Abstract
Purpose
To analyze the differences in the cardiometabolic profile in patients with nonfunctioning adrenal incidentalomas (NFAI) with post-dexamethasone suppression test (DST) cortisol ≤1.4 µg/dL (NFAI ≤ 1.4) and those with post-DST cortisol >1.4 µg/dL (NFAI > 1.4) and between NFAI with post-DST cortisol ≤0.9 µg/dL (NFAI ≤ 0.9) and those with levels >0.9 µg/dL (NFAI > 0.9).
Methods
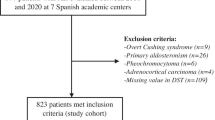
Multicenter retrospective observational study of patients with NFAIs. NFAI was defined as an adrenal incidentaloma with negative hormonal study (including metanephrines, post-DST cortisol ≤1.8 µg/dL and aldosterone/renin ratio when screening was indicated). Autonomous cortisol secretion (ACS) development was defined as an NFAIs in which post-DST serum cortisol >1.8 µg/dL were evidenced during hormonal follow-up evaluation.
Results
A total of 593 NFAI were included. Based on the 1.4 µg/dL threshold in the DST, most of the NFAI were classified as NFAI ≤ 1.4 (74.5%). Patients in the NFAI > 1.4 group were older than those in the NFAI ≤ 1.4 group, but there was no difference in the cardiometabolic profile after adjusting for age. A total of 69.5% of the patients had DST > 0.9 µg/dl. They were older and had a higher prevalence of cardiovascular disease than NFAI ≤ 0.9, even after adjusting by age (adjusted OR = 2.23 [1.10–4.53]). Patients in the NFAI > 1.4 group developed ACS more commonly than the NFAI ≤ 1.4 group (23.5% vs. 7.44%, P < 0.001). However, when the threshold of 0.9 µg/dL was considered, no difference was found between NFAI ≤ 0.9 and NFAI > 0.9 (P = 0.126).
Conclusion
The threshold of 1.4 µg/dL in the DST is useful to predict which patients with NFAI had a higher risk of ACS development during follow-up; and the threshold of 0.9 µg/dL to identify those patients with NFAI with a higher cardiovascular risk.


Similar content being viewed by others
References
M. Terzolo, A. Stigliano, I. Chiodini, P. Loli, L. Furlani, G. Arnaldi et al. AME position statement on adrenal incidentaloma. Eur. J. Endocrinol. 164, 851–870 (2011). https://doi.org/10.1530/EJE-10-1147
W.F. Young, The incidentally discovered adrenal mass. N. Engl. J. Med 356, 601–610 (2007). https://doi.org/10.1056/nejmcp065470
M. Fassnacht, W. Arlt, I. Bancos, H. Dralle, J. Newell-Price, A. Sahdev et al. Management of adrenal incidentalomas: European Society of Endocrinology Clinical Practice Guideline in collaboration with the European Network for the Study of Adrenal Tumors. Eur. J. Endocrinol. 175, G1–G34 (2016). https://doi.org/10.1530/EJE-16-0467
M. Araujo-Castro, M. Iturregui Guevara, M. Calatayud Gutiérrez, P. Parra Ramírez, P. Gracia Gimeno, F.A. Hanzu et al. Practical guide on the initial evaluation, follow-up, and treatment of adrenal incidentalomas Adrenal Diseases Group of the Spanish Society of Endocrinology and Nutrition. Endocrinol. Diabetes y. Nutr. 67, 408–419 (2020). https://doi.org/10.1016/j.endinu.2020.03.002
J.H. Kim, Min Joo Kim, J.H. Lee, J.W. Yoon, C.S. Shin, M.J. Kim et al. Nonfunctioning adrenal incidentalomas are not clinically silent: a longitudinal cohort study. Endocr. Pr. 26, 1406–1415 (2020). https://doi.org/10.4158/EP-2020-0182
F. Athanasouli, G. Georgiopoulos, N. Asonitis, F. Petychaki, A. Savelli, E. Panou et al. Nonfunctional adrenal adenomas and impaired glucose metabolism: a systematic review and meta-analysis. Endocrine 74, 50–60 (2021). https://doi.org/10.1007/s12020-021-02741-x
R. Emral, B.İ. Aydoğan, A.D. Köse, Ö. Demir, D. Çorapçıoğlu, Could a nonfunctional adrenal incidentaloma be a risk factor for increased carotid intima-media thickness and metabolic syndrome. Endocrinol. Diabetes y. Nutr. 66, 402–409 (2019). https://doi.org/10.1016/j.endinu.2019.01.007
M. Araujo-Castro Cardiometabolic profile and urinary metabolomic alterations in non-functioning adrenal incidentalomas: a review. Clin Endocrinol (Oxf) (2022). https://doi.org/10.1111/cen.14745
