Abstract
Objective
To assess the effectiveness of an indigenously assembled Nasal Bubble CPAP (NB-CPAP) in children during present swine flu pandemic presenting with acute hypoxemic respiratory failure; in improving gas exchange and vital signs; and assess method safety.
Methods
Thirty Six children with acute hypoxemic respiratory failure admitted to swine flu ICU during the present H1NI pandemic were included (18 confirmed H1N1 positive and 18 confirmed H1N1 negative). After a baseline Arterial Blood Gas, all children received Oxygen via indigenous NB-CPAP Circuit which gave expiratory positive airway pressure of 5 cm water and delivered an FiO2 of around 70%. Vital signs, pH, PaO2, PaCO2, PO2/FiO2 and O2 saturation were recorded at start and at 6 h into the study.
Results
Median age of the patients was 18 months (58% males, 42% females). Respiratory rate and heart rate improved significantly with indigenous NB-CPAP after 6 h of treatment compared with admission (p < 0.0001 and p < 0.001), respectively. At the end of 6 h on NB-CPAP,PaO2 (p < 0.0001), PCO2 (p < 0.0001), PO2/FiO2 (p < 0.0002) and O2 saturation (p < 0.001) improved significantly. Median duration of NB-CPAP use was 2 days and none required endotracheal intubation. The median hospital stay was 7 days.
Conclusions
Indigenous NB-CPAP improves hypoxemia and signs and symptoms in hemodynamically stable children with acute respiratory failure due to influenza like illness. It is a cost-effective, safe, well tolerated circuit in highly demanding pandemic situations and may prevent progression to intubation.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Acute hypoxemic respiratory failure (AHRF) is a major cause of morbidity and mortality in children. This was evident during the present H1N1 pandemic. Several treatments are used to help increase blood oxygen levels in respiratory failure and thereby reduce organ damage and the risk of death. Ventilation under positive pressure is generally the most frequent support therapy, although known to be attended by complications [1].
Continuous positive airway pressure (CPAP) is defined as positive end expiratory pressure (PEEP) applied to a spontaneously breathing patient. Maintaining positive pressure in the alveoli improves alveolar ventilation and oxygenation by increasing functional residual capacity, decreasing pulmonary edema, and minimizing expiratory bronchiolar collapse. The continuous flow of gas given throughout the respiratory cycle also assists in reducing the patient’s work of breathing [2, 3].
In Bubble CPAP, the positive pressure is achieved by kee** the efferent limb of the exhale tubing under water and the gas flow adjusted to maintain constant bubbling. The depth of the exhale tubing under water determines the amount of CPAP applied to the system. This has been primarily used in neonatal units only to manage neonatal respiratory distress.
Sassoon General Hospital (SGH) is a large government tertiary care public teaching hospital, which serves Pune (a city of 4 million in Western India) and surrounding peri-urban and rural areas. At the height of the first wave epidemic in Pune, a dedicated H1N1 ward and intensive care unit (ICU) were established at SGH and the hospital became the major referral center for children with influenza-like illness requiring hospitalization and ICU care in the region.
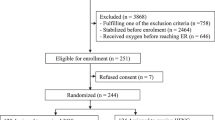
The authors indigenously prepared a Nasal bubble CPAP circuit (Fig. 1) that could be easily set up at the patients’ bedside and administer an end expiratory pressure of 5 cm of water with an FiO2 of 70% (confirmed on FiO2 analyzer); costing Rs 250/- only. The pressure was generated by connecting one tube to the oxygen flow rate of 10 L/min and exhale tube placed underwater at 5 cms into the saline filled bottle (Fig. 2). Ventilatory support was thus provided avoiding the complications of endotracheal intubation. In addition, the upper airway remained intact, whereas both physiologic functions and defense mechanisms were preserved.
Indigenous assembly of Nasal Bubble CPAP. 1 O2 supply: Central O2—Inhale tube of nasal prongs attached. Other tube close as shown. Flow rate of O2; 10 L/min. 2 Pediatric nasal cannula. 3 IV tubing cut and one end attached to exhale tube of nasal prongs and the other end put on the normal saline bottle immersed at 5 cm inside (giving 5 cm water pressure). 4 Normal saline bottle showing bubbles and the exhale tube at 5 cm length from liquid level
To the best of authors’ knowledge this is first time that an indigenously prepared Bubble Nasal CPCP circuit has been used in managing acute hypoxemic respiratory failure in children under pandemic situations.
