Abstract
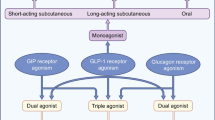
For decades, extensive research has aimed to clarify the role of pancreas and gut-derived peptide hormones in the regulation of glucose homeostasis and feeding behavior. Among these are the beta-cell hormone amylin and the intestinal L cell hormone glucagon-like peptide-1 (GLP-1). They exhibit distinct and yet several similar physiological actions including suppression of food intake, postprandial glucagon secretion, and gastric emptying—altogether lowering plasma glucose and body weight. These actions have been clinically exploited by the development of amylin and GLP-1 hormone analogs now used for treatment of diabetes and obesity. This review will outline the physiology and pharmacological potential of amylin and GLP-1, respectively, and focus on innovative peptide drug development leading to drugs acting on two or more distinct receptors, such as an amylin and GLP-1 peptide hybrid, potentially producing a more effective treatment strategy to combat the rapidly increasing global obesity.

Similar content being viewed by others
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
World Health Organization. Obesity and overweight. 2015. http://www.who.int/mediacentre/factsheets/fs311/en/.
Madsbad S, Dirksen C, Holst JJ. Mechanisms of changes in glucose metabolism and bodyweight after bariatric surgery. Lancet Diabetes Endocrinol Elsevier Ltd. 2014;2:152–64.
Dirksen C, Jørgensen NB, Bojsen-Møller KN, et al. Mechanisms of improved glycaemic control after Roux-en-Y gastric bypass. Diabetologia. 2012;55:1890–901.
Miras AD, le Roux CW. Metabolic surgery: shifting the focus from glycaemia and weight to end-organ health. Lancet Diabetes Endocrinol Elsevier Ltd. 2014;2:141–51.
Secher A, Jelsing J, Barquero AF, et al. The arcuate nucleus mediates GLP-1 receptor agonist liraglutide-dependent weight loss. J Clin Invest. 2014;124:4223–6. This study provides novel findings indicating that the GLP-1R found in key neuronal pathways of the brain that regulate energy balance likely mediates liraglutide-induced weight loss.
Hollander P, Levy P, Fineman MS, et al. Pramlintide as an adjunct to insulin therapy improves long-term glycemic and weight control in patients with type 2 diabetes: a 1-year randomized controlled trial. Diabetes Care. 2003;26:784–90.
Chapman I, Parker B, Doran S, et al. Effect of pramlintide on satiety and food intake in obese subjects and subjects with type 2 diabetes. Diabetologia. 2005;48:838–48.
Astrup A, Rössner S, Van Gaal L, et al. Effects of liraglutide in the treatment of obesity: a randomised, double-blind, placebo-controlled study. Lancet Elsevier Ltd. 2009;374:1606–16.
Sadry SA, Drucker DJ. Emerging combinatorial hormone therapies for the treatment of obesity and T2DM. Nat Rev Endocrinol Nature Publishing Group. 2013;9:425–33.
Schmitz O, Brock B, Rungby J. Amylin agonists: a novel approach in the treatment of diabetes. Diabetes. 2004;53:233–8.
Bello NT, Kemm MH, Ofeldt EM, et al. Dose combinations of exendin-4 and salmon calcitonin produce additive and synergistic reductions in food intake in nonhuman primates. Am J Physiol Regul Integr Comp Physiol. 2010;299:945–52.
Rodgers RJ, Tschop MH, Wilding JPH. Anti-obesity drugs: past, present and future. Dis Model Mech. 2012;5:621–6.
Fosgerau K, Hoffmann T. Peptide therapeutics: current status and future directions. Drug Discov Today Elsevier Ltd. 2015;20:122–8. This paper gives a fine overview of the current status and potentials ahead in development of peptide pharmaceuticals.
Trevaskis JL, Mack CM, Sun C, et al. Improved glucose control and reduced body weight in rodents with dual mechanism of action peptide hybrids. PLoS One. 2013;8:1–12.
Riddle MC, Drucker DJ. Emerging therapies mimicking the effects of amylin and glucagon-like peptide 1. Diabetes Care. 2006;29:435–49.
Lutz TA. Amylinergic control of food intake. Physiol Behav. 2006;89:465–71.
Juhl CB, Pørksen N, Sturis J, et al. High-frequency oscillations in circulating amylin concentrations in healthy humans. Am J Physiol Endocrinol Metab. 2000;278:484–90.
Lutz TA. The interaction of amylin with other hormones in the control of eating. Diabetes, Obes Metab. 2013;15:99–111.
Qi T, Ly K, Poyner DR, et al. Structure-function analysis of amino acid 74 of human RAMP1 and RAMP3 and its role in peptide interactions with adrenomedullin and calcitonin gene-related peptide receptors. Peptides Elsevier Inc. 2011;32:1060–7.
Just R, Simms J, Furness SGB, Christopoulos A SA. Understanding Amylin Receptors. Springer; 2010
Roth JD. Amylin and the regulation of appetite and adiposity: recent advances in receptor signaling, neurobiology and pharmacology. Curr Opin Endocrinol Diabetes Obes. 2013;20:8–13.
