Abstract
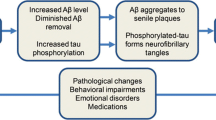
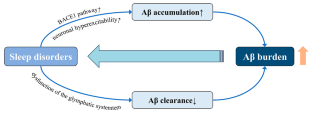
Sleep disorders affect many people worldwide and can accompany neurodegenerative and psychiatric diseases. Sleep may be altered before the clinical manifestations of some of these diseases appear. Moreover, some sleep disorders affect the physiological organization and function of the brain by influencing gene expression, accelerating the accumulation of abnormal proteins, interfering with the clearance of abnormal proteins, or altering the levels of related hormones and neurotransmitters, which can cause or may be associated with the development of neurodegenerative and psychiatric diseases. However, the detailed mechanisms of these effects are unclear. This review mainly focuses on the relationship between and mechanisms of action of sleep in Alzheimer’s disease, depression, and anxiety, as well as the relationships between sleep and Parkinson’s disease, Huntington’s disease, and amyotrophic lateral sclerosis. This summary of current research hotspots may provide researchers with better clues and ideas to develop treatment solutions for neurodegenerative and psychiatric diseases associated with sleep disorders.

Similar content being viewed by others
Abbreviations
- Aβ:
-
Amyloid β-protein
- AD:
-
Alzheimer’s disease
- ALS:
-
Amyotrophic lateral sclerosis
- APP:
-
Amyloid precursor protein
- AQP4:
-
Aquaporin 4
- ASD:
-
Acute sleep deprivation
- BACE1:
-
Β-site APP cleaving enzyme 1
- BDNF:
-
Brain-derived neurotrophic factor
- BMAL1:
-
Brain and muscle arnt-like protein-1
- CSD:
-
Chronic sleep deprivation
- CSF:
-
Cerebrospinal fluid
- CSR:
-
Chronic sleep restriction
- HD:
-
Huntington’s disease
- HPA:
-
Hypothalamic-pituitary-adrenal
- IL:
-
Interleukin
- ISF:
-
Interstitial fluid
- Keap1:
-
Kelch-like ECH-associated protein 1
- LB:
-
Lewy body
- LRP-1:
-
Low-density lipoprotein receptor-related protein 1
- MCI:
-
Mild cognitive impairment
- NC:
-
Normal cognition
- NREM:
-
Non-rapid eye movement
- Nrf2:
-
Nuclear factor erythroid 2-related factor
- OSA:
-
Obstructive sleep apnea
- PD:
-
Parkinson’s disease
- RAGE:
-
Receptor of advanced glycation end products
- RBD:
-
Rapid eye movement sleep-behavior disorder
- REM:
-
Rapid eye movement
- SD:
-
Sleep deprivation
- SDB:
-
Sleep-disordered breathing
- SWA:
-
Slow-wave activity
- SWS:
-
Slow wave sleep
- TDP-43:
-
43-kDa TAR DNA-binding protein
- TSD:
-
Total sleep deprivation
- WT:
-
Wild-type
References
Grandner MA, Fernandez FX (2021) The translational neuroscience of sleep: a contextual framework. Science 374:568–573
Voysey Z, Fazal SV, Lazar AS, Barker RA (2021) The sleep and circadian problems of Huntington’s Disease: when, why and their importance. J Neurol 268:2275–2283
Joiner WJ (2018) The neurobiological basis of Sleep and Sleep disorders. Physiol (Bethesda) 33:317–327
Léger D, Bayon V (2010) Societal costs of insomnia. Sleep Med Rev 14:379–389
Hillman DR, Lack LC (2013) Public health implications of sleep loss: the community burden. Med J Aust 199:S7–10
Latreille MKP V (2019) Sleep disorders. Am J Med 132:292–299
Liew SC, Aung T (2021) Sleep deprivation and its association with diseases- a review. Sleep Med 77:192–204
Banks S, Dinges DF (2007) Behavioral and physiological consequences of sleep restriction. J Clin Sleep Med 3:519–528
Umemura GS, Furtado F, Dos Santos FC, Gonçalves B, Forner-Cordero A (2022) Is Balance Control affected by Sleep Deprivation? A systematic review of the impact of Sleep on the control of balance. Front Neurosci 16:779086
Pires GN, Bezerra AG, Tufik S, Andersen ML (2016) Effects of acute sleep deprivation on state anxiety levels: a systematic review and meta-analysis. Sleep Med 24:109–118
Colwell CS (2021) Defining circadian disruption in neurodegenerative disorders. J Clin Invest 131
Fang H, Tu S, Sheng J, Shao A (2019) Depression in sleep disturbance: a review on a bidirectional relationship, mechanisms and treatment. J Cell Mol Med 23:2324–2332
Wang YQ, Li R, Zhang MQ, Zhang Z, Qu WM, Huang ZL (2015) The neurobiological mechanisms and treatments of REM sleep disturbances in Depression. Curr Neuropharmacol 13:543–553
