Abstract
Vitiligo is a chronic inflammatory skin disease leading to the loss of epidermal melanocytes. To date, treatment options for vitiligo patients are limited, lack sustained efficacy, and are mainly based on off-label use of immunosuppressive agents, such as systemic or topical steroids or topical calcineurin inhibitors, in association with the use of ultraviolet light. However, recent insights into the understanding of the immune pathogenesis of the disease have led to the identification of several therapeutic targets and the development of targeted therapies that are now being tested in clinical trials. In this review, based on the physiopathology of the disease, we summarize emerging targets that could be developed for the treatment of vitiligo and discuss recent and ongoing developments of drugs for the management of the disease.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
A better understanding of the immune pathogenesis of vitiligo has led to the identification and development of targeted therapies. |
Targeting innate immune pathways through the inhibition of danger signals, such as HSP70, represents an interesting approach for the treatment of vitiligo. |
Resident memory T cells are involved in the recurrence of vitiligo and could be targeted by blocking interleukin-15. |
Trials involving JAK inhibitors, which inhibit the effects of several pro-inflammatory cytokines, have shown promising results in vitiligo. |
Promoting the regeneration of melanocytes and preventing their loss will still be an important step to consider in treating vitiligo. |
Digital Features
This article is published with digital features to facilitate understanding of the article. To view digital features for this article go to https://doi.org/10.6084/m9.figshare.12928409.
Introduction
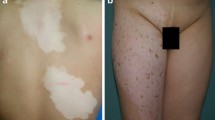
Vitiligo is a common chronic inflammatory skin depigmenting disorder with a worldwide prevalence of 0.5–1% [1]. The occurrence of white patches results from a loss of epidermal melanocytes [2]. While vitiligo does not affect life expectancy, the color dissimilarity has a serious impact on patients’ quality of life and mental well-being, with patients often enduring stigmatization and social isolation, as well as being more subject to psychiatric morbidities [3, 4]. To date, available treatments for vitiligo remain limited, and therapeutical strategies rely on nonspecific therapies targeting the inflammatory and immune responses, such as topical or systemic steroids or topical calcineurin inhibitors, both associated with ultraviolet (UV) light to promote melanocyte regeneration. This limitation in treatment possibilities highlights the need to improve vitiligo management.
The physiopathology of vitiligo is complex and involves multiple combinatorial factors. One of the leading hypothesis is that the immune response plays a role in targeting the melanocyte compartment, as evidenced by genome-wide association studies (GWAS) that demonstrated the association of vitiligo with genes mainly related to both innate and adaptive immune responses [5]. Both animal models and human studies have also highlighted the important role of the immune system in vitiligo, opening new doors of hope for the development of targeted therapies dedicated to this disease [2]. These therapies will target inflammatory responses of immune and epidermal cells occuring during the progression or relapse of the disease. Therefore, early aggressive treatments can now be considered that would inhibit the consequences of the immune response against melanocytes to prevent their loss. Once the exaggerated immune response is controlled, the regeneration of melanocytes from hair follicles or interfollicular compartment is an important to consideration, as is a maintenance therapy to prevent the recurrence of the disease (Fig. 1).
Emerging treatments in vitiligo. Development of vitiligo is associated with skin inflammation. Strategies targeting the innate and adaptive immune response will be important to control skin inflammation in vitiligo, to stabilize and prevent the progression of the disease. Therapies aiming to promote melanocyte regeneration will also be important to consider to induce regimentation. Lastly, a maintenance therapy will be of utmost importance to prevent the recurrence of the disease.
In this review, we discuss the current concepts for managing vitiligo and summarize future innovative strategies and ongoing clinical trials (Table 1).
This article is based on previously conducted studies and does not contain any studies with human participants or animals performed by any of the authors.
Blocking the Initiation and Restraining the Progression of the Disease
Targeting Innate Immunity
Danger Signals from Epidemal Cells
Epidermal cells in vitiligo, especially melanocytes, exhibit metabolic defects that contributed to increased levels of reactive oxygen species (ROS) [6]. These changes, in the context of a susceptible genetic background, are associated with the release of pro-inflammatory cytokines and damage-associated molecular patterns (DAMPs, or endogenous danger molecules). Inducible heat shock protein 70 (HSP70i), calreticulin (CRT), and high-mobility group protein B1 (HMGB1) are the most studied molecules in vitiligo [2]. The secretion of DAMPs in the extracellular environment may be accountable for bridging cellular stress to the autoimmune response against melanocytes in vitiligo [7] and, therefore, could represent highly interesting potential targets to prevent initiation of autoimmunity at the onset of the disease. Indeed, HMGB1 can induce the production of chemokine ligands, such as (C-X-C motif) ligand (CXCL1)6 or interleukin (IL)-8 by keratinocytes, which is important for the recruitment of immune cells [8]. For its part, CRT has been reported to induce melanocyte apoptosis and the release of membrane-debris important for immunogenecity [9]. To date, HSP70i seems to be a critical component in the initiation of the disease. HSP70i is overexpressed in vitiliginous skin compared to healthy control skin and plays an important role in the induction and progression of vitiligo in mice [10,11,12,13]. Blocking HSP70i activity might offer a good strategy to treat vitiligo. Le Poole and colleagues were the first to show that a plasmid DNA encoding a mutant HSP70i with a single amino acid change (HSP70iQ435A) was capable of preventing and reversing vitiligo in mouse models by dampening the activation of dendritic cells (DC) [12]. The same research team then confirmed their initial results in the Sinclair swine model that develops melanomas regressing by immune surveillance, leading to vitiligo-like depigmentation. The findings of this subsequent study showed that treating swine with HSP70iQ435A-encoding DNA induced repigmentation of treated lesions and, most importantly, of distant vitiligo lesions, indicating a possible systemic effect [14]. This approach seems to confer a long-lasting repigmentation. Moreover, transfection of HSP70iQ435A DNA in human vitiligo skin explants could reoriente the immune phenotype toward an anti-inflammatory phenotype [12], reinforcing the potential of HSP70iQ435A as an interesting therapeutic option in vitiligo. Clinical studies will be necessary to confirm these encouraging preclinical data.
