Abstract
Pediatric liver transplantation remains the gold standard for life-threatening acute and chronic liver diseases and multiple liver-based inherited metabolic defects. Advances in surgical techniques, better perioperative care and immunosuppression regimes have resulted in excellent long-term graft and patient survival. The success of pediatric liver transplantation does however bring the additional challenge of long-term patient outcomes including graft hepatitis-related fibrosis and suboptimal biopsychosocial outcomes. In this review, authors will explore the current landscape of pediatric liver transplantation including indications, timing of referral for liver transplantation, surgical techniques and long-term outcomes such as recurrence of pre-transplant liver disease, idiopathic graft hepatitis and biopsychosocial outcomes. Ultimately, early identification and management of potential issues long-term helps ensure our recipients achieve a “meaningful survival”.


Similar content being viewed by others
References
Vimalesvaran S, Souza LN, Deheragoda M, et al. Outcomes of adults who received liver transplant as young children. EClinicalMedicine. 2021;38:100987.
Rela M, Reddy MS. Pediatric liver transplantation: an asymmetrical war for access to livers. Gastroenterology. 2017;153:888–9.
Vimalesvaran S, Dhawan A. Liver transplantation for pediatric inherited metabolic liver diseases. World J Hepatol. 2021;13:1351–66.
Jagadisan B, Verma A, Dhawan A. Assessment and preparation for liver transplantation in children. In: Burra P, editor. Textbook of Liver Transplantation. Cham: Springer; 2022. p. 479–94.
Zalewska K. POLICY POL195/7 Liver Transplantation: Selection Criteria and Recipient Registration 2018. Available at: https://nhsbtdbe.blob.core.windows.net/umbraco-assets-corp/9440/pol195_7-liver-selection-policy.pdf. Accessed on 20 Mar 2018.
Freeman RB Jr, Wiesner RH, Roberts JP, McDiarmid S, Dykstra DM, Merion RM. Improving liver allocation: MELD and PELD. Am J Transplant. 2004;4:114–31.
Salvalaggio PR, Neighbors K, Kelly S, et al. Regional variation and use of exception letters for cadaveric liver allocation in children with chronic liver disease. Am J Transplant. 2005;5:1868–74.
Duffy JP, Kao K, Ko CY, et al. Long-term patient outcome and quality of life after liver transplantation: analysis of 20-year survivors. Ann Surg. 2010;252:652–61.
Seda-Neto J, Antunes da Fonseca E, Pugliese R, et al. Twenty years of experience in pediatric living donor liver transplantation: focus on hepatic artery reconstruction, complications, and outcomes. Transplantation. 2016;100:1066–72.
Horvat N, Marcelino ASZ, Horvat JV, et al. Pediatric liver transplant: techniques and complications. Radiographics. 2017;37:1612–31.
Chaubal G, Nanavati AJ, Biradar V, et al. Monosegment liver allografts for liver transplantation in infants weighing less than 6 kg: an initial indian experience. Transplant Proc. 2021;53:1670–3.
Quadros J, Piedade C, Lopes MF. Auxiliary liver transplantation for management of acute liver failure in children - systematic review. Transplant Rev (Orlando). 2021;35:100631.
Faraj W, Dar F, Bartlett A, et al. Auxiliary liver transplantation for acute liver failure in children. Ann Surg. 2010;251:351–6.
Weiner J, Griesemer A, Island E, et al. Longterm outcomes of auxiliary partial orthotopic liver transplantation in preadolescent children with fulminant hepatic failure. Liver Transpl. 2016;22:485–94.
Kato T, Selvaggi G, Levi D, et al. Routine use of auxiliary partial orthotopic liver transplantation for children with fulminant hepatic failure: preliminary report. Transplant Proc. 2006;38:3607–8.
Ciria R, Davila D, Heaton N. Auxiliary liver transplantation in children. Curr Opin Organ Transplant. 2011;16:489–93.
Oishi K, Arnon R, Wasserstein MP, Diaz GA. Liver transplantation for pediatric inherited metabolic disorders: considerations for indications, complications, and perioperative management. Pediatr Transplant. 2016;20:756–69.
