roberts DF, Routledge PA, Shand DA. Determinants of plasma alpha-1-acid glycoprotein (AAG) concentrations in health. Br J Clin Pharmacol. 1985;20(5):500–2.
Alcorn J, McNamara PJ. Ontogeny of hepatic and renal systemic clearance pathways in infants: part II. Clin Pharmacokinet. 2002;41(13):1077–94.
Hayton WL. Maturation and growth of renal function: dosing renally cleared drugs in children. AAPS PharmSci. 2000;2(1):E3.
Alcorn J, McNamara PJ. Ontogeny of hepatic and renal systemic clearance pathways in infants: part I. Clin Pharmacokinet. 2002;41(12):959–98.
Edginton AN, Schmitt W, Voith B, Willmann S. A mechanistic approach for the scaling of clearance in children. Clin Pharmacokinet. 2006;45(7):683–704.
Björkman S. Prediction of cytochrome p450-mediated hepatic drug clearance in neonates, infants and children: how accurate are available scaling methods? Clin Pharmacokinet. 2006;45(1):1–11.
Lötsch J. Pharmacokinetic–pharmacodynamic modeling of opioids. J Pain Symptom Manag. 2005;29(5 Suppl):S90–103.
Scott JC, Ponganis KV, Stanski DR. EEG quantitation of narcotic effect: the comparative pharmacodynamics of fentanyl and alfentanil. Anesthesiology. 1985;62(3):234–41.
Scott JC, Cooke JE, Stanski DR. Electroencephalographic quantitation of opioid effect: comparative pharmacodynamics of fentanyl and sufentanil. Anesthesiology. 1991;74(1):34–42.
Shafer SL. Towards optimal intravenous dosing strategies. Semin Anesth. 1993;12(4):222–34.
Roth B, Schlünder C, Houben F, Günther M, Theisohn M. Analgesia and sedation in neonatal intensive care using fentanyl by continuous infusion. Dev Pharmacol Ther. 1991;17(3–4):121–7.
Yassen A, Olofsen E, Dahan A, Danhof M. Pharmacokinetic–pharmacodynamic modeling of the antinociceptive effect of buprenorphine and fentanyl in rats: role of receptor equilibration kinetics. J Pharmacol Exp Ther. 2005;313(3):1136–49.
Kalvass JC, Olson ER, Cassidy MP, Selley DE, Pollack GM. Pharmacokinetics and pharmacodynamics of seven opioids in P-glycoprotein-competent mice: assessment of unbound brain EC50, u and correlation of in vitro, preclinical, and clinical data. J Pharmacol Exp Ther. 2007;323(1):346–55.
Yassen A, Kan J, Olofsen E, Suidgeest E, Dahan A, Danhof M. Mechanism-based pharmacokinetic–pharmacodynamic modeling of the respiratory-depressant effect of buprenorphine and fentanyl in rats. J Pharmacol Exp Ther. 2006;319(2):682–92.
Gauntlett IS, Fisher DM, Hertzka RE, Kuhis E, Spellman MJ, Rudolph C. Pharmacokinetics of fentanyl in neonatal humans and lambs: effects of age. Anesthesiology. 1988;69(5):683–7.
Johnson KL, Erickson JP, Holley FO, Scott JC. Fentanyl pharmacokinetics in the pediatric population. Anesthesiology. 1984;61(3):A441.
Koehntop DE, Rodman JH, Brundage DM, Hegland MG, Buckley JJ. Pharmacokinetics of fentanyl in neonates. Anesth Analg. 1986;65(3):227–32.
Franck LS, Miaskowski C. The use of intravenous opioids to provide analgesia in critically ill, premature neonates: a research critique. J Pain Symptom Manag. 1998;15(1):41–69.
Singleton MA, Rosen JI, Fisher DM. Plasma concentrations of fentanyl in infants, children and adults. Can J Anaesth. 1987;34(2):152–5.
Anderson BJ, Allegaert K. The pharmacology of anaesthetics in the neonate. Best Pract Res Clin Anaesthesiol. 2010;24(3):419–31.
Koren G, Goresky G, Crean P, Klein J, MacLeod SM. Pediatric fentanyl dosing based on pharmacokinetics during cardiac surgery. Anesth Analg. 1984;63(6):577–82.
Ariano RE, Duke PC, Sitar DS. Population pharmacokinetics of fentanyl in healthy volunteers. J Clin Pharmacol. 2001;41(7):757–63.
Bentley JB, Borel JD, Nenad RE, Gillespie TJ. Age and fentanyl pharmacokinetics. Anesth Analg. 1982;61(12):968–71.
de Wildt SN, Kearns GL, Leeder JS, van den Anker JN. Cytochrome P450 3A ontogeny and drug disposition. Clin Pharmacokinet. 1999;37(6):485–505.
Santeiro ML, Christie J, Stromquist C, Torres BA, Markowsky SJ. Pharmacokinetics of continuous infusion fentanyl in newborns. J Perinatol. 1997;17(2):135–9.
Rigby-Jones AE, Nolan JA, Priston MJ, Wright PM, Sneyd JR, Wolf AR. Pharmacokinetics of propofol infusions in critically ill neonates, infants, and children in an intensive care unit. Anesthesiology. 2002;97(6):1393–400.
Reed MD, Yamashita TS, Marx CM, Myers CM, Blumer JL. A pharmacokinetically based propofol dosing strategy for sedation of the critically ill, mechanically ventilated pediatric patient. Crit Care Med. 1996;24(9):1473–81.
Lötsch J, Walter C, Parnham MJ, Oertel BG, Geisslinger G. Pharmacokinetics of non-intravenous formulations of fentanyl. Clin Pharmacokinet. 2013;52(1):23–36.
Acknowledgments
At the time of preparation of this study, Rosario Calvo was employed at the Department of Pharmacology, School of Medicine, University of the Basque Country, Leioa, Spain. This study was supported by a predoctoral grant to one of the authors (Esther Encinas) from the Research Staff Training Program (Basque Country Government) and by an INNPACTO project of the Spanish Ministry of Science and Innovation—MICINN (ITP-09000-2010-002). One of the investigators (John C. Lukas) was supported by an Ikerbasque Visiting Professor Grant. Esther Encinas, Rosario Calvo, John C. Lukas, Valvanera Vozmediano, Monica Rodriguez, and Elena Suarez have no conflicts of interest that are directly relevant to the content of this study.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Encinas, E., Calvo, R., Lukas, J.C. et al. A Predictive Pharmacokinetic/Pharmacodynamic Model of Fentanyl for Analgesia/Sedation in Neonates Based on a Semi-Physiologic Approach. Pediatr Drugs 15, 247–257 (2013). https://doi.org/10.1007/s40272-013-0029-1
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40272-013-0029-1