Another approach could be the direct neutralization of DAMPs by blocking agents. As an example, three anti-HGMB1 monoclonal antibodies have been developed that show beneficial therapeutic effects in experimental models of different inflammatory conditions, such as sepsis or arthritis; however, these have not yet been tested in clinical trials [15, 16].
These different approaches targeting DAMPs secreted by stressed melanocytes and/or keratinocytes at an early stage of the disease could prevent activation of the innate immune system by blocking their interaction with pathogen recognition receptors and, consequently, activation of local DC, in particular plasmacytoid DC (pDC), leading to the production of type I interferon (IFN) [17].
The Type I IFN Pathway
Several data link vitiligo to a type I IFN signature. First, variants of INF induced with the helicase C domain 1 (IFIH1) gene, associated with a loss of function, could provide protection against vitiligo [18]. IFIH1 encodes melanoma differentiation-associated protein 5 (MDA5), a member of the RIG-I-like receptor family and a sensor of dsRNA; IFIH1 induces the production of IFN-α [19]. Interestingly, a recent study showed that MDA5 could potentiate epidermal secretion of the chemokines CXCL10 and CXCL16, important recruiters of autoreactive T cells [19]. pDC are the major cell subset responsible for the production of IFN-α. Our group previously reported the presence of IFN-α in vitiliginous skin during the initiation and spreading of the disease, associated with increased expression of type I IFN-related molecules [20]. In vitiliginous skin, these cells could be activated by local production of HSP70i by epidermal cells, potentiating their production of IFN-α [17].
IFN-α is an important actor in the initiation of the disease by inducing the production of chemokines ligands, such as CXCL9 and CXCL10, by epidermal cells [17]. Hydroxychloroquine (HCL) acts on the immune system notably by inhibiting endosomal Toll-like receptors (TLRs), in particular TLR7 and TLR9, which results in impairment of IFN-α production by pDC. Moreover, this anti-malaria drug is known to induce hyperpigmentation; a case report described repigmentation of vitiligo lesions in a patient treated for rheumatoid arthritis with HCL [21, 22]. Taking these data into consideration, this treatment could be subjected to a clinical trial. Another interesting and more specific approach could be anti-blood DC antigen 2 (BDCA2) therapy. BDCA2 is an inhibitory receptor expressed on pDC which, once engaged, inhibits the production of type I IFN [23]. A proof of concept study showed that a monoclonal antibody directed against BDCA2 (BIIB059) improved the cutaneous lesions of systemic lupus erythematosus (SLE), and a phase II clinical trial is ongoing in cutaneous lupus erythematosous [24] (NCT02847598). Another strategy to block the IFN-α pathway would involve the use of antibodies directed against the cytokine itself or its receptor, interferon alpha and beta receptor (IFNAR). The use of sifalimumab and anifrolimumab, targeting IFN-α and its receptor, respectively, has proven to be effective for the treatment of SLE [25, 26]. These strategies could therefore be a reliable option to inhibit the initiation of the disease.
Inflammasome
Large-scale genome-wide studies have also bolstered the notion that inflammasome and IL1-β are involved in the development of vitiligo. Polymorphisms in IL-1β and NOD-like receptor protein 1 (NLRP1) inflammasome are associated with an increased risk to develop vitiligo [5, 27]. Moreover, IL-1β and NLRP1 are overexpressed in perilesional skin of patients with vitiligo [28]. The NLRP1 inflammasome is activated by sensing DAMPs released by stressed melanocytes, leading to caspase 1 activation and the subsequent release of IL-1β. This pro-inflammatory cytokine promotes the immune response by activating T lymphocytes and promoting the migration of immune cells [29]. Treatments directed against the NLRP1 inflammasome or IL-1β, which have not yet been tested in vitiligo, may be other treatments that to act on the first step of the pathogenesis of this disease.
Targeting the Adaptative Immune Response
Resident Memory T Cells
The recurrence of vitiligo on previously affected anatomic sites demonstrate the role of a memory response in vitiligo [30]. Indeed, resident memory T (TRM) cells have been identified in vitiligo [31]. TRM display a memory phenotype, have a distinct transcriptional program, and express characteristic cell-surface markers, such as CD69, CD103, or the newly identified CD49a; as such, they define a subset of TRM cells with cytotoxic properties [32,33,34]. It is now evident that the microenvironment plays a crucial role during TRM formation and regulation. It is known that the expression of CD103 depends on transforming growth factor-β (TGF-β), and an increasing number of studies are reporting the involvement of several cytokines involved in T-cell homeostasis (IL-15) or inflammation (IL-12, IL-18, IL-33, IFN-β, tumor necrosis factor [TNF]-α) during the differentiation or regulation of TRM [35]. Therefore, owing to their functional role in the pathogenesis of vitiligo, targeting this T-cell subset offers a reliable approach to managing vitiligo. Strategies targeting IL-15 or its receptor are promising in terms of inhibiting the generation of TRM, as recently shown in a pre-clinical mouse model of vitiligo with the use of an antibody directed against CD122, the β subunit of the IL-15 receptor, which is expressed on TRM cells [31]. However, human data are still lacking to confirm these results. Lastly, it was recently demonstrated that TRM survival is dependent on the uptake and metabolism of exogenous fatty acids, suggesting that a possible treatment for inflammatory disorders could be modulation of the lipid metabolic program, possibly leading to TRM elimination from peripheral tissues [36, 37].
