Abstract
Background
The effect of weight loss by bariatric surgery on gonadal hormones in morbidly obese males is not entirely known. The main objective of the study was to analyze gonadal hormonal changes after weight loss.
Methods
An observational study was conducted before and after 12 months of weight loss at a clinical research center. Thirty-three men [age 40.5 ± 9.9, body mass index (BMI) 50.3 ± 6.1 kg/m2] undergoing bariatric surgery were included. The main outcome measures were as follows: changes in total (TT) and free testosterone (FT), estradiol (E2), sex hormone binding globulin (SHBG), luteinizing hormone (LH), follicle-stimulating hormone (FSH), anti-Müllerian hormone (AMH), inhibin B, and prolactin (PRL).
Results
Baseline prevalence of hypogonadism (defined by TT < 300 ng/dl or FT < 65 pg/ml) was 78.8 and 51.5 %, respectively. Hypogonadal patients were older and showed inhibin B and AMH significantly lower than those with normal TT. BMI correlated negatively with TT, LH, and SHBG. Regression analyses showed a significant and independent association of hypogonadism with age (OR = 1.2, p = 0.01), BMI (OR = 1.3, p = 0.03), and AMH (OR = 0.4, p = 0.03) after adjustments. After 1 year, percentage of weight loss (%WL) was 18.8 ± 5.2 %, and there was a significant increase of TT, FT, SHBG, and FSH and a decrease of E2 and PRL. Prevalence of persistent hypogonadism after surgery was 6 % (low TT) and 15 % (low FT). %WL was significantly associated with percent changes in SHBG (r = −0.4, p = 0.04), inhibin B (r = −0.4, p = 0.03), and AMH (r = −0.4, p = 0.01). Age and %WL were the only significant and independent parameters associated with %TT change.
Conclusions
Obesity-associated hypogonadism is very prevalent in males with morbid obesity and is mostly reversed after sustained weight loss by bariatric surgery.

Similar content being viewed by others
References
Narayan KM, Boyle JP, Thompson TJ, et al. Effect of BMI on lifetime risk for diabetes in the U.S. Diabetes Care. 2007;30:1562–6.
Serra A, Romero R, Lopez D, et al. Renal injury in the extremely obese patients with normal renal function. Kidney Int. 2008;73:947–55.
Buchwald H, Estok R, Fahrbach K, et al. Weight and type 2 diabetes after bariatric surgery: systematic review and meta-analysis. Am J Med. 2009;122:248–56.
Sjöström L, Lindroos AK, Peltonen M, et al. Swedish Obese Subjects Study Scientific Group lifestyle, diabetes, and cardiovascular risk factors 10 years after bariatric surgery. N Engl J Med. 2004;351:2683–93.
Navarro-Díaz M, Serra A, Romero R, et al. Effect of drastic weight loss after bariatric surgery on renal parameters in extremely obese patients: long-term follow-up. J Am Soc Nephrol. 2006;17:S213–7.
Serra A, Granada ML, Romero R, et al. The effect of bariatric surgery on adipocytokines, renal parameters and other cardiovascular risk factors in severe and very severe obesity: 1-year follow-up. Clin Nutr. 2006;25:400–8.
Dhindsa S, Miller MG, McWhirter CL, et al. Testosterone concentrations in diabetic and nondiabetic obese men. Diabetes Care. 2010;33:1186–92.
Hofstra J, Loves S, van Wageningen B, et al. High prevalence of hypogonadotropic hypogonadism in men referred for obesity treatment. Neth J Med. 2008;66:103–9.
Dandona P, Dhindsa S. Update: hypogonadotropic hypogonadism in type 2 diabetes and obesity. J Clin Endocrinol Metab. 2011;96:2643–51.
Dallal RM, Chernoff A, O'Leary MP, et al. Sexual dysfunction is common in the morbidly obese male and improves after gastric bypass surgery. J Am Coll Surg. 2008;207:859–64.
Reis LO, Favaro WJ, Barreiro GC, et al. Erectile dysfunction and hormonal imbalance in morbidly obese male is reversed after gastric bypass surgery: a prospective randomized controlled trial. Int J Androl. 2010;33:736–44.
Giagulli VA, Kaufman JM, Vermeulen A. Pathogenesis of the decreased androgen levels in obese men. J Clin Endocrinol Metab. 1994;79:997–1000.
Aggerholm AS, Thulstrup AM, Toft G, et al. Is overweight a risk factor for reduced semen quality and altered serum sex hormone profile? Fertil Steril. 2008;90:619–26.
Hammoud A, Gibson M, Hunt SC, et al. Effect of Roux-en-Y gastric bypass surgery on the sex steroids and quality of life in obese men. J Clin Endocrinol Metab. 2009;94:1329–32.
Bastounis EA, Karayiannakis AJ, Syrigos K, et al. Sex hormone changes in morbidly obese patients after vertical banded gastroplasty. Eur Surg Res. 1998;30:43–7.
Alagna S, Cossu ML, Gallo P, et al. Biliopancreatic diversion: long-term effects on gonadal function in severely obese men. Surg Obes Relat Dis. 2006;2:82–6.
Globerman H, Shen-Orr Z, Karnieli E, et al. Inhibin B in men with severe obesity and after weight reduction following gastroplasty. Endocr Res. 2005;31:17–26.