Material and Methods
Children presenting with severe respiratory distress who were suspected to have Influenza Like Illness (ILI) during the present H1N1 pandemic in Pune,India and admitted to Swine Flu ICU, were enrolled in the study from August 2009 through November 2009.The inclusion criteria were: child of 0 to 12 years of age with ILI having evidence of moderate to severe respiratory distress –dyspnea, tachypnea, and use of accessory muscles and who had respiratory failure (oxygen requirement >40% for maintaining oxygen saturation >94%). Children of age >12 years and who had Shock which was refractory to volume expansion and dopamine, apneas or PaO2/FiO2 < 200 (ARDS), were excluded from this study. Informed consent was taken from parents and the institutional ethics committee approval was obtained.
All patients received NB—CPAP (with FiO2 70%) and oxygen was supplied through a circuit connection; flow between 6 to 8 L/min to keep saturation >94%. Those with evidence of wheeze, received nebulised salbutamol as needed. Whenever bacterial infection was suspected, antibiotics were given. All patients were given IV fluids for first 6 h and received chest physiotherapy, as required. When sedation was needed, chloral hydrate 30–50 mg/kg every 6–8 h by mouth or midazolam bolus 0.1–0.2 mg/kg every 4–6 h IV was used. All patients received Syrup Oseltamivir in appropriate doses, as per government of India guidelines.
Continuous assessment of RR, HR, transdermal oxygen saturation, patient comfort, awareness level, chest elevation, use of accessory muscles, was performed. A chest radiograph was performed between 1 and 4 h after starting ventilation .A repeat Arterial Blood Gas (ABG) was done at the end of 6 h of monitoring. Patients were intubated and mechanically ventilated if they had severe respiratory distress without improvement (signs of fatigue and non-improvement of oxygenation); airway protection was required (coma, convulsions); hemodynamic instability was present or if ABG showed deterioration in the form of pH <7.25, PCO2 >45 mm Hg or PaO2/FiO2 < 200.
NB-CPAP was discontinued when respiratory distress settled and O2 saturation was above 97%. Oxygen was continued through face mask (<40%) or O2 hood if needed. Standard therapy was maintained. The primary endpoint was improvement in vital signs and gas exchange for six hours and secondary end point was the need for endotracheal intubation. Complications associated with NB-CPAP like nasal and facial skin erosions, conjunctivitis, gastric distension, and air leakage were looked for.
Statistical Analysis
The physiologic characteristics before and at the end of 6 h of NB-CPAP were compared using Student’s paired t test for continuous data and p values were calculated to illustrate the statistical significance. All analysis were conducted using STATA version 10 (College Station, Texas). Descriptive statistics included frequency analysis for categorical variables and median and range for continuous variables.
Results
Median age of the patient was 18 months with 58% males and 42% females. All the patients studied had severe respiratory distress and/or PaO2/FiO2 ratio suggestive of acute lung injury [median 278, (range 261–323)] with severe respiratory distress on admission.
Tables 1 and 2 show the vital signs and arterial blood gas changes before and 6 h after initiation of NBCPAP. RR and HR fell significantly in the first six hours of NBCPAP compared with the initial values . PaO2/FiO2 improved significantly within 6 h (p < 0.017). Changes in PaO2 was statistically significant at the end of 6 h (P < 0.0001). The O2 saturation significantly improved after 6 h of NBCPAP (p < 0.001). The duration of ICU stay and administration of NBCPAP was 2 days (range 2–5 days). None of the patients deteriorated to require endotracheal intubation. The median hospital stay was 7 days (range 6–11 days). Underlying respiratory conditions (Table 3) were—pneumonia (67%), bronchopneumonia (22%) and Empyema (11%). The nasal prongs did not cause any nasal or facial skin erosions at pressure points.
Discussion
Hypoxemia is the result of alveolar hypoventilation (with increased CO2) and altered ventilation/perfusion ratio. It is treated by increasing oxygen concentration and recruiting airspaces. Positive pressure improves tidal volume, gas exchange, respiratory frequency, and diaphragm activity in both chronic respiratory failure [4–6] and acute lung injury [7], proportionate to the level of applied pressure.