T Helper Type 1-Skewed Immune Profile in Vitiligo
Vitiliginous skin is consistently associated with the infiltration of immune cells confined to the vicinity of the remaining melanocytes, characterized by the presence of CD8 T cells with a type 1-skewed immune profile and producing elevated levels of IFN-γ and TNF-α. These T cells are characterized by the expression of the chemokine receptor CXCR3 and can respond to CXCR3 cognate ligands CXCL9 and CXCL10, which are highly expressed in vitiliginous skin [38, 39]. Therefore, targeting the CXCR3–CXCL9 and CXCL10 axis in vitiligo appears to be a promising therapeutic strategy. Pre-clinical models in mice have shown significant repigmentation in response to CXCL10 blocking [40], but these data are not yet confirmed in human studies. A monoclonal antibody directed against CXCL10 has been developed and tested in inflammatory bowel diseases, but the absence of significant results observed in Phase II trials did not encourage further development in chronic inflammatory disorders. Statins have been shown to reduce the production of chemokines ligands, such as CXCL10, and have been tested in two randomized clinical trials in combination with UV light [41, 42]; however, no significant repigmentation was observed in the group treated with statins compared to the placebo control group. Targeting the CXCL10 receptor could represent another strategy, as also proposed in pre-clinical models [43]. Several classes of CXCR3 small molecule inhibitors have been developed to date; the one developed by Amgen Inc. (AMG-487) did not show clinical efficacy in psoriasis disease and was not further developed. Recently, NKG2D, an activating receptor, was found to define a highly functional memory CD8 T-cell subset in vitiliginous skin and could therefore represent a potential therapeutic target. A monoclonal antibody directed against NKG2D showed promising results in Crohn’s disease, supporting further development in this disease, but also in other chronic inflammatory disease where NKG2D-expressing cells are involved [44, 45].
In addition to indications that T helper type 1/cytotoxic T lymphocyte (Th1/Tc1) subsets are involved in vitiligo, data suggest that more heterogeneous lymphocyte subsets are also implicated in the pathogenesis of this disease [46, 47]. Future studies are required to dissect the role of the different immune T-cell subsets in vitiligo before investigating therapeutic options that target them.
Cytokines and their Signaling Pathways
Cytokines are key mediators of melanocyte loss in vitiligo and participate at every step of the pathogenesis of this disease. The IFN-γ and TNF-α immune pathways are the most extensively studied to date in vitiligo and appear to be critical for disease initiation and progression.
The binding of IFN-γ to its receptor induces the Janus kinase/signal transducer and activator of the transcription (JAK/STAT) pathway, in particular JAK1-2 and STAT1 activation [48]. In contrast, binding of TNF-α to its receptors (TNF receptor superfamily: TNFR1 or TNFR2) mainly induces the activation of the mitogen-activated protein kinases (MAPK) and nuclear factor-kappa B (NF-kB) pathways [49]. Recent studies in vitiligo have demonstrated that IFN-γ induces the production of the CXCR3 ligands CXCL9 and CXCL10 by keratinocytes, thereby amplifying inflammation and the recruitment of immune cells expressing CXCR3 that will further promote vitiligo progression [50, 51]. IFN-γ and TNF-α also have a direct impact on melanocyte function by decreasing the pigmentation process. Treatment with physiological levels of IFN-γ has been shown to downregulate the expression of melanogenic genes and stall the maturation of melanosome at stages I and II [52]. The canonical JAK/STAT1 pathway along with the downstream transcriptional regulator interferon regulatory factor-1 (IRF-1) is the primary mediator that suppresses pigmentation in melanocytes [53]. Additionally, we have recently shown that the combined activity of IFN-γ and TNF-α can induce the disruption of E-cadherin, the major protein responsible for the adhesion of melanocytes to the basal layer of the epidermis, leading to their destabilization and detachment [54]. In addition to the impact of the IFN-γ signaling pathway on the pathogenesis of vitiligo, other cytokines and their related-signaling pathways have been suggested to play a role in vitiligo. For example, elevated levels of IL-17 and IL-23 have been shown in the sera and/or skin of vitiligo patients. IL-17 could impact the function and survival of melanocytes [55]. Therefore, different strategies targeting cytokines and their signaling pathways could be proposed. Apremilast, a selective phosphodiesterase-4 inhibitor that is currently approved for the treatment of psoriasis and psoriatic arthritis, inhibits the degradation of cAMP, thereby reducing the production of proinflammatory cytokines [56, 57]. In addition to its well-known effects on the modulation of the inflammatory response, apremilast, by increasing the levels of cAMP, could also impact melanocyte growth and differentiation [58]. One case report showed repigmentation of vitiligo lesions after 13 months of apremilast use [59]. However, a recent clinical trial evaluating the efficacy and safety of apremilast in combination with UVB light did not meet the primary endpoint [60].
Despite the role of TNF-α in vitiligo and the fact that anti-TNF-α therapies are commonly used to treat a number of chronic inflammatory disorders, blocking TNF-α in vitiligo has shown conflicting results. It may be that blocking TNF-α in vitiligo could be effective at best in halting disease progression without achieving significant repigmentation [61, 62]. However, the development or worsening of vitiligo has also been reported in patients receiving anti-TNF-α agents [63, 64], and an increased risk of vitiligo following anti-TNF-α therapy has recently been demonstrated in patients treated for other chronic inflammatory conditions [65], probably due to the increased type I IFN signature in lesional skin. These results support the notion that anti-TNF-α can no longer be a treatment option for patients with vitiligo.
