Abstract
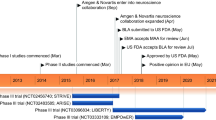
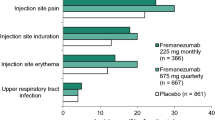
Erenumab (Aimovig®, erenumab-aooe), a fully human monoclonal antibody (MAb) calcitonin gene-related peptide (CGRP) receptor antagonist, is the first MAb approved for the prophylaxis of migraine in adults. Erenumab is subcutaneously administered and has a convenient once-monthly/every-4-week dosing regimen. In patients with episodic or chronic migraine, erenumab is effective and generally well tolerated, significantly reducing the frequency of migraines and the use of migraine-specific medications during weeks 9–12 and months 4–6 relative to placebo. Erenumab also displays efficacy in numerous subgroup analyses, including in patients with episodic or chronic migraine with prior prophylactic treatment failure and/or patients with a history of aura. Although the efficacy and tolerability profiles of erenumab remain to be determined in specific populations (for example, in patients with major cardiovascular disease), it is a promising candidate for alleviating the widespread personal, societal and economic burdens that are presently associated with migraine.

Similar content being viewed by others
References
Headache Classification Committee of the International Headache Society. The International Classification of Headache Disorders, 3rd edition (beta version). Cephalalgia. 2013;33(9):629–808.
NICE (National Institute for Health and Care Excellence). Headaches in over 12s: diagnosis and management (CG150). London: NICE; 2012.
World Health Organization. Fact sheet: headache disorders. Geneva: World Health Organization; 2016.
Evers S, Afra J, Frese A, et al. EFNS guideline on the drug treatment of migraine–revised report of an EFNS task force. Eur J Neurol. 2009;16(9):968–81.
Silberstein SD, Holland S, Freitag F, et al. Evidence-based guideline update: pharmacologic treatment for episodic migraine prevention in adults. Neurology. 2012;78(17):1337–45.
Silberstein SD. Practice parameter: evidence-based guidelines for migraine headache (an evidence-based review). Neurology. 2000;55(6):754–62.
Steiner T, MacGregor E, Davies P. Guidelines for all healthcare professionals in the diagnosis and management of migraine, tension-type, cluster and medication overuse headache, 3rd edition (1st revision). Hull: British Association for the Study of Headache; 2010.
Frampton JE, Silberstein S. OnabotulinumtoxinA: a review in the prevention of chronic migraine. Drugs. 2018;78(5):589–600.
Hepp Z, Bloudek LM, Varon SF. Systematic review of migraine prophylaxis adherence and persistence. J Manag Care Pharm. 2014;20(1):22–33.
Yaldo AZ, Wertz DA, Rupnow MF, et al. Persistence with migraine prophylactic treatment and acute migraine medication utilization in the managed care setting. Clin Ther. 2008;30(12):2452–60.
Holland S, Fanning KM, Serrano D, et al. Rates and reasons for discontinuation of triptans and opioids in episodic migraine: results from the American Migraine Prevalence and Prevention (AMPP) study. J Neurol Sci. 2013;326(1–2):10–7.
Woolley JM, Bonafede MM, Maiese BA, et al. Migraine prophylaxis and acute treatment patterns among commercially insured patients in the United States. Headache. 2017;57(9):1399–408.
Stovner L, Hagen K, Jensen R, et al. The global burden of headache: a documentation of headache prevalence and disability worldwide. Cephalalgia. 2007;27(3):193–210.
Vos T, Abajobir AA, Abate KH, et al. Global, regional, and national incidence, prevalence, and years lived with disability for 328 diseases and injuries for 195 countries, 1990–2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet. 2017;390(10100):1211–59.
Bigal ME, Walter S. Monoclonal antibodies for migraine: preventing calcitonin gene-related peptide activity. CNS Drugs. 2014;28(5):389–99.
Benarroch EE. CGRP sensory neuropeptide with multiple neurologic implications. Neurology. 2011;77(3):281–7.
Buture A, Gooriah R, Nimeri R, et al. Current understanding on pain mechanism in migraine and cluster headache. Anesth Pain Med. 2016;6(3):1–8.