In 1996, Meduri et al. [8] concluded that utilization of NIV in clinical practice is a safe and an effective alternative to endotracheal intubation in hemodynamically stable patients with hypoxemic and hypercapnic respiratory failure.
As Nasal Bubble CPAP (NBCPAP) was first developed for use in premature infants, most of the literature on nasal bubble CPAP pertains to its use in this specialist group. Since 1987, when nasal bubble CPAP was found to reduce the rate of chronic lung disease in premature infants [9], ongoing studies have found nasal bubble CPAP to be a simple inexpensive therapy that decreases respiratory fatigue in premature infants, thereby playing a valuable role in weaning from positive pressure ventilation [10, 11].
The literature discussing the use of nasal bubble CPAP in infants with bronchiolitis is scarce. Soong et al. [12] studied 10 infants with bronchiolitis and impending respiratory failure in a non-randomized study. They reported improvement in symptoms, signs and physiologic parameters (heart rate, respiratory rate, PaCO2 and oxygenation index) after 2 h of CPAP via double nasal prongs.
NBCPAP has not been used so far in acute hypoxemic respiratory failure (AHRF) due to acute lung injury (ALI) under pandemic H1N1 scenario. ALI is defined as acute onset, severe arterial hypoxemia (PaO2/FiO2 between 200–300), bilateral pulmonary infiltrates and no evidence of left atrial hypertension [13].
CPAP is achieved using a conventional ventilator or CPAP driver, whereas in Bubble CPAP,the positive pressure is achieved by kee** the efferent limb of the exhale tubing under water and the gas flow adjusted to maintain constant bubbling. The depth of the exhale tubing under water determines the amount of CPAP applied to the system.
The present study shows that both infants and children upto 5 years with acute hypoxemic respiratory failure are able to tolerate indigenous NB-CPAP and gives evidence of clinical and laboratory improvement. Another major feature of NB-CPAP is easy installation of non-invasive support, before respiratory muscle fatigue sets in and atelectasis appears. Indigenous assembly of NB-CPAP costs only Rs 250/- for the circuit as compared to Rs 5 lakhs from commercial Bubble CPAP. It is tolerated well by infants and children.
There are descriptive series of pediatric patients with pneumonia and asthma responding to bilevel face mask pressure [14, 15]. In a descriptive trial of 42 patients with NIV, however, only 10 of 18 patients with pneumonia and bronchiolitis responded to positive pressure, which was administered to young infants through a nasal mask [16].
A prospective randomized crossover study suggests that Inspiratory Positive Airway Pressure/Expiratory Positive Airway Pressure for 2 h can be effective in patients with lower airway obstruction by reducing respiratory effort [17]. In the authors’ view, patient’s response is dependent on adequate application of inspiratory and expiratory pressure to obtain alveolar opening and counteract intrinsic positive end expiratory pressure, thus, reducing the respiratory effort and also preventing fatigue and need for intubation.
The present indigenous NBCPAP circuit, being at the patient’s bedside, plays a major role to ensure appropriate positive end-expiratory pressure level, avoids triggering respiratory effort, and ensures patient comfort with respiratory muscles at rest.
In the present series, no patient needed intubation. One of the reasons might be the degree of hypoxemia (PaO2/FiO2) being in ALI range (<300) rather than ARDS (<200) range. There was sustained oxygenation in the first 6 h with less lung damage and reduced respiratory fatigue.
Unlike the complications seen by Yanez LJ et al. [18], Fortenberry et al. [14] and Padman et al. [15] with use of nasal prongs or facial mask to deliver CPAP, the present series did not show any such problem. No gastric distension was found in this series as the pressure applied did not exceed the opening pressure of the inferior esophageal pressure [19]. None of the patients died. Unlike other series using CPAP, the authors’ included no patient with chronic disease [14–16] and sought to show that early management of acute respiratory failure seems to prevent such outcome.
Conclusions
The present findings suggest that the indigenous assembly of NB-CPAP applied to children with AHRF due to ALI can improve oxygenation, reduce respiratory effort and diminish the need for intubation, especially if applied early on.
Further randomized controlled trials are needed on larger number of patients to determine the role of indigenously assembled NB-CPAP in specific disease, e.g., asthma, ARDS, chronic pulmonary disease, mechanical ventilation weaning, avoiding intubation, decreasing hospital stays, and decreasing complications.