Züger D, Forster K, Lutz TA, et al. Amylin and GLP-1 target different populations of area postrema neurons that are both modulated by nutrient stimuli. Physiol Behav Elsevier Inc. 2013;112–113:61–9.
Roth JD, Erickson MR, Chen S, et al. GLP-1R and amylin agonism in metabolic disease: complementary mechanisms. Br J Pharmacol. 2012;166:121–36.
Moon HS, Chamberland JP, Diakopoulos KN, et al. Leptin and amylin act in an additive manner to activate overlap** signaling pathways in peripheral tissues: in vitro and ex vivo studies in humans. Diabetes Care. 2011;34:132–8.
Moon HS, Chamberland JP, Mantzoros CS. Amylin and leptin activate overlap** signalling pathways in an additive manner in mouse GT1-7 hypothalamic, C 2C 12 muscle and AML12 liver cell lines. Diabetologia. 2012;55:215–25.
Vilsbøll T, Holst JJ. Incretins, insulin secretion and Type 2 diabetes mellitus. Diabetologia. 2004;47:357–66.
Sjölund K, Sandén G, Håkanson R. Endocrine cells in human intestine: an immunocytochemical study. Gastroent. 1983;85:1120–30.
Holst JJ. The physiology of glucagon-like peptide 1. Physiol Rev. 2007;87:1409–39.
Vilsbøll T, Krarup T, Madsbad S, et al. Both GLP-1 and GIP are insulinotropic at basal and postprandial glucose levels and contribute nearly equally to the incretin effect of a meal in healthy subjects. Regul Pept. 2003;114:115–21.
Madsbad S. The role of glucagon-like peptide-1 impairment in obesity and potential therapeutic implications. Diabetes Obes Metab. 2013;1:1–13.
Pyke C, Heller RS, Kirk RK, et al. GLP-1 receptor localization in monkey and human tissue: novel distribution revealed with extensively validated monoclonal antibody. Endocrinology. 2014;155:1280–90.
Sandhu H, Wiesenthal SR, MacDonald PE, et al. Glucagon-like peptide 1 increases insulin sensitivity in depancreatized dogs. Diabetes. 1999;48:1045–53.
Bullock P, Scott R. Tissue distribution of messenger ribonucleic acid encoding the rat glucagon-like peptide-1 receptor. Endocrinology. 2015;137:31–3.
Egan M, Bernier M. Glucagon-like peptide-1 (7–34) amide (GLP-1) enhances insulin-stimulated glucose metabolism in 3T3-L1 adipocytes: one of several potential extrapancreatic sites of GLP-1 action. Endocrinology. 2007;135:2070–5.
Mulvihill EE, Drucker DJ. Pharmacology, physiology, and mechanisms of action of dipeptidyl peptidase-4 inhibitors. Endocr Rev. 2014;35:992–1019.
Holst JJ, Deacon CF. Glucagon-like peptide-1 mediates the therapeutic actions of DPP-IV inhibitors. Diabetologia. 2005;48:612–5.
Jones MC. Therapies for diabetes: pramlintide and exenatide. Am Fam Physician. 2007;75:1831–5.
Hollander P, Levy P, Fineman MS, et al. Pramlintide as an adjunct to insulin therapy improves long-term glycemic and weight control in patients with type 2 diabetes: a 1-year randomized controlled trial. Diabetes Care. 2003;26:784–90.
Hollander P, Ratner R, Fineman M, et al. Addition of pramlintide to insulin therapy lowers HbA1c in conjunction with weight loss in patients with type 2 diabetes approaching glycaemic targets. Diabetes, Obes Metab. 2003;5:408–14.
Hollander P, Maggs DG, Ruggles JA, et al. Effect of pramlintide on weight in overweight and obese insulin-treated type 2 diabetes patients. Obes Res. 2004;12:661–8.
Smith S, Aronne L, Weyer C. Sustained weight loss following 12-month pramlintide treatment as an adjunct to lifestyle intervention in obesity. Biomed Res. 2008;31:1816–23.
Meier JJ, Nauck MA. Incretin-based therapies: where will we be 50 years from now? Diabetologia. 2015;58:1745–50.
Lund A, Knop FK, Vilsboll T. Glucagon-like peptide-1 receptor agonists for the treatment of type 2 diabetes: differences and similarities. Eur J Intern Med. 2014;25:407–14.
Garber AJ. Long-acting glucagon-like peptide 1 receptor agonists: a review of their efficacy and tolerability. Diabetes Care. 2011;34:279–84.
Vilsboll T, Christensen M, Junker A, et al. Effects of glucagon-like peptide-1 receptor agonists on weight loss: systematic review and meta-analyses of randomised controlled trials. BMJ. 2012;344:1–11.
McGill J. Insights from the liraglutide clinical development program-the liraglutide effect and action in diabetes (LEAD) studies. Postgr Med. 2013;121(3):16–25.
Sethi BK, Viswanathan V, Kumar A, et al. Liraglutide in clinical practice: insights from LEAD programme. J Assoc Physicians India. 2010;58:18–22.