Goadsby PJ, Holland PR, Martins-Oliveira M, et al. Pathophysiology of migraine: a disorder of sensory processing. Physiol Rev. 2017;97(2):553–622.
Goadsby PJ, Edvinsson L, Ekman R. Vasoactive peptide release in the extracerebral circulation of humans during migraine headache. Ann Neurol. 1990;28(2):183–7.
Lassen L, Haderslev P, Jacobsen V, et al. CGRP may play a causative role in migraine. Cephalalgia. 2002;22(1):54–61.
Hansen JM, Hauge AW, Olesen J, et al. Calcitonin gene-related peptide triggers migraine-like attacks in patients with migraine with aura. Cephalalgia. 2010;30(10):1179–86.
Russo AF. Calcitonin gene-related peptide (CGRP): a new target for migraine. Annu Rev Pharmacol Toxicol. 2015;55:533–52.
Aimovig (erenumab): EU summary of product characteristics. Dublin: Novartis Europharm Limited; 2018. https://www.ema.europa.eu/documents/product-information/aimovig-epar-product-information_en.pdf. Accessed 11 Oct 2018.
Aimovig™ (erenumab-aoee) injection, for subcutaneous use: US prescribing information. Thousand Oaks: Amgen Inc.; 2018. https://www.accessdata.fda.gov/drugsatfda_docs/label/2018/761077s000lbl.pdf. Accessed 11 Oct 2018.
Giamberardino MA, Affaitati G, Costantini R, et al. Calcitonin gene-related peptide receptor as a novel target for the management of people with episodic migraine: current evidence and safety profile of erenumab. J Pain Res. 2017;10:2751–60.
Xu Y, Gabriel K, Wang Y, et al. A multicenter, open-label, pharmacokinetic drug interaction study of erenumab (AMG 334) and a combined oral contraceptive in healthy female subjects [abstract no. PS23]. Headache. 2017;57(Suppl 3):192–3.
de Hoon J, Van Hecken A, Vandermeulen C, et al. Phase 1, randomized, parallel-group, double-blind, placebo-controlled trial to evaluate the effects of erenumab (AMG 334) and concomitant sumatriptan on blood pressure in healthy volunteers. Cephalalgia. 2018. https://doi.org/10.1177/0333102418776017.
de Hoon J, Van Hecken A, Vandermeulen C, et al. Phase I, randomized, double-blind, placebo-controlled, single-dose, and multiple-dose studies of erenumab in healthy subjects and patients with migraine. Clin Pharmacol Ther. 2018;103(5):815–25.
Shi L, Lehto SG, Zhu DX, et al. Pharmacologic characterization of AMG 334, a potent and selective human monoclonal antibody against the calcitonin gene-related peptide receptor. J Pharmacol Exp Ther. 2016;356(1):223–31.
Sun H, Dodick DW, Silberstein S, et al. Safety and efficacy of AMG 334 for prevention of episodic migraine: a randomised, double-blind, placebo-controlled, phase 2 trial. Lancet Neurol. 2016;15(4):382–90.
Dodick DW, Ashina M, Brandes JL, et al. ARISE: a phase 3 randomized trial of erenumab for episodic migraine. Cephalalgia. 2018;38(6):1026–37.
Goadsby PJ, Reuter U, Hallstrom Y, et al. A controlled trial of erenumab for episodic migraine. N Engl J Med. 2017;377(22):2123–32.
Reuter U, Goadsby PJ, Lanteri-Minet M, et al. Efficacy and tolerability of erenumab in patients with episodic migraine in whom two-to-four previous preventive treatments were unsuccessful: a randomised, double-blind, placebo-controlled, phase 3b study. Lancet. 2018. https://doi.org/10.1016/s0140-6736(18)32534-0.
Tepper S, Ashina M, Reuter U, et al. Safety and efficacy of erenumab for preventive treatment of chronic migraine: a randomised, double-blind, placebo-controlled phase 2 trial. Lancet Neurol. 2017;16(6):425–34.
Edvinsson L. The trigeminovascular pathway: role of CGRP and CGRP receptors in migraine. Headache. 2017;57(Suppl 2):47–55.
Silberstein S, Lenz R, Xu C. Therapeutic monoclonal antibodies: what headache specialists need to know. Headache. 2015;55(8):1171–82.