Guo B, Zhang M, Hao W, Wang Y, Zhang T, Liu C (2023) Neuroinflammation mechanisms of neuromodulation therapies for anxiety and depression. Transl Psychiatry 13:5
Gauthier S, Webster C, Servaes S, Morais JA, Rosa-Neto P (2022) World Alzheimer Report 2022: Life after diagnosis: Navigating treatment, care and support. In. Alzheimer’s Disease International, London, England
Okuda S, Tetsuka J, Takahashi K, Toda Y, Kubo T, Tokita S (2019) Association between sleep disturbance in Alzheimer’s Disease patients and burden on and health status of their caregivers. J Neurol 266:1490–1500
Kastanenka KV, Hou SS, Shakerdge N, Logan R, Feng D, Wegmann S, Chopra V, Hawkes JM, Chen X, Bacskai BJ (2017) Optogenetic restoration of disrupted slow oscillations halts amyloid deposition and restores Calcium Homeostasis in an animal model of Alzheimer’s Disease. PLoS ONE 12:e0170275
Suh SW, Han JW, Lee JR, Byun S, Kwon SJ, Oh SH, Lee KH, Han G, Hong JW, Kwak KP, Kim BJ, Kim SG, Kim JL, Kim TH, Ryu SH, Moon SW, Park JH, Seo J, Youn JC, Lee DY, Lee DW, Lee SB, Lee JJ, Jhoo JH, Kim KW (2018) Sleep and cognitive decline: a prospective nondemented elderly cohort study. Ann Neurol 83:472–482
Lucey BP, Wisch J, Boerwinkle AH, Landsness EC, Toedebusch CD, McLeland JS, Butt OH, Hassenstab J, Morris JC, Ances BM, Holtzman DM (2021) Sleep and longitudinal cognitive performance in preclinical and early symptomatic Alzheimer’s Disease. Brain 144:2852–2862
Maestri M, Carnicelli L, Tognoni G, Di Coscio E, Giorgi FS, Volpi L, Economou NT, Ktonas P, Ferri R, Bonuccelli U, Bonanni E (2015) Non-rapid eye movement sleep instability in mild cognitive impairment: a pilot study. Sleep Med 16:1139–1145
Pase MP, Himali JJ, Grima NA, Beiser AS, Satizabal CL, Aparicio HJ, Thomas RJ, Gottlieb DJ, Auerbach SH, Seshadri S (2017) Sleep architecture and the risk of incident Dementia in the community. NEUROLOGY 89:1244–1250
Lucey BP, McCullough A, Landsness EC, Toedebusch CD, McLeland JS, Zaza AM, Fagan AM, McCue L, **ong C, Morris JC, Benzinger TLS, Holtzman DM (2019) Reduced non-rapid eye movement sleep is associated with tau pathology in early Alzheimer’s disease. Sci Transl Med 11
Liu S, Meng Y, Wang N, Lei Q, He L, Hong X, Li Z (2023) Disturbance of REM sleep exacerbates microglial activation in APP/PS1 mice. Neurobiol Learn Mem 200:107737
Chylinski D, Van Egroo M, Narbutas J, Muto V, Bahri MA, Berthomier C, Salmon E, Bastin C, Phillips C, Collette F, Maquet P, Carrier J, Lina JM, Vandewalle G (2022) Timely coupling of sleep spindles and slow waves linked to early amyloid-β burden and predicts memory decline. eLife 11
Chylinski DO, Van Egroo M, Narbutas J, Grignard M, Koshmanova E, Berthomier C, Berthomier P, Brandewinder M, Salmon E, Bahri MA, Bastin C, Collette F, Phillips C, Maquet P, Muto V, Vandewalle G (2021) Heterogeneity in the links between sleep arousals, amyloid-β, and cognition. JCI Insight 6
Winer JR, Deters KD, Kennedy G, ** M, Goldstein-Piekarski A, Poston KL, Mormino EC (2021) Association of short and long sleep duration with Amyloid-β Burden and Cognition in Aging. JAMA Neurol 78:1187–1196
Fan L, Xu W, Cai Y, Hu Y, Wu C (2019) Sleep duration and the risk of Dementia: a systematic review and Meta-analysis of prospective cohort studies. J Am Med Dir Assoc 20:1480–1487e1485
Leng Y, Ackley SF, Glymour MM, Yaffe K, Brenowitz WD (2021) Genetic risk of Alzheimer’s Disease and Sleep Duration in Non-demented elders. Ann Neurol 89:177–181
Xu W, Tan L, Su BJ, Yu H, Bi YL, Yue XF, Dong Q, Yu JT (2020) Sleep characteristics and cerebrospinal fluid biomarkers of Alzheimer’s Disease pathology in cognitively intact older adults: the CABLE study. Alzheimers Dement 16:1146–1152
Cavaillès C, Berr C, Helmer C, Gabelle A, Jaussent I, Dauvilliers Y (2022) Complaints of daytime sleepiness, insomnia, hypnotic use, and risk of Dementia: a prospective cohort study in the elderly. Alzheimers Res Ther 14:12
Anderson EL, Richmond RC, Jones SE, Hemani G, Wade KH, Dashti HS, Lane JM, Wang H, Saxena R, Brumpton B, Korologou-Linden R, Nielsen JB, Åsvold BO, Abecasis G, Coulthard E, Kyle SD, Beaumont RN, Tyrrell J, Frayling TM, Munafò MR, Wood AR, Ben-Shlomo Y, Howe LD, Lawlor DA, Weedon MN, Davey Smith G (2021) Is disrupted sleep a risk factor for Alzheimer’s Disease? Evidence from a two-sample mendelian randomization analysis. Int J Epidemiol 50:817–828