References
Shah PS, Ohlsson A, Shah JP. Continuous negative extra thoracic pressure or continuous positive airway pressure for acute hypoxemic respiratory failure in children. Cochrane Database Syst Rev. 2003;3:CD003699.
Marshall A, Pittard M. Use of continuous positive airway pressure (CPAP) in the critically ill—physiological principles. Aust Crit Care. 1999;12:154–8.
Pirret AM. Acute care nursing: a physiological approach to clinical assessment and patient care. Auckland: Alison Pirret; 2005.
Ambrosino N, Nava S, Bertone P, Frachhia C, Rampulla C. Physiologic evaluation of pressure support ventilation by nasal mask in patients with stable COPD. Chest. 1992;101:385–91.
Carrey Z, Gottfried SB, Levy RD. Ventilatory muscle support in respiratory failure with nasal positive pressure ventilation. Chest. 1990;97:150–8.
Vitacca M, Clini E, Pagani M, Bianchi L, Rossi A, Ambrosino N. Physiologic effects of early administered mask proportional assist ventilation in patients with chronic obstructive pulmonary disease and acute respiratory failure. Crit Care Med. 2000;28:1791–7.
L’Her E, Deye N, Lellouche F, et al. Physiologic effects of noninvasive ventilation during acute lung injury. Am J Respir Criti Care Med. 2005;172:1112–8.
Meduri GU, Turner RE, Abou-Shala N, Wunderink R, Tolley E. Noninvasive positive pressure ventilation via face mask- First-line intervention in patients with acute hypercapnic and hypoxemic respiratory failure. Chest. 1996;109:179–93.
Avery ME, Tooley W, Keller JB, et al. Is chronic lung disease in low birth weight infants preventable? A survey of eight centers. Pediatrics. 1987;79:26–9.
Ho JJ, Subramaniam P, Henderson-Smart DJ, Davis PG. Continuous distending pressure for respiratory distress in preterm infants. Cochrane Database of Systematic Reviews 2002, Issue 2. Art. No.: CD002271. DOI: 10.1002/14651858.CD002271
Koti J, Murki S, Gaddam P, Reddy A, Reddy M. Bubble CPAP for respiratory distress syndrome in preterm infants. Indian Pediatr. 2010;47:139–43.
Soong WJ, Hwang B, Tang RB. Continuous positive airway pressure by nasal prongs in bronchiolitis. Paediatr Pulmonol. 1993;16:163–6.
Adrienne G. Management of acute lung injury and acute respiratory syndrome in children. Crit Care Med. 2009;37:2448–54.
Fortenberry JD, Del Toro J, Jefferson LS, Evey L, Haase D. Management of pediatric acute hypoxemic respiratory insufficiency with bilevel positive pressure (BiPAP) nasal mask ventilation. Chest. 1995;108:1059–64.
Padman R, Lawless ST, Kettrick RG. Noninvasive ventilation via bilevel positive airway pressure support in pediatric practice. Crit Care Med. 1998;26:169–73.
Bernet V, Hug MI, Frey F. Predictive factors for the success of noninvasive mask ventilation in infants and children with acute respiratory failure. Pediatr Crit Care Med. 2005;6:660–4.
Thill PJ, Mc Guire JK, Baden HP, Green TP, Checchia PA. Noninvasive positive-pressure ventilation in children with lower airway obstruction. Pediat Crit Care Med. 2004;5:337–42.
Yanez LJ, Yunge M, Emilfork M, et al. A prospective, randomized, controlled trial of noninvasive ventilation in pediatric acute respiratory failure. Pediatr Crit care Med. 2008;9:484–9.
Mittal RK, Balaban DH. The esophagogastric junction. N Engl J Med. 1997;336:924–32.
Contributions
AK and RK designed the study. RK and CV recruited the subjects andcollected the data. AK, RK and NG monitored the patient recruitment and data collection.AK and NG analyzed data and wrote the manuscript with inputs from RK and CV. Allauthors approved the final manuscript.
Conflict of Interest
None.
Role of Funding Source
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Kinikar, A., Kulkarni, R., Valvi, C. et al. Use of Indigenous Bubble CPAP during Swine Flu Pandemic in Pune, India. Indian J Pediatr 78, 1216–1220 (2011). https://doi.org/10.1007/s12098-011-0389-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12098-011-0389-x