Astrup A, Carraro R, Harper A, et al. Safety, tolerability and sustained weight loss over 2 years with the once-daily human GLP-1 analog, liraglutide. Int J Obes (Lond). 2012;36(6):843–54.
Davies MJ, Bergenstal R, Bode B, et al. Efficacy of liraglutide for weight loss among patients with type 2 diabetes. Jama. 2015;314(7):687–99.
Pi-Sunyer X, Astrup A, Fujioka K, et al. A randomized, controlled trial of 3.0 mg of liraglutide in weight management. N Engl J Med. 2015;373:11–22. This study provides important clinical data on liraglutide 3.0 mg recently approved for treatment of obesity.
Chalmer T, Almdal TP, Vilsbøll T, et al. Adverse drug reactions associated with the use of liraglutide in patients with type 2 diabetes—focus on pancreatitis and pancreas cancer. Expert Opin Drug Saf. 2015;14(1):1–10.
DeFronzo R, Bergenstal R, Bode B, et al. Effect of liraglutide 3.0 mg cessation on efficacy and safety/tolerability after 56 weeks’ treatment in obese/overweight adults with type 2 diabetes: SCALE diabetes. Diabetologia. 2014;57(Suppl1):S38–9.
http://www.fda.gov/NewsEvents/Newsroom/PressAnnouncements/ucm427913.htm U.S. Food and Drug Administration. FDA approves weight-management drug Saxenda. 2014.
European Medicines Agency, Saxenda recommended for approval in weight management in adults. 2015 http://www.ema.europa.eu/ema/index.jsp?curl=pages/news_and_events/news/2015/01/news_detail_002255.jsp&mid=WC0b01ac058004d5c1.
Hayes MR, Mietlicki-Baase EG, Kanoski SE, et al. Incretins and amylin: neuroendocrine communication between the gut, pancreas, and brain in control of food intake and blood glucose. Annu Rev Nutr. 2014;34:237–60.
Dawson PE, Kent SBH. Synthesis of native proteins by chemical ligation. Annu Rev Biochem. 2000;69:923–60.
Pocai A, Carrington PE, Adams JR, et al. Glucagon-like peptide 1/glucagon receptor agonism reverses obesity in mice. Diabetes. 2009;58:2258–66.
Claus TH, Pan CQ, Buxton JM, et al. Dual-acting peptide with prolonged glucagon-like peptide-1 receptor agonist and glucagon receptor antagonist activity for the treatment of type 2 diabetes. J Endocrinol. 2007;192:371–80.
Fosgerau K, Jessen L, Lind TJ, et al. The novel GLP-1-gastrin dual agonist, ZP3022, increases β-cell mass and prevents diabetes in db/db mice. Diabetes, Obes Metab. 2013;15:62–71.
Just R. The novel GLP-1-GLP-2 dual agonist ZP-GG-72 increases intestinal growth and improves insulin sensitivity in DIO mice. Diabetes. 2014;63:A1–A102.
Finan B, Ma T, Ottaway N, et al. Unimolecular dual incretins maximize metabolic benefits in rodents, monkeys, and humans. Sci Transl Med. 2013;5:209ra151.
Pocai A. Unraveling oxyntomodulin, GLP1’s enigmatic brother. J Endocrinol. 2012;215:335–46.
Witkamp RF. Current and future drug targets in weight management. Pharm Res. 2011;28:1792–818.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of Interest
T. Jorsal declares that she has no conflict of interest.
J. Rungby has received personal honoraria for consulting, lectures, and/or for advisory board participation within the last 36 months from AstraZeneca, Boehringer Ingelheim Pharmaceuticals, Janssen-Cilag, Merck Sharp & Dohme, Novo Nordisk, and Sanofi-Aventis and has received unrestricted research grants from Novo Nordisk and Merck.
F. K. Knop has received personal honoraria for consulting, lectures, and/or for advisory board participation within the last 36 months from AstraZeneca, Boehringer-Ingelheim Pharmaceuticals, Bristol-Myers Squibb, Eli Lilly, Gilead Sciences, Merck Sharp & Dohme, Novo Nordisk, Sanofi-Aventis, Janssen, and Zealand Pharma and has received unrestricted research grants from AstraZeneca, the Novo Nordisk Foundation, and Sanofi-Aventis.
T. Vilsbøll has received personal honoraria for consulting, lectures and/or for advisory board participation within the last 36 months from Amgen, AstraZeneca, Boehringer-Ingelheim Pharmaceuticals, Bristol-Myers Squibb, Eli Lilly, Janssen-Cilag, Merck Sharp & Dohme, Novo Nordisk, Sanofi-Aventis, and Zealand Pharma and has received unrestricted research grants from Novo Nordisk and the Novo Nordisk Foundation.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
This article is part of the Topical Collection on Pharmacologic Treatment of Type 2 Diabetes
Rights and permissions
About this article
Cite this article
Jorsal, T., Rungby, J., Knop, F.K. et al. GLP-1 and Amylin in the Treatment of Obesity. Curr Diab Rep 16, 1 (2016). https://doi.org/10.1007/s11892-015-0693-3
Published:
DOI: https://doi.org/10.1007/s11892-015-0693-3