Abstract
Background and Objective
The role of liver resection in advanced hepatocellular carcinoma (multinodular or with macroscopic vascular involvement) is still controversial. The aim of this study is to evaluate the role of surgical resection compared to other therapeutic modalities in patients with advanced hepatocellular carcinoma (HCC).
Methods
Four hundred sixty four patients with HCC observed from 1991 to 2007 were included in the study. All the patients were evaluated for the treatment of HCC in relation to the severity of liver impairment and tumor stage. All the patients included in the study had no evidence of distant metastases.
Results
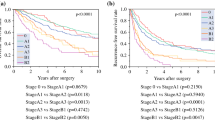
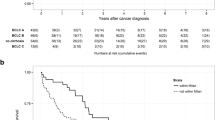
Median follow up time for surviving patients was 25 months (range 1–155). Two-hundred and eighty-three patients were in Child–Pugh class A, 161 in class B, and 20 in class C. Two-hundred and seventy-one patients had single HCC, 121 patients had two or three HCCs, and 72 more than three HCCs. One-hundred and thirty-six patients (29.3%) were submitted to liver resection (LR), 232 (50.0%) to local ablative therapies (LAT) (ethanol injection, radiofrequency ablation, chemoembolization), eight (1.7%) to liver transplantation (LT), and 88 (19%) to supportive therapy (ST). Median survival time for all patients was 36 months (95% CI 24–36). Median survival time was 57 months for LR, 30 months for LAT, and 8 months for ST, with a 5-year survival of 47%, 20%, and 2.5%, respectively (p = 0.001). Actuarial 5-year survival for patients submitted to LT was 75%. Overall survival was significantly shorter in patients with multiple HCCs compared to single HCC, with median survival times of 39, 16, and 11 months for patients with a single HCC, with two to three HCCs, and with more than three HCCs, respectively (p = 0.01). Survival for patients with single HCC was significantly longer in patients submitted to LR compared to LAT and ST with median survival times of 57, 37, and 14 months, respectively (p = 0.02). Also, in patients with multinodular HCCs (2–3 HCCs) LR showed the best results with a median survival time of 58 months compared to 22 and 8 months for LAT and ST (p = 0.01). In patients with more than three HCCs, LR did not show different results compared to LAT and ST. Seventy-three patients had evidence of macroscopic vascular involvement; median survival in this subgroup of patients was significantly shorter compared to patients without vascular involvement, 10 and 36 months, respectively. Survival for patients with macroscopic vascular involvement submitted to LR or LAT was significant longer compared to ST, with mean survivals of 27, 30, and 12 months, respectively (p = 0.01).
Conclusions
The present study shows that the surgery can achieve good results in patients with single HCC and good liver function. Also, patients with multinodular HCCs (two to three nodules) could benefit from LR where survival is longer than after LAT or ST. In patients with more than three HCCs, LR have similar results of LAT. Macroscopic vascular invasion is a major prognostic factor, and the LR is justified in selected patients, where it can allow good long-term results compared to ST.
Similar content being viewed by others
References
Parkin DM, Bray F, Ferlay J, Pisani P. Estimating the world cancer burden: Globocan 2000. Int J Cancer. 2001;94(2):153–156. doi:10.1002/ijc.1440.
Abdalla EK, Denys A, Hasegawa K, Leung TW, Makuuchi M, Murthy R, et al. Treatment of large and advanced hepatocellular carcinoma. Ann Surg Oncol. 2008;15(4):979–985. doi:10.1245/s10434-007-9727-7.
Wakabayashi H, Ushiyama T, Ishimura K, Izuishi K, Karasawa Y, Masaki T, et al. Significance of reduction surgery in multidisciplinary treatment of advanced hepatocellular carcinoma with multiple intrahepatic lesions. J Surg Oncol. 2003;82(2):98–103. doi:10.1002/jso.10203.
Chen XP, Qiu FZ, Wu ZD, Zhang ZW, Huang ZY, Chen YF, et al. Effects of location and extension of portal vein tumor thrombus on long-term outcomes of surgical treatment for hepatocellular carcinoma. Ann Surg Oncol. 2006;13(7):940–946. doi:10.1245/ASO.2006.08.007.
Ng KK, Vauthey JN, Pawlik TM, Lauwers GY, Regimbeau JM, Belghiti J, et al. Is hepatic resection for large or multinodular hepatocellular carcinoma justified? Results from a multi-institutional database. Ann Surg Oncol. 2005;12(5):364–373. doi:10.1245/ASO.2005.06.004.
Bruix J, Sherman M, Llovet JM, Beaugrand M, Lencioni R, Burroughs AK, et al. Clinical management of hepatocellular carcinoma. Conclusions of the Barcelona-2000 EASL conference. European Association for the Study of the Liver. J Hepatol. 2001;35(3):421–430. doi:10.1016/S0168-8278(01)00130-1.
Llovet JM, Burroughs A, Bruix J. Hepatocellular carcinoma. Lancet 2003;362(9399):1907–1917. doi:10.1016/S0140-6736(03)14964-1.
