Abstract
Purpose
Decreasing popularity of Roux-en-Y gastric bypass (RYGB) in bariatric-metabolic surgery may be due to higher perceived peri-operative complications. There are few studies on whether preoperative weight loss can reduce complications or reoperations following RYGB. We investigated this using a standardised operative technique.
Materials and Methods
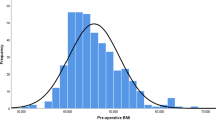
Retrospective single-centre study of RYGB from 2004 to 2019 using a prospective database. Preoperative behavioural management included intentional weight loss. Maximum preoperative weight, weight on the day of operation, and Obesity-Surgery Mortality Risk Score (OS-MRS) class were recorded. Short-term outcomes (post-operative stay, 30-day complication and reoperation rates) were analysed.
Results
In 2,067 RYGB patients (1,901 primary and 166 revisional), median preoperative total body weight loss (TWL) was 6.2% (IQR: 2.5–10.7%). The median age was 46 (interquartile range (IQR) 38–54) and 80.4% were female (n=1,661). For primary surgery, the median body mass index (BMI) was 47.6 kg/m2 (IQR: 43.1–53.3). Excluding the 100-procedure learning curve, the complication rate for primary cases was 4.4% and reoperation rate of 2.8% and one peri-operative mortality (0.06%). OS-MRS ≥2 (class B or C) predicted higher risk of complications (6.1%) compared to those with a score <2 (class A) (3.8%, p=0.021), but not reoperations. Five percent preoperative TWL did not decrease complications compared to <5% TWL. Patients with ≥10% TWL had greater baseline risk and had an increased risk of complications (6.6% vs 3.7%, p=0.017) and reoperations (4.5% vs 2.7%, p<0.001).
Conclusions
RYGB performed using a standardised technique has low overall risk. The influence of preoperative weight loss on outcomes was inconsistent.
Graphical abstract


Similar content being viewed by others
References
Sjöström L, Narbro K, Sjöström CD, et al. Effects of bariatric surgery on mortality in swedish obese subjects. N Engl J Med. 2007;357(8):741–52.
Sjöström L, Gummesson A, Sjöström CD, et al. Effects of bariatric surgery on cancer incidence in obese patients in Sweden (Swedish Obese Subjects Study): a prospective, controlled intervention trial. Lancet Oncol. 2009;10(7):653–62.
Sjöström L, Peltonen M, Jacobson P, et al. Bariatric surgery and long-term cardiovascular events. JAMA. 2012;307(1):56–65.
Wiggins T, Guidozzi N, Welbourn R, et al. Association of bariatric surgery with all-cause mortality and incidence of obesity-related disease at a population level: a systematic review and meta-analysis. PLoS Med. 2020;17(7):e1003206.
Wiggins T, Antonowicz SS, Markar SR. Cancer risk following bariatric surgery—systematic review and meta-analysis of national population-based cohort studies. Obes Surg. 2019;29(3):1031–9.
Schauer PR, Bhatt DL, Kirwan JP, et al. Bariatric surgery versus intensive medical therapy for diabetes — 5-year outcomes. N Engl J Med. 2017;376(7):641–51.
Mingrone G, Panunzi S, De Gaetano A, et al. Bariatric surgery versus conventional medical therapy for type 2 diabetes. N Engl J Med. 2012;366(17):1577–85.
Cummings DE, Rubino F. Metabolic surgery for the treatment of type 2 diabetes in obese individuals. Diabetologia. 2018;61(2):257–64.
Welbourn R, Hollyman M, Kinsman R, et al. Bariatric surgery worldwide: baseline demographic description and one-year outcomes from the Fourth IFSO Global Registry Report 2018. Obes Surg. 2019;29(3):782–95.
Ames GE, Maynard JR, Collazo-Clavell ML, et al. Rethinking patient and medical professional perspectives on bariatric surgery as a medically necessary treatment. Mayo Clin Proc. 2020;95(3):527–40.
Salminen P, Helmiö M, Ovaska J, et al. Effect of laparoscopic sleeve gastrectomy vs laparoscopic Roux-en-Y gastric bypass on weight loss at 5 years among patients with morbid obesity: the SLEEVEPASS randomized clinical trial. JAMA. 2018;319(3):241–54.
Peterli R, Wölnerhanssen BK, Peters T, et al. Effect of laparoscopic sleeve gastrectomy vs laparoscopic Roux-en-Y gastric bypass on weight loss in patients with morbid obesity: the SM-BOSS randomized clinical trial. JAMA. 2018;319(3):255–65.
Robert M, Espalieu P, Pelascini E, et al. Articles efficacy and safety of one anastomosis gastric bypass versus Roux-en-Y gastric bypass for obesity (YOMEGA): a multicentre , randomised , open-label , non-inferiority trial. Lancet. 2019;393(10178):1299–309.