André C, Rehel S, Kuhn E, Landeau B, Moulinet I, Touron E, Ourry V, Le Du G, Mézenge F, Tomadesso C, de Flores R, Bejanin A, Sherif S, Delcroix N, Manrique A, Abbas A, Marchant NL, Lutz A, Klimecki OM, Collette F, Arenaza-Urquijo EM, Poisnel G, Vivien D, Bertran F, de la Sayette V, Chételat G, Rauchs G (2020) Association of Sleep-Disordered Breathing with Alzheimer Disease biomarkers in Community-Dwelling older adults: a secondary analysis of a Randomized Clinical Trial. JAMA Neurol 77:716–724
Lee JE, Yang SW, Ju YJ, Ki SK, Chun KH (2019) Sleep-disordered breathing and Alzheimer’s Disease: a nationwide cohort study. Psychiatry Res 273:624–630
Liguori C, Maestri M, Spanetta M, Placidi F, Bonanni E, Mercuri NB, Guarnieri B (2021) Sleep-disordered breathing and the risk of Alzheimer’s Disease. Sleep Med Rev 55:101375
Bubu OM, Andrade AG, Umasabor-Bubu OQ, Hogan MM, Turner AD, de Leon MJ, Ogedegbe G, Ayappa I, Jean-Louis GG, Jackson ML, Varga AW, Osorio RS (2020) Obstructive sleep apnea, cognition and Alzheimer’s Disease: a systematic review integrating three decades of multidisciplinary research. Sleep Med Rev 50:101250
Sharma RA, Varga AW, Bubu OM, Pirraglia E, Kam K, Parekh A, Wohlleber M, Miller MD, Andrade A, Lewis C, Tweardy S, Buj M, Yau PL, Sadda R, Mosconi L, Li Y, Butler T, Glodzik L, Fieremans E, Babb JS, Blennow K, Zetterberg H, Lu SE, Badia SG, Romero S, Rosenzweig I, Gosselin N, Jean-Louis G, Rapoport DM, de Leon MJ, Ayappa I, Osorio RS (2018) Obstructive sleep apnea severity affects amyloid Burden in Cognitively Normal Elderly. A longitudinal study. Am J Respir Crit Care Med 197:933–943
Punjabi NM (2008) The epidemiology of adult obstructive sleep apnea. Proc Am Thorac Soc 5:136–143
Ooms S, Overeem S, Besse K, Rikkert MO, Verbeek M, Claassen JA (2014) Effect of 1 night of total sleep deprivation on cerebrospinal fluid β-amyloid 42 in healthy middle-aged men: a randomized clinical trial. JAMA Neurol 71:971–977
Lucey BP, Hicks TJ, McLeland JS, Toedebusch CD, Boyd J, Elbert DL, Patterson BW, Baty J, Morris JC, Ovod V, Mawuenyega KG, Bateman RJ (2018) Effect of sleep on overnight cerebrospinal fluid amyloid β kinetics. Ann Neurol 83:197–204
Benedict C, Blennow K, Zetterberg H, Cedernaes J (2020) Effects of acute sleep loss on diurnal plasma dynamics of CNS health biomarkers in young men. NEUROLOGY 94:e1181–e1189
Wei M, Zhao B, Huo K, Deng Y, Shang S, Liu J, Li Y, Ma L, Jiang Y, Dang L, Chen C, Wei S, Zhang J, Yang H, Gao F, Qu Q (2017) Sleep Deprivation Induced plasma Amyloid-β transport disturbance in healthy young adults. J Alzheimers Dis 57:899–906
Ju Y-ES, Ooms SJ, Sutphen C, Macauley SL, Zangrilli MA, Jerome G, Fagan AM, Mignot E, Zempel JM, Claassen JAHR, Holtzman DM (2017) Slow wave sleep disruption increases cerebrospinal fluid amyloid-β levels. Brain 140:2104–2111
Qiu H, Zhong R, Liu H, Zhang F, Li S, Le W (2016) Chronic sleep deprivation exacerbates Learning-Memory disability and Alzheimer’s Disease-Like pathologies in AβPP(swe)/PS1(∆E9) mice. J Alzheimers Dis 50:669–685
Zhao HY, Wu HJ, He JL, Zhuang JH, Liu ZY, Huang LQ, Zhao ZX (2017) Chronic sleep restriction induces cognitive deficits and cortical Beta-amyloid deposition in mice via BACE1-Antisense activation. CNS Neurosci Ther 23:233–240
Zhao B, Liu P, Wei M, Li Y, Liu J, Ma L, Shang S, Jiang Y, Huo K, Wang J, Qu Q (2019) Chronic sleep restriction induces Aβ Accumulation by disrupting the balance of Aβ production and clearance in rats. Neurochem Res 44:859–873
**e Y, Ba L, Wang M, Deng SY, Chen SM, Huang LF, Zhang M, Wang W, Ding FF (2020) Chronic sleep fragmentation shares similar pathogenesis with neurodegenerative Diseases: Endosome-autophagosome-lysosome pathway dysfunction and microglia-mediated neuroinflammation. CNS Neurosci Ther 26:215–227
Vasciaveo V, Iadarola A, Casile A, Dante D, Morello G, Minotta L, Tamagno E, Cicolin A, Guglielmotto M (2023) Sleep fragmentation affects glymphatic system through the different expression of AQP4 in wild type and 5xFAD mouse models. Acta Neuropathol Commun 11:16