M. Araujo-Castro, H.F. Escobar-Morreale, P. Valderrábano, A Proposal for Nomenclature Revision of Non-functioning Adrenal Incidentalomas as Adrenal Lesions of Undetermined Secretion of Adrenal Steroids (ALUSAS). Endocr Pract (2022). https://doi.org/10.1016/J.EPRAC.2022.06.007
M. Araujo-Castro, P. Parra Ramírez, C. Robles Lázaro, R. García Centeno, P. Gracia Gimeno, M.T. Fernández-Ladreda, et al. Predictors of tumour growth and autonomous cortisol secretion development during follow-up in non-functioning adrenal incidentalomas. J Clin Med 10, (2021). https://doi.org/10.3390/jcm10235509
M. Araujo-Castro, P.P. Ramírez, C.R. Lázaro, R.G. Centeno, P.G. Gimeno, M.T. Fernández-Ladreda et al. Accuracy of the dexamethasone suppression test for the prediction of autonomous cortisol secretion-related comorbidities in adrenal incidentalomas. Horm 2021 20, 1–10 (2021). https://doi.org/10.1007/S42000-021-00308-Z
N. Genere, R.J. Kaur, S. Athimulam, M.A. Thomas, T. Nippoldt, M. Van Norman et al. Interpretation of abnormal dexamethasone suppression test is enhanced with use of synchronous free cortisol assessment. J. Clin. Endocrinol. Metab. 107, E1221–E1230 (2022). https://doi.org/10.1210/CLINEM/DGAB724
M. Araujo-Castro, E. Pascual-Corrales, A. Acitores Cancela, S. García Duque, L. Ley Urzaiz, V. Rodríguez Berrocal, Status and clinical and radiological predictive factors of presurgical anterior pituitary function in pituitary adenomas. Study 232 patients Endocr. 70, 584–592 (2020). https://doi.org/10.1007/s12020-020-02455-6
P.A. Harris, R. Taylor, R. Thielke, J. Payne, N. Gonzalez, J.G. Conde, Research electronic data capture (REDCap)-A metadata-driven methodology and workflow process for providing translational research informatics support. J. Biomed. Inf. 42, 377–381 (2009). https://doi.org/10.1016/j.jbi.2008.08.010
P.A. Harris, R. Taylor, B.L. Minor, V. Elliott, M. Fernandez, O’Neal L., et al. The REDCap consortium: Building an international community of software platform partners. J Biomed Inform 95, (2019). https://doi.org/10.1016/j.jbi.2019.103208
M. Araujo-Castro, C. Robles Lázaro, P. Parra Ramírez, R. García Centeno, P. Gracia Gimeno, M.T. Fernández-Ladreda et al. Maximum adenoma diameter, regardless of uni- or bilaterality, is a risk factor for autonomous cortisol secretion in adrenal incidentalomas. J. Endocrinol. Invest 44, 2349–2357 (2021). https://doi.org/10.1007/s40618-021-01539-y
O. Akkus, G. Akkus, O. Kaypakli, F.K. Ozturk, E. Gurkan, O. Bekler et al. Increased rates of coronary artery calcium score in patients with non - functioning adrenal incidentaloma. Endocr., Metab. Immune Disord. - Drug Targets 21, 1319–1325 (2020). https://doi.org/10.2174/1871530320666200910110337
M.P. de Paula, A.B. Moraes, M. de Souza, G.C. das, E.M.R. Cavalari, R.C. Campbell, G. Fernandes, S. da et al. Cortisol level after dexamethasone suppression test in patients with non-functioning adrenal incidentaloma is positively associated with the duration of reactive hyperemia response on microvascular bed. J. Endocrinol. Invest 44, 609–619 (2021). https://doi.org/10.1007/s40618-020-01360-z
V. Morelli, C. Aresta, A. Gaudio, C. Eller-Vainicher, V.V. Zhukouskaya, D. Merlotti et al. Prediction of hypertension, diabetes and fractures in eucortisolemic women by measuring parameters of cortisol milieu. Endocrine 68, 411–419 (2020). https://doi.org/10.1007/S12020-020-02212-9
M. Parasiliti-Caprino, C. Lopez, M. Bollati, F. Bioletto, C. Sola, M.C. Di Carlo, et al. A retrospective study on the association between urine metanephrines and cardiometabolic risk in patients with nonfunctioning adrenal incidentaloma. Sci Rep 12, (2002). https://doi.org/10.1038/S41598-022-19321-2