Based on data supporting increased levels of Th17-related cytokines, such as IL-17 and IL-23, in the blood and skin of vitiligo patients, targeting the IL-23/IL-17 immune axis might represent another option for patients with vitiligo [55, 66]. However, a recent clinical trial evaluating the efficacy and safety of secukinumab, a monoclonal antibody directed against IL-17, was prematuraly stopped due to the absence of clinical improvement, with worsening of the disease observed in some patients [67].
A number of human monoclonal antibodies against IFN-γ have been tested in clinical trials in patients with psoriasis, Crohn’s disease, and SLE. However, because trials did not reach the primary endpoint, the development of these targeted therapies was not continued.
Better knowledge of the events occurring when cytokines bind to their specific receptors has raised interest in the possibility to target these intracellular signaling cascades. The JAK/STAT pathway mediates signaling between surface receptors and cellular responses. Members of the JAK family include JAK1, JAK2, JAK3, and tyrosine kinase 2 (TYK2), all of which have been shown to be critical components of cytokine-mediated effects, notably those involved in vitiligo pathogenesis, including cytokines associated with innate responses (e.g., IFN-α: JAK1/TYK2) as well as adaptive responses (e.g., IFN-γ: JAK1/JAK2; or IL-2 and IL-15: JAK1/JAK3).
An increasing number of case reports emphasizes that topical or systemic use of the JAK inhibitors tofacitinib (a JAK1/3 inhibitor) [68,69,70,71,72] or ruxolitinib (a JAK1/ 2 inhibitor) [73,74,75] might be effective in inducing repigmentation in vitiligo. Nonetheless, a retrospective study that included ten patients treated with oral tofacitinib indicated that repigmentation using tofacitinib may require association with low-level light therapy, suggesting that anti-JAK therapies are important to dampen skin inflammation, while phototherapy remains the gold standard therapy to activate and stimulate melanocyte replenishment and subsequent repigmentation. More recently, a proof-of-concept clinical trial showed that topical application of ruxolitinib provided significant improvement in facial vitiligo in a small cohort of patients [74]. Additionally, the results of a 32-week open label extension study with optional UV light therapy concomitant with topical ruxolitinib treatment confirmed the benefit of phototherapy to improve repigmentation in patients treated with JAK inhibitors [73]. A randomized, double blind, dose ranging study of topical application of ruxolitinib in vitiligo has been recently published [76]. The primary endpoint was the proportion of patients achieving a ≥ 50% improvement from baseline on the Facial-Vitiligo Area Scoring Index (F-VASI50) at week 24. F-VASI50 at week 24 was reached by significantly more patients that received ruxolitinib cream 1.5% twice daily than patients treated with vehicle [76].
Although JAK antagonism is promising, these treatments cannot dissect the complex and heterogeneous immune signature of vitiligo. Therefore, despite current improvement in the understanding of the immune pathogenesis of vitiligo, finding the right target(s) remains difficult to date. JAK inhibitors are showing promising results, but their broader effects can not reveal which predominant pathways are fully involved in the disease, supporting the notion that an intricate combination of multiple immune pathways are involved in the initiation and progression of the disease.
Immune Tolerance
As a chronic inflammatory disorder, vitiligo is associated with disruption of immune regulation systems. In this line, GWAS identified a polymorphism of forkhead box protein 3 (FOXP3), the master transcription factor of regulatory T cells (Tregs), in vitiliginous skin [77]. However, it is still not clear whether the defect is due to a decreased migration of Tregs into the skin and/or a loss of function [78]. One study reported that an increased skin expression of CCL22 induced the migration of Tregs into the skin, leading to repigmentation in mouse models of depigmentation, suggesting that CCL22 could be a strategy for vitiligo [79]. Another approach to enhance Treg homeostasis and function would be the use of low-dose IL-2 therapy. IL-2 is a key survival factor for Tregs. Administration of low-dose IL-2 has now been widely tested in various chronic autoimmune diseases, such as SLE and, recently, alopecia areata [80, 81]. The interesting effect of low-dose IL-2 therapy is the selective activation of Tregs due to their expression of the high-affinity receptor to IL-2, with minimal effect on effector T cells [80].
Promoting the Regeneration of Melanocytes
Once melanocyte loss has occurred in lesional skin of vitiligo patients, repigmentation through differentiation, proliferation, and migration of new melanocytes in the depigmented area is required. This important step needs to be achieved in combination with immunomodulating agents that will inhibit the immune response. To date, UV light therapy remains the most popular treatment in vitiligo for repopulation of the epidermis with melanocytes from stem cells of the hair follicle. Therefore, vitiligo appears to be a disease model for regenerative medicine.
Intrinsic Abnormalities of Melanocytes
Several in vitro and in vivo studies have demonstrated the presence of intrinsic abnormalities in vitiligo melanocytes. Vitiligo melanocytes are characterized by an altered redox status, with the presence of oxidative stress coupled to an increased susceptibility to pro-oxidant agents [7]. Elevated levels of ROS have been observed in perilesional and non-lesional skin of persons with vitiligo, together with decreased levels of anti-oxidant enzymes, such as catalase, which is important for the protection of cells from oxidative stress [6, 82]. Based on these findings, one proposal has been to treat vitiligo patients with anti-oxidants in order to limit these effects and promote the differentiation and proliferation of melanocytes. However, a recent meta-analysis evaluating the use of anti-oxidant therapies concluded that this strategy is not effective in vitiligo [83]. Another approach consists of the use of platelet-rich plasma.