Nick H, Fenik P, Zhu Y, Veasey S (2022) Hypocretin/orexin influences chronic sleep disruption injury in the hippocampus. Front Aging Neurosci 14:1025402
Kent BA, Feldman HH, Nygaard HB (2021) Sleep and its regulation: an emerging pathogenic and treatment frontier in Alzheimer’s Disease. Prog Neurobiol 197:101902
Tabuchi M, Lone SR, Liu S, Liu Q, Zhang J, Spira AP, Wu MN (2015) Sleep interacts with aβ to modulate intrinsic neuronal excitability. Curr Biol 25:702–712
Ba L, Huang L, He Z, Deng S, **e Y, Zhang M, Jacob C, Antonecchia E, Liu Y, **ao W, **e Q, Huang Z, Yi C, D’Ascenzo N, Ding F (2021) Does chronic sleep fragmentation lead to Alzheimer’s Disease in Young Wild-Type mice? Front Aging Neurosci 13:759983
Owen JE, Zhu Y, Fenik P, Zhan G, Bell P, Liu C, Veasey S (2021) Late-in-life neurodegeneration after chronic sleep loss in young adult mice. Sleep 44
Zhang F, Niu L, Zhong R, Li S, Le W (2023) Chronic sleep disturbances alters Sleep structure and tau phosphorylation in AβPP/PS1 AD mice and their wild-type littermates. J Alzheimers Dis 92:1341–1355
Zhu Y, Zhan G, Fenik P, Brandes M, Bell P, Francois N, Shulman K, Veasey S (2018) Chronic sleep disruption advances the temporal progression of Tauopathy in P301S Mutant mice. J Neurosci 38:10255–10270
Niu L, Zhang F, Xu X, Yang Y, Li S, Liu H, Le W (2022) Chronic sleep deprivation altered the expression of circadian clock genes and aggravated Alzheimer’s Disease neuropathology. Brain Pathol 32:e13028
Lucey BP (2020) It’s complicated: the relationship between sleep and Alzheimer’s Disease in humans. Neurobiol Dis 144:105031
Sato C, Barthélemy NR, Mawuenyega KG, Patterson BW, Gordon BA, Jockel-Balsarotti J, Sullivan M, Crisp MJ, Kasten T, Kirmess KM, Kanaan NM, Yarasheski KE, Baker-Nigh A, Benzinger TLS, Miller TM, Karch CM, Bateman RJ (2018) Tau kinetics in neurons and the Human Central Nervous System. Neuron 98:861–864
Yanamandra K, Patel TK, Jiang H, Schindler S, Ulrich JD, Boxer AL, Miller BL, Kerwin DR, Gallardo G, Stewart F, Finn MB, Cairns NJ, Verghese PB, Fogelman I, West T, Braunstein J, Robinson G, Keyser J, Roh J, Knapik SS, Hu Y, Holtzman DM (2017) Anti-tau antibody administration increases plasma tau in transgenic mice and patients with tauopathy. Sci Transl Med 9
Yamada K, Holth JK, Liao F, Stewart FR, Mahan TE, Jiang H, Cirrito JR, Patel TK, Hochgräfe K, Mandelkow EM, Holtzman DM (2014) Neuronal activity regulates extracellular tau in vivo. J Exp Med 211:387–393
Holth JK, Fritschi SK, Wang C, Pedersen NP, Cirrito JR, Mahan TE, Finn MB, Manis M, Geerling JC, Fuller PM, Lucey BP, Holtzman DM (2019) The sleep-wake cycle regulates brain interstitial fluid tau in mice and CSF tau in humans. Sci (New York NY) 363:880–884
Irwin MR, Vitiello MV (2019) Implications of sleep disturbance and inflammation for Alzheimer’s Disease Dementia. Lancet Neurol 18:296–306
Wu R, Tripathy S, Menon V, Yu L, Buchman AS, Bennett DA, De Jager PL, Lim ASP (2022) Fragmentation of rest periods, astrocyte activation, and cognitive decline in older adults with and without Alzheimer’s disease. Alzheimers Dement
Kaneshwaran K, Olah M, Tasaki S, Yu L, Bradshaw EM, Schneider JA, Buchman AS, Bennett DA, De Jager PL, Lim ASP (2019) Sleep fragmentation, microglial aging, and cognitive impairment in adults with and without Alzheimer’s Dementia. Sci Adv 5:eaax7331
Bellesi M, de Vivo L, Chini M, Gilli F, Tononi G, Cirelli C (2017) Sleep loss promotes astrocytic phagocytosis and microglial activation in mouse cerebral cortex. J Neurosci 37:5263–5273
Kincheski GC, Valentim IS, Clarke JR, Cozachenco D, Castelo-Branco MTL, Ramos-Lobo AM, Rumjanek V, Donato J Jr., De Felice FG, Ferreira ST (2017) Chronic sleep restriction promotes Brain Inflammation and synapse loss, and potentiates memory impairment induced by amyloid-β oligomers in mice. Brain Behav Immun 64:140–151
Liu P, Zhao B, Wei M, Li Y, Liu J, Ma L, Shang S, Huo K, Wang J, Li R, Qu Q (2020) Activation of inflammation is Associated with Amyloid-β Accumulation Induced by Chronic Sleep restriction in rats. J Alzheimers Dis 74:759–773
