Abstract
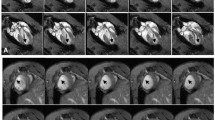
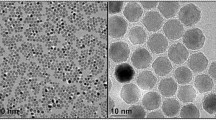
Migration of stem cells after transplantation reduces their therapeutic effects. In this study, we hypothesized that superparamagnetic iron oxide nanoparticles (SPION)-labeled mesenchymal stem cells (MSCs) in the presence of magnetic field may have a capability to increase regenerative ability after heart failure (HF). A rat model of ISO (isoproterenol)-HF was established to investigate the effects of SPION-labeled MSCs on tissue regeneration in the presence and absence of magnetic field. Hydrodynamic size, shape, and formation of chemical bonds between SPION and polyethylene glycol (PEG) were measured using dynamic light scattering (DLS), transmission electron microscopy (TEM), and Fourier-transform infrared spectroscopy (FTIR). The MRI was used to monitor SPION-labeled MSCs in vivo. Cell and tissue uptake of nanoparticles were determined by Prussian blue staining, atomic absorption spectroscopy (AAS), and inductively coupled plasma spectroscopy (ICP). Purity of the MSCs, heart function, myocardial fibrosis, and histologic damage were evaluated using flow-cytometry, echocardiography, Masson’s trichrome, and H&E staining respectively. Various spectroscopic and microscopic analyses revealed that hydrodynamic size of SPION was 40 ± 2 and their shape was spherical. FTIR confirmed the presence of PEG on the surface of nanoparticles. The presence of magnetic field significantly increased cell homing. Highly purified MSCs population was detected by flow-cytometry. Using SPION-labeled MSCs in the presence of magnetic field markedly improved heart function and myocardial hypertrophy and reduced fibrosis (p < 0.05). Collectively, our results demonstrated that SPION-labeled MSCs in the presence of magnetic field might contribute to regeneration after HF.






Similar content being viewed by others
Change history
22 February 2024
A Correction to this paper has been published: https://doi.org/10.1007/s13346-024-01549-2
Abbreviations
- SPION:
-
Superparamagnetic iron oxide nanoparticles
- MSCs:
-
Mesenchymal stem cells
- hAMSCs:
-
Human amniotic mesenchymal stromal cells
- DLS:
-
Dynamic light scattering
- HF:
-
Heart failure
- ISO:
-
Isoproterenol
- ISO-HF:
-
ISO-induced heart failure
- TEM:
-
Transmission electron microscopy
- FTIR:
-
Fourier-transform infrared spectroscopy
- 2D:
-
Two dimensional
- PEG:
-
Polyethylene glycol
- ICP:
-
Inductively coupled plasma spectroscopy
- MRI:
-
Magnetic resonance imaging
- AAS:
-
Atomic absorption spectroscopy
- VSM:
-
Vibrating sample magnetometer
- EF:
-
Ejection fraction
- FS:
-
Fractional shortening
- LVDd:
-
Left ventricular diameter in diastole
- LVDs:
-
Left ventricular diameter in systole
- H&E:
-
Hematoxylin and eosin
- FACS:
-
Fluorescence-activated cell sorting
- DMEM:
-
Dulbecco’s modified Eagle’s medium
- FBS:
-
Fetal bovine serum
- MDT:
-
Magnetic drug targeting
- MTE:
-
Magnetic tissue engineering
References
Murray SA, Boyd K, Kendall M, Worth A, Benton TF, Clausen H. Dying of lung cancer or cardiac failure: prospective qualitative interview study of patients and their carers in the community. Bmj. 2002;325(7370):929.
Bellumkonda L, Tyrrell D, Hummel SL, Goldstein DR. Pathophysiology of heart failure and frailty: a common inflammatory origin? Aging Cell. 2017;16:444–50.
Teerlink JR, Metra M, Filippatos GS, Davison BA, Bartunek J, Terzic A, et al. Benefit of cardiopoietic mesenchymal stem cell therapy on left ventricular remodelling: results from the Congestive Heart Failure Cardiopoietic Regenerative Therapy (CHART-1) study. Eur J Heart Fail. 2017;19(11):1520–9.