Strain GW. Zumoffb, Miller LD et al. Effect of massive weight loss on hypothalamic–pituitary–gonadal function in obese men. J Clin Endocrinol Metab. 1988;66:1019–23.
National Cholesterol Education Program (NCEP). Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III). Third report of the National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III) final report. Circulation. 2002;106:3143–421.
Deitel M, Crosby RD, Gagner M. The First International Consensus Summit for sleeve gastrectomy (SG), New York City, October 25–27, 2007. Obes Surg. 2008;18(5):487–96.
Pérez-Romero N, Serra A, Granada ML, et al. Effects of two variants of Roux-en-Y gastric bypass on metabolism behaviour: focus on plasma ghrelin concentrations over a 2-year follow-up. Obes Surg. 2010;20:600–9.
Vermeulen A, Verdonck L, Kaufman JM. A critical evaluation of simple methods for the estimation of free testosterone in serum. J Clin Endocrinol Metab. 1999;84:3666–72.
Rosner W, Auchus RJ, Azziz R, et al. Position statement: utility, limitations, and pitfalls in measuring testosterone: an Endocrine Society position statement. J Clin Endocrinol Metab. 2007;92:405–13.
Isidori AM, Caprio M, Strollo F, et al. Leptin and androgens in male obesity: evidence for leptin contribution to reduced androgen levels. J Clin Endocrinol Metab. 1999;84:3673–80.
Pasquali R, Casimirri F, De R I, et al. Insulin regulates testosterone and sex hormone-binding globulin concentrations in adult normal weight and obese men. J Clin Endocrinol Metab. 1995;80:654–8.
Mingrone G, Greco AV, Giancaterini A, et al. Sex hormone-binding globulin levels and cardiovascular risk factors in morbidly obese subjects before and after weight reduction induced by diet or malabsorptive surgery. Atherosclerosis. 2002;161:455–62.
Bhasin S, Cunningham GR, Hayes FJ, et al. Testosterone therapy in men with androgen deficiency syndromes: an Endocrine Society clinical practice guideline. J Clin Endocrinol Metab. 2010;95:2536–59.
Zumoff B, Strain GW, Miller LK, et al. Plasma free and non-sex-hormone-binding-globulin-bound testosterone are decreased in obese men in proportion to their degree of obesity. J Clin Endocrinol Metab. 1990;71:929–31.
Rao SR, Kini S, Tamler R. Sex hormones and bariatric surgery in men. Gend Med. 2011;8:300–11.
Travison TG, Araujo AB, Kupelian V, et al. The relative contributions of aging, health, and lifestyle factors to serum testosterone decline in men. J Clin Endocrinol Metab. 2007;92:549–55.
Wang C, Nieschlag E. Swerdloff R et al; International Society of Andrology (ISA); International Society for the Study of Aging Male (ISSAM); European Association of Urology (EAU); European Academy of Andrology (EAA); American Society of Andrology (ASA) Investigation, treatment, and monitoring of late-onset hypogonadism in males: ISA, ISSAM, EAU, EAA, and ASA recommendations. J Androl. 2009;30:1–9.
Laaksonen DE, Niskanen L, Punnonen K, et al. Testosterone and sex hormone-binding globulin predict the metabolic syndrome and diabetes in middle-aged men. Diabetes Care. 2004;27:1036–41.
Caprio M, Isidori AM, Carta AR, et al. Expression of functional leptin receptors in rodent Leydig cells. Endocrinology. 1999;140:4939–47.
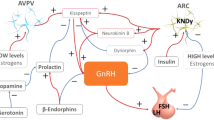
Tena-Sempere M. KiSS-1 and reproduction: focus on its role in the metabolic regulation of fertility. Neuroendocrinology. 2006;83:275–81.
Dungan HM, Clifton DK, Steiner RA. Minireview: kisspeptin neurons as central processors in the regulation of gonadotropin-releasing hormone secretion. Endocrinology. 2006;147:1154–8.
MacDonald AA, Herbison GP, Showell M, et al. The impact of body mass index on semen parameters and reproductive hormones in human males: a systematic review with meta-analysis. Hum Reprod Update. 2010;16:293–311.
Teerds KJ, de Rooij DG, Keijer J. Functional relationship between obesity and male reproduction: from humans to animal models. Hum Reprod Updat. 2011;17:667–83.
Håkonsen LB, Thulstrup AM, Aggerholm AS, et al. Does weight loss improve semen quality and reproductive hormones? Results from a cohort of severely obese men. Reprod Health. 2011;17:24.
Kelleher S, Conway AJ, Handelsman DJ. Blood testosterone threshold for androgen deficiency symptoms. J Clin Endocrinol Metab. 2004;89:3813–7.
Zumoff B, Miller LK, Strain GW. Reversal of the hypogonadotropic hypogonadism of obese men by administration of the aromatase inhibitor testolactone. Metabolism. 2003;52:1126–8.
Conflict of interest
The authors declare that there is no conflict of interest that could be perceived as prejudicing the impartiality of the research reported.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Pellitero, S., Olaizola, I., Alastrue, A. et al. Hypogonadotropic Hypogonadism in Morbidly Obese Males Is Reversed After Bariatric Surgery. OBES SURG 22, 1835–1842 (2012). https://doi.org/10.1007/s11695-012-0734-9
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-012-0734-9