Berk M, Williams LJ, Jacka FN, O’Neil A, Pasco JA, Moylan S, Allen NB, Stuart AL, Hayley AC, Byrne ML, Maes M (2013) So depression is an inflammatory Disease, but where does the inflammation come from? BMC Med 11:200
Siegel JM (2005) Clues to the functions of mammalian sleep. Nature 437:1264–1271
Wulff K, Gatti S, Wettstein JG, Foster RG (2010) Sleep and circadian rhythm disruption in psychiatric and neurodegenerative Disease. Nat Rev Neurosci 11:589–599
Mendoza J (2019) Circadian insights into the biology of depression: symptoms, treatments and animal models. Behav Brain Res 376:112186
Chellappa SL, Aeschbach D (2022) Sleep and anxiety: from mechanisms to interventions. Sleep Med Rev 61:101583
Mirchandaney R, Barete R, Asarnow LD (2022) Moderators of cognitive behavioral treatment for Insomnia on Depression and anxiety outcomes. Curr Psychiatry Rep 24:121–128
Soehner AM, Kaplan KA, Harvey AG (2014) Prevalence and clinical correlates of co-occurring insomnia and hypersomnia symptoms in depression. J Affect Disord 167:93–97
Zhou F, Li S, Xu H (2022) Insomnia, sleep duration, and risk of anxiety: a two-sample mendelian randomization study. J Psychiatr Res 155:219–225
Bean CAL, Ciesla JA (2021) Naturalistic partial sleep deprivation leads to Greater Next-Day anxiety: the moderating role of baseline anxiety and depression. Behav Ther 52:861–873
Palmer CA, Alfano CA (2020) Anxiety modifies the emotional effects of sleep loss. Curr Opin Psychol 34:100–104
Zhou L, Zhang H, Luo Z, Liu X, Yang L, Hu H, Wang Y, Wang C, Wang F (2020) Abnormal night sleep duration and inappropriate sleep initiation time are associated with elevated anxiety symptoms in Chinese rural adults: the Henan Rural Cohort. Psychiatry Res 291:113232
Riemann D (2007) Insomnia and comorbid psychiatric disorders. Sleep Med 8(Suppl 4):S15–20
Lopez R, Barateau L, Evangelista E, Dauvilliers Y (2017) Depression and Hypersomnia: a Complex Association. Sleep Med Clin 12:395–405
Luik AI, Zuurbier LA, Direk N, Hofman A, Van Someren EJ, Tiemeier H (2015) 24-HOUR ACTIVITY RHYTHM AND SLEEP DISTURBANCES IN DEPRESSION AND ANXIETY: A POPULATION-BASED STUDY OF MIDDLE-AGED AND OLDER PERSONS. Depress Anxiety 32:684–692
Bouwmans ME, Conradi HJ, Bos EH, Oldehinkel AJ, de Jonge P (2017) Bidirectionality between sleep symptoms and core depressive symptoms and their long-term course in Major Depression. Psychosom Med 79:336–344
Casement MD, Keenan KE, Hipwell AE, Guyer AE, Forbes EE (2016) Neural reward Processing mediates the relationship between insomnia symptoms and Depression in Adolescence. Sleep 39:439–447
Coles ME, Schubert JR, Nota JA (2015) Sleep, circadian rhythms, and anxious traits. Curr Psychiatry Rep 17:73
Horváth A, Montana X, Lanquart JP, Hubain P, Szűcs A, Linkowski P, Loas G (2016) Effects of state and trait anxiety on sleep structure: a polysomnographic study in 1083 subjects. Psychiatry Res 244:279–283
Short MA, Louca M (2015) Sleep deprivation leads to mood deficits in healthy adolescents. Sleep Med 16:987–993
Taraku B, Zavaliangos-Petropulu A, Loureiro JR, Al-Sharif NB, Kubicki A, Joshi SH, Woods RP, Espinoza R, Narr KL, Sahib AK (2023) White matter microstructural perturbations after total sleep deprivation in depression. Front Psychiatry 14:1195763
Hu B, Liu C, Mou T, Luo F, Lv T, Qian C, Zhang J, Ye M, Liu Z (2021) Meta-analysis of Sleep Deprivation effects on patients with Depression. Front Psychiatry 12:783091
Dong L, **e Y, Zou X (2022) Association between sleep duration and depression in US adults: a cross-sectional study. J Affect Disord 296:183–188
Tartar JL, Ward CP, Cordeira JW, Legare SL, Blanchette AJ, McCarley RW, Strecker RE (2009) Experimental sleep fragmentation and sleep deprivation in rats increases exploration in an open field test of anxiety while increasing plasma corticosterone levels. Behav Brain Res 197:450–453
Pires GN, Bezerra AG, Tufik S, Andersen ML (2016) Effects of experimental sleep deprivation on anxiety-like behavior in animal research: systematic review and meta-analysis. Neurosci Biobehav Rev 68:575–589
Finan PH, Quartana PJ, Smith MT (2015) The effects of Sleep Continuity disruption on positive Mood and Sleep Architecture in healthy adults. Sleep 38:1735–1742