Stimulating Melanocyte Stem Cells
The differentiation and proliferation of melanocyte stem cells is induced by several soluble factors targeting the melanocortin 1 receptor (MC1R), endothelin receptor, and/or Wnt receptors. The use of platelet-rich plasma that contains several growth factors has received attention as a treatment for stable vitiligo [84]. More precisely, alpha-melanocyte stimulating hormone (α-MSH), through its binding to MC1R, affects several melanocyte functions. This peptide plays a role in the regulation of melanogenesis, dendrite formation, and proliferation and differentiation, and it can also protect melanocytes from oxidative damage [85,86,87]. Clinicals trials have shown the beneficial effect of the combination of afamelatonide, a synthetic analogue of α-MSH, and phototherapy [88, 89], with a higher rate and faster repigmentation observed in the group receiving combination therapy of narrow-band UVB (NB-UVB) + afamelatonide compared to the group receiving NB-UVB as monotherapy. However, afamelatonide caused some side effects, such as hyperpigmentation, headaches, and nausea, that led patients to drop out the study [88]. Regazzetti et al. reported the impairment of Wnt signalling in depigmented skin of vitiligo patients [90]. The WNT pathway is involved in melanoblast differentiation. Ex vivo treatment of vitiligo skin explants with Wnt agonists or GSK3β (glycogen synthase kinase 3β) inhibitors, the critical negative regulator of β-catenin, induced the differentiation of melanoblasts. Hence, the use of pharmacological agents that would activate Wnt signalling could be an interesting approach for the treatment of vitiligo [90].
Maintenance Therapy to Prevent Recurrence of the Disease
As previously discussed, vitiligo is a chronic inflammatory skin disease that needs a careful follow-up for optimal maintenance therapy. Recurrence of the disease is mediated by autoreactive TRM cells located close to replenished melanocytes. To date, a prospective randomized study showed that a twice-weekly application of topical calcineurin inhibitors is an effective treatment strategy to prevent vitiligo relapses by supporting the need to continuously inhibit the immune system to maintain repigmentation [91]. Therefore, with the development of targeted therapies, the use of topical JAK inhibitors could be a reliable treatment in this context. As TRM maintenance in the skin is dependent on IL-15, targeting IL-15 could be another potential treatment strategy. We have recently shown that matrix metalloproteinase (MMP)-9 released by keratinocytes in vitiligo lesional skin could induce the cleavage of E-cadherin, leading to the detachment of epidermal melanocytes. Consequently, MMP-9 inhibition could also be an interesting strategy for stabilizing melanocytes in the basal layer of the epidermis and prevent their loss [54].
Conclusion
Recent research advances in our understanding of the pathogenesis of vitiligo has led to the development of targeted therapies for this disease, which has a high impact on patients’ quality of life. JAK inhibition is showing promising results, and ongoing clinical trials could lead to a first approved treatment for vitiligo. However, research needs also to remain focused on the development of strategies to prevent the loss of melanocytes and/or promote their regeneration, especially for localization of vitiligo that will not respond to the treatment.
References
Elbuluk N, Ezzedine K. Quality of life, burden of disease, co-morbidities, and systemic effects in vitiligo patients. Dermatol Clin. 2017;35:117–28.
Boniface K, Seneschal J, Picardo M, Taïeb A. Vitiligo: focus on clinical aspects, immunopathogenesis, and therapy. Clin Rev Allergy Immunol. 2018;54:52–67.
Hamidizadeh N, Ranjbar S, Ghanizadeh A, Parvizi MM, Jafari P, Handjani F. Evaluating prevalence of depression, anxiety and hopelessness in patients with vitiligo on an Iranian population. Health Qual Life Outcomes. 2020;18:20. https://doi.org/10.1186/s12955-020-1278-7.
Lai YC, Yew YW, Kennedy C, Schwartz RA. Vitiligo and depression: a systematic review and meta-analysis of observational studies. Br J Dermatol. 2017;177:708–18.
Spritz RA, Andersen GHL. Genetics of vitiligo. Dermatol Clin. 2017;35:245–55.
Schallreuter KU, Moore J, Wood JM, et al. In vivo and in vitro evidence for hydrogen peroxide (H2O2) accumulation in the epidermis of patients with vitiligo and its successful removal by a UVB-activated pseudocatalase. J Investig Dermatol Symp Proc. 1999;4:91–6.
Wang Y, Li S, Li C. Perspectives of new advances in the pathogenesis of vitiligo: from oxidative stress to autoimmunity. Med Sci Monit. 2019;25:1017–23.
Cui T, Zhang W, Li S, et al. Oxidative stress-induced HMGB1 release from melanocytes: a paracrine mechanism underlying the cutaneous inflammation in vitiligo. J Invest Dermatol. 2019;139:2174–84.e.
Zhang Y, Liu L, ** L, et al. Oxidative stress-induced calreticulin expression and translocation: new insights into the destruction of melanocytes. J Investig Dermatol. 2014;134:183–91.
Abdou AG, Maraee AH, Reyad W. Immunohistochemical expression of heat shock protein 70 in vitiligo. Ann Diagn Pathol. 2013;17:245–9.
Denman CJ, McCracken J, Hariharan V, et al. HSP70i accelerates depigmentation in a mouse model of autoimmune vitiligo. J Invest Dermatol. 2008;128:2041–8.
Mosenson JA, Zloza A, Nieland JD, et al. Mutant HSP70 reverses autoimmune depigmentation in vitiligo. Sci Transl Med. 2013;5:174ra28. https://doi.org/10.1126/scitranslmed.3005127.
Mosenson JA, Zloza A, Klarquist J, Barfuss AJ, Guevara-Patino JA, Le Poole IC. HSP70i is a critical component of the immune response leading to vitiligo. Pigment Cell Melanoma Res. 2012;25:88–98.
Henning SW, Fernandez MF, Mahon JP, et al. HSP70iQ435A-encoding DNA repigments vitiligo lesions in sinclair swine. J Investig Dermatol. 2018;138:2531–9.