Ikai I, Arii S, Okazaki M, Okita K, Omata M, Kojiro M, et al. Report of the 17th Nationwide Follow-up Survey of Primary Liver Cancer in Japan. Hepatol Res. 2007;37(9):676–691. doi:10.1111/j.1872-034X.2007.00119.x.
Llovet JM, Schwartz M, Mazzaferro V. Resection and liver transplantation for hepatocellular carcinoma. Semin Liver Dis. 2005;25(2):181–200. doi:10.1055/s-2005-871198.
Benckert C, Jonas S, Thelen A, Spinelli A, Schumacher G, Heise M, et al. Liver transplantation for hepatocellular carcinoma in cirrhosis: prognostic parameters. Transplant Proc. 2005;37(4):1693–1694. doi:10.1016/j.transproceed.2005.03.143.
Guglielmi A, Ruzzenente A, Battocchia A, Tonon A, Fracastoro G, Cordiano C. Radiofrequency ablation of hepatocellular carcinoma in cirrhotic patients. Hepatogastroenterology 2003;50(50):480–484.
Lau WY, Lai EC. Hepatocellular carcinoma: current management and recent advances. Hepatobiliary Pancreat Dis Int. 2008;7(3):237–257.
Llovet JM, Bruix J. Systematic review of randomized trials for unresectable hepatocellular carcinoma: Chemoembolization improves survival. Hepatology 2003;37(2):429–442. doi:10.1053/jhep.2003.50047.
Lau W. Future perspectives for hepatocellular carcinoma. HPB Oxf. 2003;5(4):206–213.
Fan J, Zhou J, Wu ZQ, Qiu SJ, Wang XY, Shi YH, et al. Efficacy of different treatment strategies for hepatocellular carcinoma with portal vein tumor thrombosis. World J Gastroenterol. 2005;11(8):1215–1219.
Fan J, Wu ZQ, Zhou J, Qiu SJ, Shi YH, Chen RX, et al. Hepatocellular carcinoma associated with tumor thrombosis in the portal vein: the effects of different treatments. Hepatobiliary Pancreat Dis Int. 2003;2(4):513–519.
Pawlik TM, Delman KA, Vauthey JN, Nagorney DM, Ng IO, Ikai I, et al. Tumor size predicts vascular invasion and histologic grade: Implications for selection of surgical treatment for hepatocellular carcinoma. Liver Transpl. 2005;11(9):1086–1092. doi:10.1002/lt.20472.
Ishizawa T, Hasegawa K, Aoki T, Takahashi M, Inoue Y, Sano K, et al. Neither multiple tumors nor portal hypertension are surgical contraindications for hepatocellular carcinoma. Gastroenterology 2008;134(7):1908–1916. doi:10.1053/j.gastro.2008.02.091.
Liu CL, Fan ST, Lo CM, Ng IO, Poon RT, Wong J. Hepatic resection for bilobar hepatocellular carcinoma: is it justified? Arch Surg. 2003;138(1):100–104.
Pawarode A, Voravud N, Sriuranpong V, Kullavanijaya P, Patt YZ. Natural history of untreated primary hepatocellular carcinoma: a retrospective study of 157 patients. Am J Clin Oncol. 1998;21(4):386–391. doi:10.1097/00000421-199808000-00014.
Llovet JM, Bustamante J, Castells A, Vilana R, Ayuso Mdel C, Sala M, et al. Natural history of untreated nonsurgical hepatocellular carcinoma: rationale for the design and evaluation of therapeutic trials. Hepatology 1999;29(1):62–67. doi:10.1002/hep.510290145.
Liver Cancer Study Group of Japan. Primary liver cancer in Japan. Clinicopathologic features and results of surgical treatment. Ann Surg. 1990;211(3):277–287.
Poon RT, Fan ST. Evaluation of the new AJCC/UICC staging system for hepatocellular carcinoma after hepatic resection in Chinese patients. Surg Oncol Clin N Am. 2003;12(1):35–50, viii. doi:10.1016/S1055-3207(02)00086-8.
Minagawa M, Makuuchi M, Takayama T, Ohtomo K. Selection criteria for hepatectomy in patients with hepatocellular carcinoma and portal vein tumor thrombus. Ann Surg. 2001;233(3):379–384. doi:10.1097/00000658-200103000-00012.
Fan J, Wu ZQ, Tang ZY, Zhou J, Qiu SJ, Ma ZC, et al. Multimodality treatment in hepatocellular carcinoma patients with tumor thrombi in portal vein. World J Gastroenterol. 2001;7(1):28–32.
Author information
Authors and Affiliations
Corresponding author
Additional information
This study was presented as Quick Shot oral presentation of the Surgical Society Alimentary Tract at Digestive Disease Week, May 20, 2008, San Diego Convention Center, San Diego, CA, USA and as oral presentation at 23rd Annual SSAT Residents & Fellows Research Conference, May 17, 2008, Omni San Diego, San Diego, CA.
Rights and permissions
About this article
Cite this article
Ruzzenente, A., Capra, F., Pachera, S. et al. Is Liver Resection Justified in Advanced Hepatocellular Carcinoma? Results of an Observational Study in 464 Patients. J Gastrointest Surg 13, 1313–1320 (2009). https://doi.org/10.1007/s11605-009-0903-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11605-009-0903-x