Meerlo P, Mistlberger RE, Jacobs BL, Heller HC, McGinty D (2009) New neurons in the adult brain: the role of sleep and consequences of sleep loss. Sleep Med Rev 13:187–194
Clasadonte J, McIver SR, Schmitt LI, Halassa MM, Haydon PG (2014) Chronic sleep restriction disrupts sleep homeostasis and behavioral sensitivity to alcohol by reducing the extracellular accumulation of adenosine. J Neurosci 34:1879–1891
Arvin P, Ghafouri S, Bavarsad K, Hajipour S, Khoshnam SE, Sarkaki A, Farbood Y (2023) Administration of growth hormone ameliorates adverse effects of total sleep deprivation. Metab Brain Dis 38:1671–1681
Klumpers UM, Veltman DJ, van Tol MJ, Kloet RW, Boellaard R, Lammertsma AA, Hoogendijk WJ (2015) Neurophysiological effects of sleep deprivation in healthy adults, a pilot study. PLoS ONE 10:e0116906
Jordan W, Tumani H, Cohrs S, Eggert S, Rodenbeck A, Brunner E, Rüther E, Hajak G (2004) Prostaglandin D synthase (beta-trace) in healthy human sleep. Sleep 27:867–874
Zhang Y, Dai C, Shao Y, Peng J, Yang Y, Hou Y (2021) Decreased functional connectivity in the reward network and its relationship with negative emotional experience after total sleep deprivation. Front Neurol 12:641810
Bosch OG, Rihm JS, Scheidegger M, Landolt HP, Stämpfli P, Brakowski J, Esposito F, Rasch B, Seifritz E (2013) Sleep deprivation increases dorsal nexus connectivity to the dorsolateral prefrontal cortex in humans. Proc Natl Acad Sci U S A 110:19597–19602
Lopez-Rodriguez F, Wilson CL, Maidment NT, Poland RE, Engel J (2003) Total sleep deprivation increases extracellular serotonin in the rat hippocampus. Neuroscience 121:523–530
Wu JC, Gillin JC, Buchsbaum MS, Schachat C, Darnall LA, Keator DB, Fallon JH, Bunney WE (2008) Sleep deprivation PET correlations of Hamilton symptom improvement ratings with changes in relative glucose metabolism in patients with depression. J Affect Disord 107:181–186
Grassi Zucconi G, Cipriani S, Balgkouranidou I, Scattoni R (2006) One night’ sleep deprivation stimulates hippocampal neurogenesis. Brain Res Bull 69:375–381
Tartar JL, Ward CP, McKenna JT, Thakkar M, Arrigoni E, McCarley RW, Brown RE, Strecker RE (2006) Hippocampal synaptic plasticity and spatial learning are impaired in a rat model of sleep fragmentation. Eur J Neurosci 23:2739–2748
Grubac Z, Sutulovic N, Ademovic A, Velimirovic M, Rasic-Markovic A, Macut D, Petronijevic N, Stanojlovic O, Hrncic D (2019) Short-term sleep fragmentation enhances anxiety-related behavior: the role of hormonal alterations. PLoS ONE 14:e0218920
Nair D, Zhang SX, Ramesh V, Hakim F, Kaushal N, Wang Y, Gozal D (2011) Sleep fragmentation induces cognitive deficits via nicotinamide adenine dinucleotide phosphate oxidase-dependent pathways in mouse. Am J Respir Crit Care Med 184:1305–1312
Stepnowsky CJ, Palau JJ, Zamora T, Ancoli-Israel S, Loredo JS (2011) Fatigue in sleep apnea: the role of depressive symptoms and self-reported sleep quality. Sleep Med 12:832–837
Gong L, Liao T, Liu D, Luo Q, Xu R, Huang Q, Zhang B, Feng F, Zhang C (2019) Amygdala Changes in Chronic Insomnia and Their Association with sleep and anxiety symptoms: insight from shape analysis. Neural Plast 2019:8549237
Gong L, Shi M, Wang J, Xu R, Yu S, Liu D, Ding X, Zhang B, Zhang X, ** C (2021) The abnormal functional connectivity in the Locus Coeruleus-Norepinephrine System Associated with anxiety Symptom in Chronic Insomnia Disorder. Front Neurosci 15:678465
Xu M, Wang Q, Li B, Qian S, Wang S, Wang Y, Chen C, Liu Z, Ji Y, Liu K, **n K, Niu Y (2023) Cerebellum and hippocampus abnormalities in patients with insomnia comorbid depression: a study on cerebral blood perfusion and functional connectivity. Front Neurosci 17:1202514
Motomura Y, Katsunuma R, Ayabe N, Oba K, Terasawa Y, Kitamura S, Moriguchi Y, Hida A, Kamei Y, Mishima K (2021) Decreased activity in the reward network of chronic insomnia patients. Sci Rep 11:3600
Gong L, Yu S, Xu R, Liu D, Dai X, Wang Z, Hu Y, Yan B, Kui Y, Zhang B, Feng F (2021) The abnormal reward network associated with insomnia severity and depression in chronic insomnia disorder. Brain Imaging Behav 15:1033–1042