Andersson U, Yang H, Harris H. Extracellular HMGB1 as a therapeutic target in inflammatory diseases. Expert Opin Ther Targets. 2018;22:263–77.
Venereau E, De Leo F, Mezzapelle R, Careccia G, Musco G, Bianchi ME. HMGB1 as biomarker and drug target. Pharmacol Res. 2016;111:534–44.
Jacquemin C, Rambert J, Guillet S, et al. Heat shock protein 70 potentiates interferon alpha production by plasmacytoid dendritic cells: relevance for cutaneous lupus and vitiligo pathogenesis. Br J Dermatol. 2017;177:1367–75.
** Y, Andersen GHL, Santorico SA, Spritz RA. Multiple functional variants of IFIH1, a gene involved in triggering innate immune responses, protect against vitiligo. J Investig Dermatol. 2017;137:522–4.
Zhuang T, Yi X, Chen J, et al. Intracellular virus sensor MDA5 exacerbates vitiligo by inducing the secretion of chemokines in keratinocytes under virus invasion. Cell Death Dis. 2020;11:453. https://doi.org/10.1038/s41419-020-2665-z.
Bertolotti A, Boniface K, Vergier B, et al. Type I interferon signature in the initiation of the immune response in vitiligo. Pigment Cell Melanoma Res. 2014;27:398–407.
Bahloul E, Jallouli M, Garbaa S, et al. Hydroxychloroquine-induced hyperpigmentation in systemic diseases: prevalence, clinical features and risk factors: a cross-sectional study of 41 cases. Lupus. 2017;26:1304–8.
Joo K, Park W, Kwon SR, Lim MJ, Jung K-H. Improvement of vitiligo in a patient with rheumatoid arthritis after hydroxychloroquine treatment. Int J Rheum Dis. 2015;18:679–80.
Pellerin A, Otero K, Czerkowicz JM, et al. Anti-BDCA2 monoclonal antibody inhibits plasmacytoid dendritic cell activation through Fc-dependent and Fc-independent mechanisms. EMBO Mol Med. 2015;7:464–76.
Furie R, Werth VP, Merola JF, et al. Monoclonal antibody targeting BDCA2 ameliorates skin lesions in systemic lupus erythematosus. J Clin Investig. 2019;129:1359–71.
Khamashta M, Merrill JT, Werth VP, et al. Sifalimumab, an anti-interferon-α monoclonal antibody, in moderate to severe systemic lupus erythematosus: a randomised, double-blind, placebo-controlled study. Ann Rheum Dis. 2016;75:1909–16.
Furie R, Khamashta M, Merrill JT, et al. Anifrolumab, an anti-interferon-α receptor monoclonal antibody, in moderate-to-severe systemic lupus erythematosus. Arthritis Rheumatol. 2017;69:376–86.
Laddha NC, Dwivedi M, Mansuri MS, et al. Association of neuropeptide Y (NPY), interleukin-1B (IL1B) genetic variants and correlation of IL1B transcript levels with vitiligo susceptibility. PLoS ONE. 2014;9:e107020. https://doi.org/10.1371/journal.pone.0107020.
Marie J, Kovacs D, Pain C, et al. Inflammasome activation and vitiligo/nonsegmental vitiligo progression. Br J Dermatol. 2014;170:816–23.
Lamkanfi M, Vande Walle L, Kanneganti T-D. Deregulated inflammasome signaling in disease. Immunol Rev. 2011;243:163–73.
Nicolaidou E, Antoniou C, Stratigos AJ, Stefanaki C, Katsambas AD. Efficacy, predictors of response, and long-term follow-up in patients with vitiligo treated with narrowband UVB phototherapy. J Am Acad Dermatol. 2007;56:274–8.
Richmond JM, Strassner JP, Zapata L, et al. Antibody blockade of IL-15 signaling has the potential to durably reverse vitiligo. Sci Transl Med. 2018;10(450):eaam7710. https://doi.org/10.1126/scitranslmed.aam7710.
Khalil S, Bardawil T, Kurban M, Abbas O. Tissue-resident memory T cells in the skin. Inflamm Res. 2020;69(3):245–54.
Sasson SC, Gordon CL, Christo SN, Klenerman P, Mackay LK. Local heroes or villains: tissue-resident memory T cells in human health and disease. Cell Mol Immunol. 2020;17:113–22.
Ho AW, Kupper TS. T cells and the skin: from protective immunity to inflammatory skin disorders. Nat Rev Immunol. 2019;19:490–502.
Frączek A, Owczarczyk-Saczonek A, Placek W. The role of TRM cells in the pathogenesis of vitiligo-a review of the current state-of-the-art. Int J Mol Sci. 2020;21:3552. https://doi.org/10.3390/ijms21103552.
Pan Y, Kupper TS. Metabolic reprogramming and longevity of tissue-resident memory T cells. Front Immunol. 2018;9:1347. https://doi.org/10.3389/fimmu.2018.01347.
Pan Y, Tian T, Park CO, et al. Survival of tissue-resident memory T cells requires exogenous lipid uptake and metabolism. Nature. 2017;543:252–6.
Boniface K, Jacquemin C, Darrigade A-S, et al. Vitiligo skin is imprinted with resident memory CD8 T cells expressing CXCR3. J Invest Dermatol. 2018;138:355–64.
Speeckaert R, Speeckaert M, De Schepper S, van Geel N. Biomarkers of disease activity in vitiligo: a systematic review. Autoimmun Rev. 2017;16:937–45.
Rashighi M, Agarwal P, Richmond JM, et al. CXCL10 is critical for the progression and maintenance of depigmentation in a mouse model of vitiligo. Sci Transl Med. 2014;6:223ra23. https://doi.org/10.1126/scitranslmed.3007811.