Neves DB, Rusi MB, Diaz LG, Salvalaggio P. Primary graft dysfunction of the liver: definitions, diagnostic criteria and risk factors. Einstein (Sao Paulo). 2016;14:567–72.
Uemura T, Randall HB, Sanchez EQ, et al. Liver retransplantation for primary nonfunction: analysis of a 20-year single-center experience. Liver Transpl. 2007;13:227–33.
Kutluturk K, Sahin TT, Karakas S, et al. Early hepatic artery thrombosis after pediatric living donor liver transplantation. Transplant Proc. 2019;51:1162–8.
Nishida S, Kato T, Levi D, et al. Effect of protocol Doppler ultrasonography and urgent revascularization on early hepatic artery thrombosis after pediatric liver transplantation. Arch Surg. 2002;137:1279–83.
Shanmugam N, Dhawan A. Acute liver failure in children: intensive care management protocol. In: Shanmugam N, Dhawan A, editors. Pediatric Liver Intensive Care. Singapore: Springer Nature; 2018. p. 7–17.
Nacoti M, Ruggeri GM, Colombo G, Bonanomi E, Lussana F. Thrombosis prophylaxis in pediatric liver transplantation: a systematic review. World J Hepatol. 2018;10:752–60.
Kensinger CD, Sexton KW, Baron CM, Lipnik AJ, Meranze SG, Gorden DL. Management of portal vein thrombosis after liver transplantation with a combined open and endovascular approach. Liver Transpl. 2015;21:132–4.
Tannuri U, Mello ES, Carnevale FC, et al. Hepatic venous reconstruction in pediatric living-related donor liver transplantation–experience of a single center. Pediatr Transplant. 2005;9:293–8.
Gibelli NE, Tannuri AC, Andrade WC, Ricardi LR, Tannuri U. Centrilobular necrosis as a manifestation of venous outflow block in pediatric malnourished liver transplant recipients–case reports. Pediatr Transplant. 2012;16:E383–7.
Tannuri U, Tannuri AC. Postoperative care in pediatric liver transplantation. Clinics (Sao Paulo). 2014;69:42–6.
Dehghani SM, Shahramian I, Afshari M, Bahmanyar M, Ataollahi M, Sargazi A. Acute hepatic allograft rejection in pediatric recipients: effective factors. Int J Organ Transplant Med. 2018;9:41–5.
Verma A, Vimalesvaran S, Dhawan A. Epidemiology, risk factors and outcome due to multidrug resistant organisms in paediatric liver transplant patients in the era of antimicrobial stewardship and screening. Antibiotics (Basel). 2022;11:387.
Sundaram SS, Melin-Aldana H, Neighbors K, Alonso EM. Histologic characteristics of late cellular rejection, significance of centrilobular injury, and long-term outcome in pediatric liver transplant recipients. Liver Transpl. 2006;12:58–64.
Demetris A, Adams D, Bellamy C, et al. Update of the International Banff schema for liver allograft rejection: working recommendations for the histopathologic staging and reporting of chronic rejection. An International Panel Hepatology. 2000;31:792–9.
Gupta P, Hart J, Cronin D, Kelly S, Millis JM, Brady L. Risk factors for chronic rejection after pediatric liver transplantation. Transplantation. 2001;72:1098–102.
Kelly D, Verkade HJ, Rajanayagam J, McKiernan P, Mazariegos G, Hubscher S. Late graft hepatitis and fibrosis in pediatric liver allograft recipients: current concepts and future developments. Liver Transpl. 2016;22:1593–602.
Squires JE, Demetris AJ. Surveillance biopsies in pediatric liver transplantation: is the juice worth the squeeze? Liver Transpl. 2022;28:754–5.
Couchonnal E, Jacquemin E, Lachaux A, et al. Long-term results of pediatric liver transplantation for autoimmune liver disease. Clin Res Hepatol Gastroenterol. 2021;45:101537.
Jara P, Hierro L, Martinez-Fernandez P, et al. Recurrence of bile salt export pump deficiency after liver transplantation. N Engl J Med. 2009;361:1359–67.