Rahmani M, Rahmani F, Rezaei N (2020) The brain-derived neurotrophic factor: missing Link between Sleep Deprivation, Insomnia, and Depression. Neurochem Res 45:221–231
Schmitt K, Holsboer-Trachsler E, Eckert A (2016) BDNF in sleep, insomnia, and sleep deprivation. Ann Med 48:42–51
Konakanchi S, Raavi V, Ml HK, Shankar Ms V (2022) Effect of chronic sleep deprivation and sleep recovery on hippocampal CA3 neurons, spatial memory and anxiety-like behavior in rats. Neurobiol Learn Mem 187:107559
**a M, Li Z, Li S, Liang S, Li X, Chen B, Zhang M, Dong C, Verkhratsky A, Guan D, Li B (2020) Sleep Deprivation Selectively Down-Regulates Astrocytic 5-HT(2B) Receptors and Triggers Depressive-Like Behaviors via Stimulating P2X(7) Receptors in Mice. Neurosci Bull 36:1259–1270
Manchanda S, Singh H, Kaur T, Kaur G (2018) Low-grade neuroinflammation due to chronic sleep deprivation results in anxiety and learning and memory impairments. Mol Cell Biochem 449:63–72
Kiecolt-Glaser JK, Derry HM, Fagundes CP (2015) Inflammation: depression fans the flames and feasts on the heat. Am J Psychiatry 172:1075–1091
Liu H, Huang X, Li Y, ** K, Han Y, Mao H, Ren K, Wang W, Wu Z (2022) TNF signaling pathway-mediated microglial activation in the PFC underlies acute paradoxical sleep deprivation-induced anxiety-like behaviors in mice. Brain Behav Immun 100:254–266
Merikanto I, Partonen T (2021) Eveningness increases risks for depressive and anxiety symptoms and hospital treatments mediated by insufficient sleep in a population-based study of 18,039 adults. Depress Anxiety 38:1066–1077
Stahl ST, Smagula SF, Rodakowski J, Dew MA, Karp JF, Albert SM, Butters M, Gildengers A, Reynolds CF 3rd (2021) Subjective Sleep Quality and trajectories of Interleukin-6 in older adults. Am J Geriatr Psychiatry 29:204–208
Selvi Y, Boysan M, Kandeger A, Uygur OF, Sayin AA, Akbaba N, Koc B (2018) Heterogeneity of sleep quality in relation to circadian preferences and depressive symptomatology among major depressive patients. J Affect Disord 235:242–249
Taylor BJ, Hasler BP (2018) Chronotype and Mental Health: recent advances. Curr Psychiatry Rep 20:59
Merikanto I, Kronholm E, Peltonen M, Laatikainen T, Vartiainen E, Partonen T (2015) Circadian preference links to depression in general adult population. J Affect Disord 188:143–148
Schapira AHV, Chaudhuri KR, Jenner P (2017) Non-motor features of Parkinson Disease. Nat Rev Neurosci 18:435–450
Stefani A, Högl B (2020) Sleep in Parkinson’s Disease. NEUROPSYCHOPHARMACOLOGY 45:121–128
Morawska MM, Moreira CG, Ginde VR, Valko PO, Weiss T, Büchele F, Imbach LL, Masneuf S, Kollarik S, Prymaczok N, Gerez JA, Riek R, Baumann CR, Noain D (2021) Slow-wave sleep affects synucleinopathy and regulates proteostatic processes in mouse models of Parkinson’s Disease. Sci Transl Med 13:eabe7099
Zuzuárregui JRP, During EH (2020) Sleep issues in Parkinson’s Disease and their management. Neurotherapeutics 17:1480–1494
Hermanowicz N, Jones SA, Hauser RA (2019) Impact of non-motor symptoms in Parkinson’s Disease: a PMDAlliance survey. Neuropsychiatr Dis Treat 15:2205–2212
Kay DB, Tanner JJ, Bowers D (2018) Sleep disturbances and depression severity in patients with Parkinson’s Disease. Brain Behav 8:e00967
Latif S, Jahangeer M, Maknoon Razia D, Ashiq M, Ghaffar A, Akram M, El Allam A, Bouyahya A, Garipova L, Ali Shariati M, Thiruvengadam M, Azam Ansari M (2021) Dopamine in Parkinson’s Disease. Clin Chim Acta 522:114–126
Dauvilliers Y, Schenck CH, Postuma RB, Iranzo A, Luppi PH, Plazzi G, Montplaisir J, Boeve B (2018) REM sleep behaviour disorder. Nat Rev Dis Primers 4:19
Miglis MG, Adler CH, Antelmi E, Arnaldi D, Baldelli L, Boeve BF, Cesari M, Dall’Antonia I, Diederich NJ, Doppler K, Dušek P, Ferri R, Gagnon JF, Gan-Or Z, Hermann W, Högl B, Hu MT, Iranzo A, Janzen A, Kuzkina A, Lee JY, Leenders KL, Lewis SJG, Liguori C, Liu J, Lo C, Ehgoetz Martens KA, Nepozitek J, Plazzi G, Provini F, Puligheddu M, Rolinski M, Rusz J, Stefani A, Summers RLS, Yoo D, Zitser J, Oertel WH (2021) Biomarkers of conversion to α-synucleinopathy in isolated rapid-eye-movement sleep behaviour disorder. Lancet Neurol 20:671–684