Nguyen S, Chuah SY, Fontas E, et al. Atorvastatin in combination with narrowband UV-B in adult patients with active vitiligo: a randomized clinical trial. JAMA Dermatol. 2018;154:725–6.
Vanderweil SG, Amano S, Ko W-C, et al. A double-blind, placebo-controlled, phase-II clinical trial to evaluate oral simvastatin as a treatment for vitiligo. J Am Acad Dermatol. 2017;76(150–151):e3.
Richmond JM, Masterjohn E, Chu R, Tedstone J, Youd ME, Harris JE. CXCR3 depleting antibodies prevent and reverse vitiligo in mice. J Invest Dermatol. 2017;137:982–5.
Jacquemin C, Martins C, Lucchese F, et al. NKG2D defines a subset of skin effector memory CD8 T cells with proinflammatory functions in vitiligo. J Invest Dermatol. 2020;140(6):1143–53.e5.
Vadstrup K, Bendtsen F. Anti-NKG2D mAb: a new treatment for Crohn’s disease? Int J Mol Sci. 2017;18:1997. https://doi.org/10.3390/ijms1809199
Martins C, Darrigade A-S, Jacquemin C, et al. Phenotype and function of circulating memory T cells in human vitiligo. Br J Dermatol. 2020. https://doi.org/10.1111/bjd.18902.
Czarnowicki T, He H, Leonard A, et al. Blood endoty** distinguishes the profile of vitiligo from that of other inflammatory and autoimmune skin diseases. J Allergy Clin Immunol. 2019;143:2095–107.
Horvath CM. The Jak-STAT pathway stimulated by interferon gamma. Sci STKE. 2004;2004:tr8. https://doi.org/10.1126/stke.2602004tr8.
Li J, Yin Q, Wu H. Structural basis of signal transduction in the TNF receptor superfamily. Adv Immunol. 2013;119:135–53.
Yang L, Yang S, Lei J, et al. Role of chemokines and the corresponding receptors in vitiligo: a pilot study. J Dermatol. 2018;45:31–8.
Richmond JM, Bangari DS, Essien KI, et al. Keratinocyte-derived chemokines orchestrate T-cell positioning in the epidermis during vitiligo and may serve as biomarkers of disease. J Invest Dermatol. 2017;137:350–8.
Natarajan VT, Ganju P, Singh A, et al. IFN-γ signaling maintains skin pigmentation homeostasis through regulation of melanosome maturation. Proc Natl Acad Sci USA. 2014;111:2301–6.
Natarajan VT, Ganju P, Ramkumar A, Grover R, Gokhale RS. Multifaceted pathways protect human skin from UV radiation. Nat Chem Biol. 2014;10:542–51.
Boukhedouni N, Martins C, Darrigade A-S, et al. Type-1 cytokines regulate MMP-9 production and E-cadherin disruption to promote melanocyte loss in vitiligo. JCI Insight. 2020;5. https://doi.org/10.1172/jci.insight.133772.
Singh RK, Lee KM, Vujkovic-Cvi** I, et al. The role of IL-17 in vitiligo: a review. Autoimmun Rev. 2016;15:397–404.
Pincelli C, Schafer PH, French LE, Augustin M, Krueger JG. Mechanisms underlying the clinical effects of apremilast for psoriasis. J Drugs Dermatol. 2018;17:835–40.
Zebda R, Paller AS. Phosphodiesterase 4 inhibitors. J Am Acad Dermatol. 2018;78:S43–52.
Khaled M, Levy C, Fisher DE. Control of melanocyte differentiation by a MITF-PDE4D3 homeostatic circuit. Genes Dev. 2010;24:2276–81.
Huff SB, Gottwald LD. Repigmentation of tenacious vitiligo on apremilast. Case Rep Dermatol Med. 2017;2017:2386234. https://doi.org/10.1155/2017/2386234.
Khemis A, Fontas E, Moulin S, Montaudié H, Lacour J-P, Passeron T. Apremilast in combination with narrowband UVB in the treatment of vitiligo: a 52-week monocentric prospective randomized placebo-controlled study. J Invest Dermatol. 2020; 140(8):1533–37.e2.
Webb KC, Tung R, Winterfield LS, et al. Tumour necrosis factor-α inhibition can stabilize disease in progressive vitiligo. Br J Dermatol. 2015;173:641–50.
Alghamdi KM, Khurrum H, Taieb A, Ezzedine K. Treatment of generalized vitiligo with anti-TNF-α agents. J Drugs Dermatol. 2012;11:534–9.
Toussirot É, Aubin F. Paradoxical reactions under TNF-α blocking agents and other biological agents given for chronic immune-mediated diseases: an analytical and comprehensive overview. RMD Open. 2016;2:e000239. https://doi.org/10.1136/rmdopen-2015-000239.
Méry-Bossard L, Bagny K, Chaby G, et al. New-onset vitiligo and progression of pre-existing vitiligo during treatment with biological agents in chronic inflammatory diseases. J Eur Acad Dermatol Venereol. 2017;31:181–6.
Bae JM, Kim M, Lee HH, et al. Increased risk of vitiligo following anti-tumor necrosis factor therapy: a 10-year population-based cohort study. J Investg Dermatol. 2018;138:768–74.
van den Boorn JG, Konijnenberg D, Dellemijn TAM, et al. Autoimmune destruction of skin melanocytes by perilesional T cells from vitiligo patients. J Invest Dermatol. 2009;129:2220–32.
Speeckaert R, Mylle S, van Geel N. IL-17A is not a treatment target in progressive vitiligo. Pigment Cell Melanoma Res. 2019;32:842–7.