Sougawa, N., et al., Novel stem cell niches laminin 511 promotes functional angiogenesis through enhanced stem cell homing by modulating “stem cell beds” in the failed heart. 2017, Am Heart Assoc.
Han J, Kim B, Shin JY, Ryu S, Noh M, Woo J, et al. Iron oxide nanoparticle-mediated development of cellular gap junction crosstalk to improve mesenchymal stem cells’ therapeutic efficacy for myocardial infarction. ACS Nano. 2015;9(3):2805–19.
Bing W, Pang X, QU Q, Bai X, Yang W, Bi Y, et al. Simvastatin improves the homing of BMSCs via the PI3K/AKT/miR-9 pathway. J Cell Mol Med. 2016;20(5):949–61.
Jiang Q, Yu T, Huang K, Zhang H, Zheng Z, Hu S. Systemic redistribution of the intramyocardially injected mesenchymal stem cells by repeated remote ischaemic post-conditioning. J Cell Mol Med. 2018;22(1):417–28.
Ottersbach A, Mykhaylyk O, Heidsieck A, Eberbeck D, Rieck S, Zimmermann K, et al. Improved heart repair upon myocardial infarction: combination of magnetic nanoparticles and tailored magnets strongly increases engraftment of myocytes. Biomaterials. 2018;155:176–90.
Amani H, Habibey R, Hajmiresmail SJ, Latifi S, Pazoki-Toroudi H, Akhavan O. Antioxidant nanomaterials in advanced diagnoses and treatments of ischemia reperfusion injuries. J Mater Chem B. 2017;5(48):9452–76.
Jazayeri M, et al. Enhanced detection sensitivity of prostate-specific antigen via PSA-conjugated gold nanoparticles based on localized surface plasmon resonance: GNP-coated anti-PSA/LSPR as a novel approach for the identification of prostate anomalies. Cancer Gene Ther. 2016;23(10):365–9.
Jazayeri MH, Amani H, Pourfatollah AA, Pazoki-Toroudi H, Sedighimoghaddam B. Various methods of gold nanoparticles (GNPs) conjugation to antibodies. Sensing and bio-sensing research. 2016;9:17–22.
Wadajkar SA, et al. Design and application of magnetic-based theranostic nanoparticle systems. Recent Patents on Biomedical Engineering. 2013;6(1):47–57.
Taylor A, Wilson KM, Murray P, Fernig DG, Lévy R. Long-term tracking of cells using inorganic nanoparticles as contrast agents: are we there yet? Chem Soc Rev. 2012;41(7):2707–17.
Bernsen MR, Moelker AD, Wielopolski PA, van Tiel ST, Krestin GP. Labelling of mammalian cells for visualisation by MRI. Eur Radiol. 2010;20(2):255–74.
Shen WB, Vaccaro DE, Fishman PS, Groman EV, Yarowsky P. SIRB, sans iron oxide rhodamine B, a novel cross-linked dextran nanoparticle, labels human neuroprogenitor and SH-SY5Y neuroblastoma cells and serves as a USPIO cell labeling control. Contrast Media Mol Imaging. 2016;11(3):222–8.
Cheng K, Malliaras K, Li TS, Sun B, Houde C, Galang G, et al. Magnetic enhancement of cell retention, engraftment, and functional benefit after intracoronary delivery of cardiac-derived stem cells in a rat model of ischemia/reperfusion. Cell Transplant. 2012;21(6):1121–35.
Luciani A, Wilhelm C, Bruneval P, Cunin P, Autret G, Rahmouni A, et al. Magnetic targeting of iron-oxide-labeled fluorescent hepatoma cells to the liver. Eur Radiol. 2009;19(5):1087–96.
Verma VK, et al. Fluorescent magnetic iron oxide nanoparticles for cardiac precursor cell selection from stromal vascular fraction and optimization for magnetic resonance imaging. Int J Nanomedicine. 2015;10:711.