Poelemeijer YQM, Liem RSL, Våge V, et al. Gastric bypass versus sleeve gastrectomy: patient selection and short-term outcome of 47,101 primary operations from the Swedish, Norwegian, and Dutch National Quality Registries. Ann Surg. 2020;272(2):326–33.
Kumar SB, Hamilton BC, Wood SG, et al. Is laparoscopic sleeve gastrectomy safer than laparoscopic gastric bypass? a comparison of 30-day complications using the MBSAQIP data registry. Surg Obes Relat Dis. 2018;14(3):264–9.
El Chaar M, Stoltzfus J, Gersin K, et al. A novel risk prediction model for 30-day severe adverse events and readmissions following bariatric surgery based on the MBSAQIP database. Surg Obes Relat Dis. 2019;15(7):1138–45.
Ladak F, Dang JT, Switzer NJ, et al. Rates of reoperation and nonoperative intervention within 30 days of bariatric surgery. Surg Obes Relat Dis. 2019;15(3):431–40.
DeMaria EJ, Portenier D, Wolfe L. Obesity surgery mortality risk score: proposal for a clinically useful score to predict mortality risk in patients undergoing gastric bypass. Surg Obes Relat Dis. 2007;3(2):134–40.
DeMaria EJ, Murr M, Byrne TK, et al. Validation of the obesity surgery mortality risk score in a multicenter study proves it stratifies mortality risk in patients undergoing gastric bypass for morbid obesity. Ann Surg. 2007;246(4):578–82. discussion 583-4
NICE. Guidance for Clinical Comissioning Groups (CCGs): Clinical guidance: revision surgery for complex obesity. Available from: https://www.england.nhs.uk/wp-content/uploads/2016/05/appndx-8-revision-surgery-ccg-guid.pdf [Last accessed 28/09/2020].
Welbourn R, Dixon J, Barth JH, et al. NICE-Accredited commissioning guidance for weight assessment and management clinics: a model for a specialist multidisciplinary team approach for people with severe obesity. Obes Surg. 2016;26(3):649–59.
Pournaras DJ, Jafferbhoy S, Titcomb DR, et al. Three hundred laparoscopic Roux-en-Y gastric bypasses: Managing the learning curve in higher risk patients. Obes Surg. 2010;20(3):290–4.
Management of adults with diabetes undergoing surgery and elective procedures: improving standards. Diabetes UK. Available from: https://www.diabetes.org.uk/professionals/position-statements-reports/specialist-care-for-children-and-adults-and-complications/management-of-adults-with-diabetes-undergoing-surgery-and-elective-procedures-improving-standards [Last accessed 28/09/2020].
Kim JJ. Evidence base for optimal preoperative preparation for bariatric surgery: does mandatory weight loss make a difference? Curr Obes Rep. 2017;6(3):238–45.
Higa KD, Boone KB, Ho T, et al. Laparoscopic Roux-en-Y gastric bypass for morbid obesity: technique and preliminary results of our first 400 patients. Arch Surg. 2000;135(9):1029–33. discussion 1033-4
MacLean LD, Rhode BM, Nohr CW. Long- or short-limb gastric bypass? J Gastrointest Surg. 2001;5(5):525–30.
Mahawar KK, Kumar P, Parmar C, et al. Small bowel limb lengths and Roux-en-Y gastric bypass: a systematic review. Obes Surg. 2016;26(3):660–71.
Gan J, Wang Y, Zhou X. Whether a short or long alimentary limb influences weight loss in gastric bypass: a systematic review and meta-analysis. Obes Surg. 2018;28(11):3701–10.
Dindo D, Demartines N, Clavien PA. Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg. 2004;240(2):205–13.
Coulman KD, Hopkins J, Brookes ST, et al. A core outcome set for the benefits and adverse events of bariatric and metabolic surgery: the BARIACT Project. PLoS Med. 2016;13(11).
Vidarsson B, Sundbom M, Edholm D. Incidence and treatment of leak at the gastrojejunostomy in Roux-en-Y gastric bypass: a cohort study of 40,844 patients. Surg Obes Relat Dis. 2019;15(7):1075–9.
Tan SYT, Loi PL, Lim CH, et al. Preoperative weight loss via very low caloric diet (VLCD) and its effect on outcomes after bariatric surgery. Obes Surg. 2020;30(6):2099–107.
Anderin C, Gustafsson UO, Heijbel N, et al. Weight loss before bariatric surgery and postoperative complications: data from the Scandinavian Obesity Registry (SOReg). Ann Surg. 2015;261(5):909–13.
Sun Y, Liu B, Smith JK, et al. Association of preoperative body weight and weight loss with risk of death after bariatric surgery. JAMA Netw Open. 2020;3(5):3–11.
Tewksbury C, Crowley N, Parrott JM, et al. Weight loss prior to bariatric surgery and 30-day mortality, readmission, reoperation, and intervention: an MBSAQIP analysis of 349,016 cases. Obes Surg. 2019;29(11):3622–8.