Ashina M, Dodick D, Goadsby PJ, et al. Erenumab (AMG 334) in episodic migraine: interim analysis of an ongoing open-label study. Neurology. 2017;89(12):1237–43.
Paemeleire K, Broessner G, Brandes J, et al. Efficacy of erenumab in subjects with episodic migraine with prior preventive treatment failure(s) [abstract no. O1]. J Headache Pain. 2017;18(Suppl 1):135–6.
Pascual J, Buse DC, Starling AJ, et al. Effect of erenumab on patient-reported outcomes in episodic migraine patients with prior prophylactic treatment failure: results from a post-hoc analysis of the STRIVE study [abstract no. PS49]. Headache. 2018;58(Suppl 2):179–80.
McAllister P, Gomez JP, McGill L, et al. Efficacy of erenumab for the treatment of patients with episodic migraine with aura [abstract no. P4.094]. Neurology. 2018;90(15 Suppl).
Tepper S, Broessner G, Buse D, et al. Efficacy of erenumab for the treatment of patients with episodic migraine with depression and/or anxiety [abstract no. P4.105]. Neurology. 2018;90(15 Suppl).
Pavlovic J, Paemeleire K, Gobel H, et al. Efficacy of erenumab in women with and without a history of menstrually-related migraine [abstract no. P4.096]. Neurology. 2018;90(15 Suppl).
Ashina M, Tepper S, Brandes JL, et al. Efficacy and safety of erenumab (AMG334) in chronic migraine patients with prior preventive treatment failure: a subgroup analysis of a randomized, double-blind, placebo-controlled study. Cephalalgia. 2018;38(10):1611–21.
Lanteri-Minet M, Buse DC, Starling AJ, et al. Patient-reported outcomes in chronic migraine patients with prior prophylactic treatment failure receiving placebo or erenumab: subgroup analysis of a pivotal randomized study [abstract no. PS36]. Headache. 2018;58(Suppl 2):170–1.
Diener HC, Ashina M, Brandes J, et al. Efficacy of erenumab for the treatment of patients with chronic migraine in presence of medication overuse [abstract no. PR1048]. Eur J Neurol. 2017;(Suppl 1):472.
Ashina M, Dodick D, Goadsby P, et al. Efficacy of erenumab for the treatment of patients with chronic migraine with and without aura [abstract no. S32.006]. Neurology. 2018;90(15 Suppl).
Assessment report: Aimovig. London: European Medicines Agency; 2018.
Winner P, Reuter U, Dodick D, et al. Erenumab safety among migraine patients using triptans or with cardiovascular (CV) risk factors [abstract no. P4.100]. Neurology. 2018;90(15 Suppl).
Tepper S, Pascual J, Reuter U, et al. Analysis of blood pressure following short-term and long-term treatment with erenumab [abstract no. P4.103]. Neurology. 2018;90(15 Suppl).
Vargas B, Starling A, Silberstein S, et al. Erenumab immunogenicity: a pooled analysis of phase 2 and phase 3 migraine prevention clinical trials [abstract no. P4.098]. Neurology. 2018;90(15 Suppl).
Acknowledgements
The manuscript was reviewed by: H.-C. Diener, Faculty of Medicine, University Duisburg-Essen, Essen, Germany; J. de Hoon, Center for Clinical Pharmacology, University Hospitals of Leuven, Leuven, Belgium. During the peer review process, Amgen Inc. and Novartis Pharmaceutical Corporation, the marketing-authorization holders of erenumab (Aimovig®), were also offered an opportunity to provide a scientific accuracy review of their data. Changes resulting from comments received were made on the basis of scientific and editorial merit.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
The preparation of this review was not supported by any external funding.
Conflicts of interest
E.H. McCafferty and K.A. Lyseng-Williamson are employees of Adis, are responsible for the article content and declare no conflicts of interest.
Rights and permissions
About this article
Cite this article
McCafferty, E.H., Lyseng-Williamson, K.A. Erenumab in the prophylaxis of migraine: a profile of its use. Drugs Ther Perspect 35, 13–20 (2019). https://doi.org/10.1007/s40267-018-0589-9
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40267-018-0589-9