Mobasher P, Guerra R, Li SJ, Frangos J, Ganesan AK, Huang V. Open-label pilot study of tofacitinib 2% for the treatment of refractory vitiligo. Br J Dermatol. 2020;182:1047–9.
McKesey J, Pandya AG. A pilot study of 2% tofacitinib cream with narrowband ultraviolet B for the treatment of facial vitiligo. J Am Acad Dermatol. 2019;81:646–8.
Kim SR, Heaton H, Liu LY, King BA. Rapid repigmentation of vitiligo using tofacitinib plus low-dose, narrowband UV-B phototherapy. JAMA Dermatol. 2018;154:370–1.
Vu M, Heyes C, Robertson SJ, Varigos GA, Ross G. Oral tofacitinib: a promising treatment in atopic dermatitis, alopecia areata and vitiligo. Clin Exp Dermatol. 2017;42:942–4.
Craiglow BG, King BA. Tofacitinib citrate for the treatment of vitiligo: a pathogenesis-directed therapy. JAMA Dermatol. 2015;151:1110–12.
Joshipura D, Alomran A, Zancanaro P, Rosmarin D. Treatment of vitiligo with the topical Janus kinase inhibitor ruxolitinib: a 32-week open-label extension study with optional narrow-band ultraviolet B. J Am Acad Dermatol. 2018;78:1205.e1–7.e1.
Rothstein B, Joshipura D, Saraiya A, et al. Treatment of vitiligo with the topical Janus kinase inhibitor ruxolitinib. J Am Acad Dermatol. 2017;76(6):1054-60.e1.
Harris JE, Rashighi M, Nguyen N, et al. Rapid skin repigmentation on oral ruxolitinib in a patient with coexistent vitiligo and alopecia areata (AA). J Am Acad Dermatol. 2016;74:370–1.
Rosmarin D, Pandya AG, Lebwohl M, et al. Ruxolitinib cream for treatment of vitiligo: a randomised, controlled, phase 2 trial. Lancet. 2020;396:110–20.
Spritz RA. Recent progress in the genetics of generalized vitiligo. J Genet Genom. 2011;38:271–8.
Dwivedi M, Kemp EH, Laddha NC, Mansuri MS, Weetman AP, Begum R. Regulatory T cells in vitiligo: implications for pathogenesis and therapeutics. Autoimmun Rev. 2015;14:49–56.
Eby JM, Kang H-K, Tully ST, et al. CCL22 to activate treg migration and suppress depigmentation in vitiligo. J Invest Dermatol. 2015;135:1574–80.
Tahvildari M, Dana R. Low-dose IL-2 therapy in transplantation, autoimmunity, and inflammatory diseases. J Immunol. 2019;203:2749–55.
Castela E, Le Duff F, Butori C, et al. Effects of low-dose recombinant interleukin 2 to promote T-regulatory cells in alopecia areata. JAMA Dermatol. 2014;150:748–51.
Schallreuter KU, Wood JM, Berger J. Low catalase levels in the epidermis of patients with vitiligo. J Invest Dermatol. 1991;97:1081–5.
Speeckaert R, Dugardin J, Lambert J,et al. Critical appraisal of the oxidative stress pathway in vitiligo: a systematic review and meta-analysis. J Eur Acad Dermatol Venereol. 2018;32:1089–98.
Mercuri SR, Vollono L, Paolino G. The usefulness of platelet-rich plasma (PRP) for the treatment of vitiligo: state of the art and review. Drug Des Dev Ther. 2020;14:1749–55.
Luger TA, Scholzen T, Grabbe S. The role of alpha-melanocyte-stimulating hormone in cutaneous biology. J Investig Dermatol Symp Proc. 1997;2:87–93.
Thody AJ. alpha-MSH and the regulation of melanocyte function. Ann N Y Acad Sci. 1999;885:217–29.
Eves PC, MacNeil S, Haycock JW. Alpha-melanocyte stimulating hormone, inflammation and human melanoma. Peptides. 2006;27:444–52.
Lim HW, Grimes PE, Agbai O, et al. Afamelanotide and narrowband UV-B phototherapy for the treatment of vitiligo: a randomized multicenter trial. JAMA Dermatol. 2015;151:42–50.
Grimes PE, Hamzavi I, Lebwohl M, Ortonne JP, Lim HW. The efficacy of afamelanotide and narrowband UV-B phototherapy for repigmentation of vitiligo. JAMA Dermatol. 2013;149:68–73.
Regazzetti C, Joly F, Marty C, et al. Transcriptional analysis of vitiligo skin reveals the alteration of WNT pathway: a promising target for repigmenting vitiligo patients. J Invest Dermatol. 2015;135:3105–14.
Cavalié M, Ezzedine K, Fontas E, et al. Maintenance therapy of adult vitiligo with 01% tacrolimus ointment: a randomized, double blind, placebo-controlled study. J Invest Dermatol. 2015;135:970–4.
Acknowledgements
Funding
No funding or sponsorship was received for this study or publication of this article.
Authorship
All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this article, take responsibility for the integrity of the work as a whole, and have given their approval for this version to be published.
Disclosures
Laure Migayron, Katia Boniface, and Julien Seneschal have nothing to declare.
Compliance with Ethics Guidelines
This article is based on previously conducted studies and does not contain any studies with human participants or animals performed by any of the authors.
Author information
Authors and Affiliations
Corresponding author
Additional information
Digital Features
To view digital features for this article go to https://doi.org/10.6084/m9.figshare.12928409.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Migayron, L., Boniface, K. & Seneschal, J. Vitiligo, From Physiopathology to Emerging Treatments: A Review. Dermatol Ther (Heidelb) 10, 1185–1198 (2020). https://doi.org/10.1007/s13555-020-00447-y
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13555-020-00447-y