Si XL, Gu LY, Song Z, Zhou C, Fang Y, ** CY, Wu JJ, Gao T, Guo T, Guan XJ, Xu XJ, Yin XZ, Yan YP, Zhang MM, Pu JL (2020) Different Perivascular Space burdens in Idiopathic Rapid Eye Movement Sleep Behavior Disorder and Parkinson’s Disease. Front Aging Neurosci 12:580853
Maggi G, Trojano L, Barone P, Santangelo G (2021) Sleep disorders and cognitive dysfunctions in Parkinson’s Disease: a Meta-Analytic Study. Neuropsychol Rev 31:643–682
Lin YQ, Chen SD (2018) RBD: a red flag for cognitive impairment in Parkinson’s Disease? Sleep Med 44:38–44
Lazar AS, Panin F, Goodman AO, Lazic SE, Lazar ZI, Mason SL, Rogers L, Murgatroyd PR, Watson LP, Singh P, Borowsky B, Shneerson JM, Barker RA (2015) Sleep deficits but no metabolic deficits in Premanifest Huntington’s Disease. Ann Neurol 78:630–648
Vas S, Nicol AU, Kalmar L, Miles J, Morton AJ (2021) Abnormal patterns of sleep and EEG power distribution during non-rapid eye movement sleep in the sheep model of Huntington’s Disease. Neurobiol Dis 155:105367
Cabanas M, Pistono C, Puygrenier L, Rakesh D, Jeantet Y, Garret M, Cho YH (2019) Neurophysiological and behavioral effects of anti-orexinergic treatments in a mouse model of Huntington’s Disease. Neurotherapeutics: The Journal of the American Society for Experimental NeuroTherapeutics 16:784–796
Hulisz D (2018) Amyotrophic Lateral Sclerosis: Disease state overview. Am J Manag Care 24:S320–s326
Liu S, Ren Q, Gong G, Sun Y, Zhao B, Ma X, Zhang N, Zhong S, Lin Y, Wang W, Zheng R, Yu X, Yun Y, Zhang D, Shao K, Lin P, Yuan Y, Dai T, Zhang Y, Li L, Li W, Zhao Y, Shan P, Meng X, Yan C (2022) Hypothalamic subregion abnormalities are related to body mass index in patients with sporadic Amyotrophic Lateral Sclerosis. J Neurol 269:2980–2988
Gnoni V, Zoccolella S, Giugno A, Urso D, Tamburrino L, Filardi M, Logroscino G (2023) Hypothalamus and Amyotrophic Lateral Sclerosis: potential implications in sleep disorders. Front Aging Neurosci 15:1193483
Lo Martire V, Caruso D, Palagini L, Zoccoli G, Bastianini S (2020) Stress & sleep: a relationship lasting a lifetime. Neurosci Biobehav Rev 117:65–77
Basta M, Vgontzas AN, Fernandez-Mendoza J, Antypa D, Li Y, Zaganas I, Panagiotakis S, Karagkouni E, Simos P (2022) Basal cortisol levels are increased in patients with mild cognitive impairment: role of Insomnia and short sleep duration. J Alzheimers Dis 87:933–944
Gabery S, Ahmed RM, Caga J, Kiernan MC, Halliday GM, Petersén Å (2021) Loss of the metabolism and sleep regulating neuronal populations expressing orexin and oxytocin in the hypothalamus in Amyotrophic Lateral Sclerosis. Neuropathol Appl Neurobiol 47:979–989
Boentert M (2019) Sleep disturbances in patients with Amyotrophic Lateral Sclerosis: current perspectives. Nat Sci Sleep 11:97–111
Acknowledgements
We would like to thank Editage (www.editage.cn) for English language editing.
Funding
This study was supported by grants from the National Natural Science Foundation of China (No. 82371541), the project for the improvement of research skill in Anhui Medical University (No.2021xkjT003), Talent Training Program from the School of Basic Medical Sciences of Anhui Medical University (No. 2022YPJH201), Research Fund of Anhui Institute of translational medicine (No. 2022zhyx-C11) and National Training Project of Innovation and Entrepreneurship for Undergraduates of China (No. 202310366060 & No. 202310366037).
Author information
Authors and Affiliations
Contributions
All authors contributed to the manuscript. X.X. had the idea for the article. X.X., Y.M.R. and Y. J. performed the literature search, drafted the manuscript and created the figures. M.C. revised critically the manuscript. All authors read and approved the manuscript.
Corresponding author
Ethics declarations
Competing Interests
The authors have no relevant financial or non-financial interests to disclose.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
**ao, X., Rui, Y., **, Y. et al. Relationship of Sleep Disorder with Neurodegenerative and Psychiatric Diseases: An Updated Review. Neurochem Res 49, 568–582 (2024). https://doi.org/10.1007/s11064-023-04086-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11064-023-04086-5