Li M, Gu H, Zhang C. Highly sensitive magnetite nano clusters for MR cell imaging. Nanoscale Res Lett. 2012;7(1):204.
Prabhu S, Mutalik S, Rai S, Udupa N, Rao BSS. PEGylation of superparamagnetic iron oxide nanoparticle for drug delivery applications with decreased toxicity: an in vivo study. J Nanopart Res. 2015;17(10):412.
Gupta AK, Wells S. Surface-modified superparamagnetic nanoparticles for drug delivery: preparation, characterization, and cytotoxicity studies. IEEE Transactions on Nanobiosci. 2004;3(1):66–73.
Ishida T, Wang XY, Shimizu T, Nawata K, Kiwada H. PEGylated liposomes elicit an anti-PEG IgM response in a T cell-independent manner. J Control Release. 2007;122(3):349–55.
Suk JS, Xu Q, Kim N, Hanes J, Ensign LM. PEGylation as a strategy for improving nanoparticle-based drug and gene delivery. Adv Drug Deliv Rev. 2016;99:28–51.
Estelrich J, Sánchez-Martín MJ, Busquets MA. Nanoparticles in magnetic resonance imaging: from simple to dual contrast agents. Int J Nanomedicine. 2015;10:1727.
Naseroleslami M, et al. Magnetic resonance imaging of human-derived amniotic membrane stem cells using pegylated superparamagnetic iron oxide nanoparticles. Cell J (Yakhteh). 2016;18(3):332.
Lim J, Yeap S, Che H, Low S. Characterization of magnetic nanoparticle by dynamic light scattering. Nanoscale Res Lett. 2013;8(1):381.
Andreas K, Georgieva R, Ladwig M, Mueller S, Notter M, Sittinger M, et al. Highly efficient magnetic stem cell labeling with citrate-coated superparamagnetic iron oxide nanoparticles for MRI tracking. Biomaterials. 2012;33(18):4515–25.
Moyer, M.T. and M.A. Kumar, Traumatic brain injury, in Neurocritical care for the advanced practice clinician. 2018, Springer. p. 165–181.
Amani H, Ajami M, Nasseri Maleki S, Pazoki-Toroudi H, Daglia M, Tsetegho Sokeng AJ, et al. Targeting signal transducers and activators of transcription (STAT) in human cancer by dietary polyphenolic antioxidants. Biochimie. 2017;142:63–79.
Ajami M, Pazoki-Toroudi H, Amani H, Nabavi SF, Braidy N, Vacca RA, et al. Therapeutic role of sirtuins in neurodegenerative disease and their modulation by polyphenols. Neurosci Biobehav Rev. 2017;73:39–47.
Pazoki-Toroudi H, Amani H, Ajami M, Nabavi SF, Braidy N, Kasi PD, et al. Targeting mTOR signaling by polyphenols: a new therapeutic target for ageing. Ageing Res Rev. 2016;31:55–66.
Zhang, G., et al., The application of nanomaterials in stem cell therapy for some neurological diseases. Curr Drug Targets, 2017.
Cheng K, Li TS, Malliaras K, Davis DR, Zhang Y, Marban E. Magnetic targeting enhances engraftment and functional benefit of iron-labeled cardiosphere-derived cells in myocardial infarction. Circ Res. 2010;106(10):1570–81.
Lu C-W, Hsiao JK, Liu HM, Wu CH. Characterization of an iron oxide nanoparticle labelling and MRI-based protocol for inducing human mesenchymal stem cells into neural-like cells. Sci Rep. 2017;7(1):3587.
Hamoudeh M, Faraj AA, Canet-Soulas E, Bessueille F, Léonard D, Fessi H. Elaboration of PLLA-based superparamagnetic nanoparticles: characterization, magnetic behaviour study and in vitro relaxivity evaluation. Int J Pharm. 2007;338(1–2):248–57.