M. Araujo-Castro, G. Casals, F.A. Hanzu, E. Pascual-Corrales, A.M. García Cano, V.F. Lanza, et al. Characterisation of the urinary steroid profile of patients with nonfunctioning adrenal incidentalomas: A matched controlled cross-sectional study. Clin Endocrinol (Oxf) 2022. https://doi.org/10.1111/CEN.14811
I. Karahan, S. Durmaz Ceylan, A. Gungunes, A. Cifci, F. Eker, U. Kisa, Non-functioning adrenal incidentalomas may increase toxic metabolites. Wien. Klin. Wochenschr. 134, 125–129 (2022). https://doi.org/10.1007/S00508-021-01909-9
M. Peppa, C. Koliaki, S.A. Raptis, Adrenal incidentalomas and cardiometabolic morbidity: an emerging association with serious clinical implications. J. Intern Med 268, 555–566 (2010). https://doi.org/10.1111/j.1365-2796.2010.02291.x
P. Falcetta, F. Orsolini, E. Benelli, P. Agretti, P. Vitti, C. Di Cosmo et al. Clinical features, risk of mass enlargement, and development of endocrine hyperfunction in patients with adrenal incidentalomas: a long-term follow-up study. Endocrine 71, 178–188 (2020). https://doi.org/10.1007/s12020-020-02476-1
M. Araujo‐Castro, G. Casals, F.A. Hanzu, E. Pascual‐Corrales, A.M. García Cano, V.F. Lanza, et al. Characterisation of the urinary steroid profile of patients with nonfunctioning adrenal incidentalomas: A matched controlled cross-sectional study. Clin Endocrinol (Oxf) (2022). https://doi.org/10.1111/CEN.14811
N. Muangnoo, W. Manosroi, N. Leelathanapipat, T. Meejun, P. Chowchaiyaporn, P. Teetipsatit Predictive Factors of Functioning Adrenal Incidentaloma: A 15-Year Retrospective Study. Med 2022 58. https://doi.org/10.3390/MEDICINA58050597/S1
L. Barzon, C. Scaroni, N. Sonino, F. Fallo, A. Paoletta, M. Boscaro Risk Factors and Long-Term Follow-Up of Adrenal Incidentalomas 1. J Clin Endocrinol Metab (1999). https://doi.org/10.1210/jcem.84.2.5444
D.A. Vassiliadi, G. Ntali, E. Vicha, S. Tsagarakis, High prevalence of subclinical hypercortisolism in patients with bilateral adrenal incidentalomas: a challenge to management. Clin. Endocrinol. (Oxf.) 74, 438–444 (2011). https://doi.org/10.1111/j.1365-2265.2010.03963.x
E. Vassilatou, A. Vryonidou, D. Ioannidis, S.A. Paschou, M. Panagou, I. Tzavara, Bilateral adrenal incidentalomas differ from unilateral adrenal incidentalomas in subclinical cortisol hypersecretion but not in potential clinical implications. Eur. J. Endocrinol. 171, 37–45 (2014). https://doi.org/10.1530/EJE-13-0848
H. Olsen, E. Nordenström, A. Bergenfelz, U. Nyman, S. Valdemarsson, E. Palmqvist, Subclinical hypercortisolism and CT appearance in adrenal incidentalomas: a multicenter study from Southern Sweden. Endocrine 42, 164–173 (2012). https://doi.org/10.1007/s12020-012-9622-2
Funding
SENDIMAD: BECA SENDIMAD de Ayuda a la Investigación en Endocrinología, Nutrición y Diabetes 2019. IRYCIS (Convocatoria intramural de ayudas aproyectos de investigación deinvestigadores noveles, investigadoresclínicos asociados y/o grupos emergentesdel Hospital Universitario Ramón y Cajal2019).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Ethics
The study was conducted according to the guidelines of the Declaration of Helsinki and approved by the Ethics Committee of the Hospital Universitario Ramón y Cajal. Madrid. Spain (approval date: 23 September 2019, acta CEIm 10/19, approval number: 3702)
Informed consent
Patient consent was waived due to the retrospective nature of the study. Only for patients who continued follow-up or prospectively included the informed consent was requested.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Araujo-Castro, M., Parra Ramírez, P., Martín Rojas-Marcos, P. et al. Nonfunctioning adrenal incidentalomas with cortisol post-dexamethasone suppression test >0.9 µg/dL have a higher prevalence of cardiovascular disease than those with values ≤0.9 µg/dL. Endocrine 79, 384–391 (2023). https://doi.org/10.1007/s12020-022-03228-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12020-022-03228-z