Siebold L, Dick AA, Thompson R, et al. Recurrent low gamma-glutamyl transpeptidase cholestasis following liver transplantation for bile salt export pump (BSEP) disease (posttransplant recurrent BSEP disease). Liver Transpl. 2010;16:856–63.
Keitel V, Burdelski M, Vojnisek Z, Schmitt L, Haussinger D, Kubitz R. De novo bile salt transporter antibodies as a possible cause of recurrent graft failure after liver transplantation: a novel mechanism of cholestasis. Hepatology. 2009;50:510–7.
Mehl A, Bohorquez H, Serrano MS, Galliano G, Reichman TW. Liver transplantation and the management of progressive familial intrahepatic cholestasis in children. World J Transplant. 2016;6:278–90.
Knisely AS, Houwen RHJ. Liver steatosis and diarrhea after liver transplantation for progressive familial intrahepatic cholestasis type 1: can biliary diversion solve these problems? J Pediatr Gastroenterol Nutr. 2021;72:341–2.
Shanmugam N, Menon J, Vij M, Rammohan A, Rajalingam R, Rela M. Total internal biliary diversion for post-liver transplant PFIC-1-related allograft injury. J Clin Exp Hepatol. 2022;12:212–5.
Liu Y, Sun LY, Zhu ZJ, et al. Post-transplant lymphoproliferative disorder after paediatric liver transplantation. Int J Clin Pract. 2021;75:e13843.
Gonzalez-Barca E, Domingo-Domenech E, Capote FJ, et al. Prospective phase II trial of extended treatment with rituximab in patients with B-cell post-transplant lymphoproliferative disease. Haematologica. 2007;92:1489–94.
Bradford R, Tomlinson L. Psychological guidelines in the management of paediatric organ transplantation. Arch Dis Child. 1990;65:1000–3.
Author information
Authors and Affiliations
Contributions
All authors were involved in the writing, analysis and review of this article. AD will act as guarantor for this manuscript.
Corresponding author
Ethics declarations
Conflict of Interest
None.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Appendix
Appendix
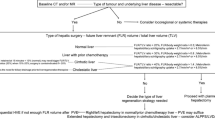
Acute liver failure super-urgent listing transplant criteria in the UK are based on National Health Service Blood and Transplant (NHSBT) criteria [5]
National Health Service Blood and Transplant (NHSBT) Criteria for Pediatric Acute Liver Failure (Super-urgent listing) |
|---|
Acute liver failure in children under two years of age: INR >4 or grade 3–4 encephalopathy |
Acute presentation of Wilson’s disease, or Budd-Chiari syndrome: A combination of coagulopathy, and any grade of encephalopathy |
Paracetamol poisoning: pH <7.25 more than 24 h after overdose and after fluid resuscitation or co-existing prothrombin time >100 s or INR >6.5, and serum creatinine >300 μmol/l or anuria, and grade 3–4 encephalopathy or persistent hyperlactatemia after adequate fluid resuscitation |
Favorable non-paracetamol etiologies such as acute viral hepatitis: The presence of clinical hepatic encephalopathy is mandatory and: prothrombin time >100 s, or INR >6.5, or any three from the following: age <10 y; prothrombin time >50 s or INR >3.5; any grade of hepatic encephalopathy with jaundice to encephalopathy time >7 d; serum bilirubin >17.5 mg/dL |
Unfavorable non-paracetamol etiologies such as seronegative or idiosyncratic drug reactions: a) prothrombin time >100 s, or INR >6.5, or b) in the absence of clinical hepatic encephalopathy then INR >2 after vitamin K repletion is mandatory and any two from the following: age <10 y; prothrombin time >50 s or INR >3.5; if hepatic encephalopathy is present then jaundice to encephalopathy time >7 d; serum bilirubin >17.5 mg/dL |
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Vimalesvaran, S., Verma, A. & Dhawan, A. Pediatric Liver Transplantation: Selection Criteria and Post-transplant Medical Management. Indian J Pediatr 91, 383–390 (2024). https://doi.org/10.1007/s12098-023-04963-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12098-023-04963-5