Kim SJ, Lewis B, Steiner MS, Bissa UV, Dose C, Frank JA. Superparamagnetic iron oxide nanoparticles for direct labeling of stem cells and in vivo MRI tracking. Contrast Media Mol Imaging. 2016;11(1):55–64.
Vaněček V, et al. Highly efficient magnetic targeting of mesenchymal stem cells in spinal cord injury. Int J Nanomedicine. 2012;7:3719.
Hoshyar N, Gray S, Han H, Bao G. The effect of nanoparticle size on in vivo pharmacokinetics and cellular interaction. Nanomedicine. 2016;11(6):673–92.
Yanai A, Häfeli UO, Metcalfe AL, Soema P, Addo L, Gregory-Evans CY, et al. Focused magnetic stem cell targeting to the retina using superparamagnetic iron oxide nanoparticles. Cell Transplant. 2012;21(6):1137–48.
Chung HJ, Lee H, Bae KH, Lee Y, Park J, Cho SW, et al. Facile synthetic route for surface-functionalized magnetic nanoparticles: cell labeling and magnetic resonance imaging studies. ACS Nano. 2011;5(6):4329–36.
Poller WC, Löwa N, Wiekhorst F, Taupitz M, Wagner S, Möller K, et al. Magnetic particle spectroscopy reveals dynamic changes in the magnetic behavior of very small superparamagnetic iron oxide nanoparticles during cellular uptake and enables determination of cell-labeling efficacy. J Biomed Nanotechnol. 2016;12(2):337–46.
Naseroleslami M, Parivar K, Khoei S, Aboutaleb N. Optimal concentration of PEG-coated Fe3O4 nanoparticles for generation of reactive oxygen species in human-derived amniotic membrane stem cells. Adv Stud Biol. 2015;7(8):377–88.
Amsalem Y, et al. Iron-oxide labeling and outcome of transplanted mesenchymal stem cells in the infarcted myocardium. Circulation. 2007;116(11 suppl):I-38–I45.
Au K-W, Liao SY, Lee YK, Lai WH, Ng KM, Chan YC, et al. Effects of iron oxide nanoparticles on cardiac differentiation of embryonic stem cells. Biochem Biophys Res Commun. 2009;379(4):898–903.
Chaudeurge A, Wilhelm C, Chen-Tournoux A, Farahmand P, Bellamy V, Autret G, et al. Can magnetic targeting of magnetically labeled circulating cells optimize intramyocardial cell retention? Cell Transplant. 2012;21(4):679–91.
Mani V, Adler E, Briley-Saebo KC, Bystrup A, Fuster V, Keller G, et al. Serial in vivo positive contrast MRI of iron oxide-labeled embryonic stem cell-derived cardiac precursor cells in a mouse model of myocardial infarction. Magn Reson Med. 2008;60(1):73–81.
Li L, Zhang Y, Li Y, Yu B, Xu Y, Zhao SD, et al. Mesenchymal stem cell transplantation attenuates cardiac fibrosis associated with isoproterenol-induced global heart failure. Transpl Int. 2008;21(12):1181–9.
Funding
This study was supported financially by Physiology Research Center of Iran, University of Medical Sciences.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical approval
Animal Ethical Committee of Iran University of Medical Sciences approved all protocols and surgical procedures. The animals were housed five per cage in a room with controlled temperature, on 12-h:12-h light:dark schedule, moisture (40–60%) with free access to standard food and water.
Informed consent
The amniotic membranes were provided by Shahid Akbar Abadi Hospital upon informed consent of the participants in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Conflict of Interest
The authors declare that they have no conflicts of interest.
Electronic supplementary material
ESM 1
(DOCX 1003 kb)
Rights and permissions
About this article
Cite this article
Naseroleslami, M., Aboutaleb, N. & Parivar, K. The effects of superparamagnetic iron oxide nanoparticles-labeled mesenchymal stem cells in the presence of a magnetic field on attenuation of injury after heart failure. Drug Deliv. and Transl. Res. 8, 1214–1225 (2018). https://doi.org/10.1007/s13346-018-0567-8
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13346-018-0567-8