Abstract
Purpose
Proximal humerus fractures in the pediatric population are a relatively uncommon injury, with the majority of injuries treated in a closed fashion due to the tremendous remodeling potential of the proximal humerus in the skeletally immature. Yet, in adolescent patients, open treatment is, at times, necessary due to unsatisfactory alignment following a closed reduction, loss of previously achieved closed reduction, and limited remodeling when close to skeletal maturity. The purpose of our study was to examine the open reduction of adolescent proximal humerus fractures.
Methods
A retrospective review of the outcomes of proximal humerus fractures in the adolescent population which were consecutively treated at our institution with open reduction was performed.
Results
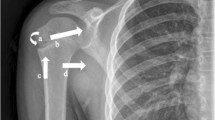
Ten children met the inclusion criteria, with a mean age of 14.3 years (±1.3) and a mean weight of 60.7 kg (±14.9) at the time of injury. There were seven Salter-Harris 2 fractures and three Salter-Harris 1 fractures. The largest mean angulation was 55.0° (±33.9) and the largest mean displacement was 87.0 % (±22.8). Intra-operatively, impediments to closed reduction within the fracture site which were found included: periosteum (90.0 %), biceps tendon (90.0 %), deltoid muscle (70.0 %), and comminuted bone (10.0 %). K-wire fixation was most commonly used (70.0 %), followed by flexible nails (20.0 %) and cannulated screws (10.0 %) for fixation. All patients achieved radiographic union at a mean of 4.0 weeks (±0.7), had non-painful full shoulder range of motion and rotator cuff strength at final follow-up (mean 7.7 ± 4.6 months), and returned to pre-injury sporting activities.
Conclusions
The operative treatment of proximal humerus fracture, particularly in adolescents with severe displacement/angulation having failed closed methods of treatment, is increasingly considered to be an acceptable modality of treatment. In addition to the long head of the biceps, periosteum, deltoid muscle, and bone fragments in combination can prevent fracture reduction. Surgeon preference and skill should dictate implant choice, and the risk of physeal damage utilizing these implants in this age group is low.



Similar content being viewed by others
References
Rose SH, Melton LJ 3rd, Morrey BF, Ilstrup DM, Riggs BL (1982) Epidemiologic features of humeral fractures. Clin Orthop Relat Res 168:24–30
Neer CS 2nd, Horwitz BS (1965) Fractures of the proximal humeral epiphysial plate. Clin Orthop Relat Res 41:24–31
Peterson CA, Peterson HA (1972) Analysis of the incidence of injuries to the epiphyseal growth plate. J Trauma 12:275–281
Shrader MW (2007) Proximal humerus and humeral shaft fractures in children. Hand Clin 23:431–435
Dameron TB Jr, Reibel DB (1969) Fractures involving the proximal humeral epiphyseal plate. J Bone Joint Surg Am 51:289–297
Pritchett JW (1988) Growth and predictions of growth in the upper extremity. J Bone Joint Surg Am 70:520–525
Larsen CF, Kiaer T, Lindequist S (1990) Fractures of the proximal humerus in children. Nine-year follow-up of 64 unoperated on cases. Acta Orthop Scand 61:255–257
Tachdjian MO (1990) Fractures involving the proximal humeral physis. In: Tachdjian MO (ed) Pediatric orthopedics, 2nd edn. WB Saunders Company, Philadelphia, pp 3046–3052
Fernandez FF, Eberhardt O, Langendörfer M, Wirth T (2008) Treatment of severely displaced proximal humeral fractures in children with retrograde elastic stable intramedullary nailing. Injury 39:1453–1459
Dobbs MB, Luhmann SL, Gordon JE, Strecker WB, Schoenecker PL (2003) Severely displaced proximal humeral epiphyseal fractures. J Pediatr Orthop 23:208–215
Beringer DC, Weiner DS, Noble JS, Bell RH (1998) Severely displaced proximal humeral epiphyseal fractures: a follow-up study. J Pediatr Orthop 18:31–37
Burgos-Flores J, Gonzalez-Herranz P, Lopez-Mondejar JA, Ocete-Guzman JG, Amaya-Alarcón S (1993) Fractures of the proximal humeral epiphysis. Int Orthop 17:16–19
Bahrs C, Zipplies S, Ochs BG, Rether J, Oehm J, Eingartner C, Rolauffs B, Weise K (2009) Proximal humeral fractures in children and adolescents. J Pediatr Orthop 29:238–242
Schwendenwein E, Hajdu S, Gaebler C, Stengg K, Vécsei V (2004) Displaced fractures of the proximal humerus in children require open/closed reduction and internal fixation. Eur J Pediatr Surg 14:51–55
Pahlavan S, Baldwin KD, Pandya NK, Namdari S, Hosalkar H (2011) Proximal humerus fractures in the pediatric population: a systematic review. J Child Orthop 5:187–194
Kohler R, Trillaud JM (1983) Fracture and fracture separation of the proximal humerus in children: report of 136 cases. J Pediatr Orthop 3:326–332
Baxter MP, Wiley JJ (1986) Fractures of the proximal humeral epiphysis. Their influence on humeral growth. J Bone Joint Surg Br 68:570–573
Nilsson S, Svartholm F (1965) Fracture of the upper end of the humerus in children. A follow-up of 44 cases. Acta Chir Scand 130:433–439
Brenner JS; American Academy of Pediatrics Council on Sports Medicine and Fitness (2007) Overuse injuries, overtraining, and burnout in child and adolescent athletes. Pediatrics 119:1242–1245
Dameron TB Jr, Rockwood CA Jr (1984) Fractures and dislocations of the shoulder. In: Rockwood CA Jr, Wilkins KE, King RE (eds) Fractures in children, 1st edn. JB Lippincott, Philadelphia, pp 577–683
Siebler G, Kuner EH, Schmitt A (1984) Operative treatment of proximal humerus fractures in children and adolescents—indications, technic, late results. Unfallchirurgie 10:237–244
Di Gennaro GL, Spina M, Lampasi M, Libri R, Donzelli O (2008) Fractures of the proximal humerus in children. Chir Organi Mov 92:89–95
David S, Kuhn C, Ekkernkamp A (2006) Fracture of the proximal humerus in children and adolescents. The most overtreated fracture. Chirurg 77:827–834
Visser JD, Rietberg M (1980) Interposition of the tendon of the long head of biceps in fracture separation of the proximal humeral epiphysis. Neth J Surg 32:12–15
Rajan RA, Hawkins KJ, Metcalfe J, Konstantoulakis C, Jones S, Fernandes J (2008) Elastic stable intramedullary nailing for displaced proximal humeral fractures in older children. J Child Orthop 2:15–19
Carey TP, El-Hawary R, Black CA, Leitch KK (2005) The results of surgical treatment for displaced pediatric proximal humerus fractures. Presented at the Canadian Orthopaedic Research Society and Canadian Orthopaedic Association Annual Meeting, Montreal, Canada, 3–5 June 2005
Author information
Authors and Affiliations
Corresponding author
Additional information
Study was conducted at Rady Children’s Hospital.
About this article
Cite this article
Pandya, N.K., Behrends, D. & Hosalkar, H.S. Open reduction of proximal humerus fractures in the adolescent population. J Child Orthop 6, 111–118 (2012). https://doi.org/10.1007/s11832-012-0398-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11832-012-0398-y