Benotti PN, Still CD, Wood GC, et al. Preoperative weight loss before bariatric surgery. Arch Surg. 2009;144(12):1150–5.
Pournaras DJ, Nygren J, Hagström-Toft E, et al. Improved glucose metabolism after gastric bypass: evolution of the paradigm. Surg Obes Relat Dis. 2016;12(8):1457–65.
Wennerlund J, Gunnarsson U, Strigård K, et al. Acid-related complications after laparoscopic Roux-en-Y gastric bypass: risk factors and impact of proton pump inhibitors. Surg Obes Relat Dis. 2020;16(5):620–5.
Benotti P, Wood GC, Winegar DA, et al. Risk factors associated with mortality after Roux-en-Y gastric bypass surgery. Ann Surg. 2014;259(1):123–30.
Ali MR, Tichansky DS, Kothari SN, et al. Validation that a 1-year fellowship in minimally invasive and bariatric surgery can eliminate the learning curve for laparoscopic gastric bypass. Surg Endosc. 2010;24(1):138–44.
Lorente L, Ramón JM, Vidal P, et al. Obesity surgery mortality risk score for the prediction of complications after laparoscopic bariatric surgery. Cir Esp. 2014;92(5):316–23.
Stenberg E, Szabo E, Ågren G, et al. Early complications after laparoscopic gastric bypass surgery: results from the scandinavian obesity surgery registry. Ann Surg. 2014;260(6):1040–7.
Coblijn UK, Lagarde SM, de Raaff CAL, et al. Evaluation of the obesity surgery mortality risk score for the prediction of postoperative complications after primary and revisional laparoscopic Roux-en-Y gastric bypass. Surg Obes Relat Dis. 2016;12(8):1504–12.
García-García ML, Martín-Lorenzo JG, Lirón-Ruiz R, et al. Failure of the Obesity Surgery Mortality Risk Score (OS-MRS) to predict postoperative complications after bariatric surgery. a single-center series and systematic review. Obes Surg. 2017;27(6):1423–9.
Gero D, Raptis DA, Vleeschouwers W, et al. Defining global benchmarks in bariatric surgery: a retrospective multicenter analysis of minimally invasive Roux-en-Y gastric bypass and sleeve gastrectomy. Ann Surg. 2019;270(5):859–67.
Zolin SJ, Petro CC, Prabhu AS, et al. Registry-based randomized controlled trials: a new paradigm for surgical research. J Surg Res. 2020;255:428–35.
Markar SR, Wiggins T, Ni M, et al. Assessment of the quality of surgery within randomised controlled trials for the treatment of gastro-oesophageal cancer: a systematic review. Lancet Oncol. 2015;16(1):e23–31.
Leonard-Murali S, Nasser H, Ivanics T, et al. Perioperative outcomes of Roux-en-Y gastric bypass and sleeve gastrectomy in patients with diabetes mellitus: an analysis of the Metabolic and Bariatric Surgery Accreditation and Quality Improvement Program (MBSAQIP) database. Obes Surg. 2020;30(1):111–8.
Welbourn R, Pournaras D. Comment on: 30-day outcomes of sleeve gastrectomy (SG) versus Roux-en-Y gastric bypass (GB): first report based on MBSAQIP database. Surg Obes Relat Dis. 2018;14(5):551–3.
Rogers CA, Reeves BC, Byrne J, et al. Adaptation of the By-Band randomized clinical trial to By-Band-Sleeve to include a new intervention and maintain relevance of the study to practice. Br J Surg. 2017;104(9):1207–14.
Hedberg S, Olbers T, Peltonen M, et al. BEST: Bypass equipoise sleeve trial; rationale and design of a randomized, registry-based, multicenter trial comparing Roux-en-Y gastric bypass with sleeve gastrectomy. Contemp Clin Trials. 2019;84:105809.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical Approval Statement
For this type of study, formal consent is not required.
Informed Consent Statement
Informed consent does not apply.
Conflict of Interest
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Key Points
1. Roux-en-Y gastric bypass is a safe procedure with low complication (4.4%) and reoperation rates (2.8%) once the procedure is well established.
2. Achieving 5% preoperative total weight loss was not protective for complications.
3. Greater preoperative weight loss (10% or more) was associated with increased complication and reoperation rates but this was likely due to increased baseline risk for these patients.
4. OS-MRS above 2 was associated with increased risk of complications.
Rights and permissions
About this article
Cite this article
Wiggins, T., Pournaras, D.J., Priestman, E. et al. Effect of Preoperative Weight Loss and Baseline Comorbidity on Short-Term Complications and Reoperations After Laparoscopic Roux-en-Y Gastric Bypass in 2,067 Patients. OBES SURG 31, 2444–2452 (2021). https://doi.org/10.1007/s11695-021-05331-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-021-05331-y