Abstract
Background
Non-alcoholic fatty liver disease (NAFLD) is defined as the most prevalent hepatic disorder that affects a significant population worldwide. There are several genes/proteins, involving in the modulation of NAFLD pathogenesis; sirtuin1 (SIRT1), TP53-inducible regulator gene (TIGAR), and autophagy-related gene 5 (Atg5) are considered a chief group of these modulators that principally act by regulating the hepatic lipid metabolism, as well as preventing the lipid accumulation. Surprisingly, bilirubin, especially in its unconjugated form, might be able to alleviate NAFLD progression by decreasing lipid accumulation and regulating the expression levels of the above-stated genes.
Methods and results
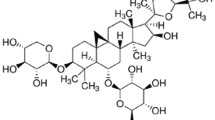
Herein, the interactions between bilirubin and the corresponding genes’ products were first analyzed by docking assessments. Afterwards, HepG2 cells were cultured under the optimum conditions, and then were incubated with high concentrations of glucose to induce NAFLD. After treating normal and fatty liver cells with particular bilirubin concentrations for 24- and 48-hour periods, 3-[4,5-dimethylthiazol-2-yl]-2,5-diphenyl-tetrazolium bromide (MTT) assay, colorimetric method, and quantitative reverse transcriptase-polymerase chain reaction (qRT-PCR) were employed to assess cell viability status, intracellular triglycerides content, and mRNA expression levels of the genes, respectively. Intracellular lipid accumulation of HepG2 cells was significantly decreased after treating with bilirubin. Bilirubin also increased SIRT1 and Atg5 gene expression levels in fatty liver cells. TIGAR gene expression levels were variable upon the conditions and the cell type, suggesting a dual role for TIGAR during the NAFLD pathogenesis.
Conclusion
Our findings indicate the potential of bilirubin in the prevention from or amelioration of NAFLD through influencing SIRT1-related deacetylation and the process of lipophagy, as well as decreasing the intrahepatic lipid content.
Graphical abstract
In vitro model of NAFLD was treated with unconjugated bilirubin under the optimal conditions.Desirably, bilirubin moderated the accumulation of triglycerides within the cells possibly through modulation of the expression of SIRT1, Atg5, and TIGAR genes. In the context, bilirubin was shown to increase the expression levels of SIRT1 and Atg5, while the expression of TIGAR was demonstrated to be either increased or decreased, depending on the treatment conditions. Created with BioRender.com.







Similar content being viewed by others
Data availability
All datasets analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- Atg5/ATG5:
-
Autophagy-related gene/protein 5
- BLVRA:
-
Biliverdin reductase
- CLOCK:
-
Circadian Locomotor Output Cycles Kaput
- CREB:
-
cAMP response element-binding protein
- FOXO:
-
Fork head box class O
- GSH:
-
Reduced form of glutathione
- HCC:
-
Hepatocellular carcinoma
- HMOX:
-
Heme oxygenase
- IRS-2:
-
Insulin receptor substrate 2
- LC3:
-
Light chain 3
- LXR:
-
Liver X-receptor
- 3-MA:
-
3-methyladenine
- NAD+ :
-
Nicotinamide adenine dinucleotide
- NAFLD:
-
Non-alcoholic fatty liver disease
- NF-κB:
-
Nuclear Factor-κB
- PDB:
-
Protein Data Bank
- PER2:
-
Period circadian regulator 2
- PGC-1a:
-
PPAR gamma co-activator 1α
- PPAR:
-
Peroxisome proliferator-activated receptor
- SIRT1:
-
Silent information regulation homology 1
- SPPARM:
-
Selective PPAR modulator
- SREBP1c:
-
Sterol regulatory element binding protein 1c
- TIGAR:
-
TP53 inducible glycolysis and apoptosis regulator
- TG:
-
Triglycerides
- TORC2:
-
Transducer of regulated CREB protein 2
- UCB:
-
Unconjugated bilirubin
- UGT1A1:
-
UDP-glucuronosyltransferase
References
McNeice K, Sandberg K (2020) Updates in non-alcoholic fatty liver disease (NAFLD). Curr Probl Pediatr Adolesc Health Care 50(8):100844
Loomba R et al (2021) Mechanisms and disease consequences of nonalcoholic fatty liver disease. Cell 184(10):2537–2564
Kawaguchi T, Torimura T (2020) Is metabolic syndrome responsible for the progression from NAFLD to NASH in non-obese patients? Springer
Targher G et al (2021) Non-alcoholic fatty liver disease: a multisystem disease requiring a multidisciplinary and holistic approach. lancet Gastroenterol Hepatol 6(7):578–588
Maurice J, Manousou P (2018) Non-alcoholic fatty liver disease. Clin Med 18(3):245
Ding R-B et al (2017) Emerging roles of SIRT1 in fatty liver diseases. Int J Biol Sci 13(7):852
Nikroo H et al (2020) The effect of aerobic, resistance, and combined training on PPAR-α, SIRT1 gene expression, and insulin resistance in high-fat diet-induced NAFLD male rats. Physiol Behav 227:113149
Borji M et al (2019) Down-regulation of SIRT1 expression by mir-23b contributes to lipid accumulation in HepG2 cells. Biochem Genet 57(4):507–521
Hsu WW et al (2016) Sirtuins 1 and 2 are universal histone deacetylases. ACS Chem Biol 11(3):792–799
Klein MA, Denu JM (2020) Biological and catalytic functions of sirtuin 6 as targets for small-molecule modulators. J Biol Chem 295(32):11021–11041
Geng J et al (2018) The diverse role of TIGAR in cellular homeostasis and cancer. Free Radic Res 52(11–12):1240–1249
Tang J et al (2021) Structure, regulation, and biological functions of TIGAR and its role in diseases. Acta Pharmacol Sin 42(10):1547–1555
Napoli M, Flores ER (2017) The p53 family orchestrates the regulation of metabolism: physiological regulation and implications for cancer therapy. Br J Cancer 116(2):149–155
Yan Z et al (2018) p53 as a double-edged sword in the progression of non-alcoholic fatty liver disease. Life Sci 215:64–72
Mao Y et al (2016) Autophagy: a new target for nonalcoholic fatty liver disease therapy. Hepatic medicine: evidence and research 8:27
Sinha RA et al (2020) Hepatic lipid catabolism via PPARα-lysosomal crosstalk. Int J Mol Sci 21(7):2391
Luo L et al (2018) Genetically regulated bilirubin and risk of non-alcoholic fatty liver disease: a mendelian randomization study. Front Genet 9:662
Fujiwara R et al (2018) Systemic regulation of bilirubin homeostasis: potential benefits of hyperbilirubinemia. Hepatology 67(4):1609–1619
Novák P et al (2020) Bilirubin in metabolic syndrome and associated inflammatory diseases: new perspectives. Life Sci 257:118032
Saffari-Chaleshtori J et al (2021) Inhibitory effects of bilirubin on colonization and migration of A431 and SK-MEL-3 skin cancer cells compared with human dermal fibroblasts (HDF). Cancer Invest 39(9):721–733
Yousefi Z et al (2020) microRNA-141 is associated with hepatic steatosis by downregulating the sirtuin1/AMP‐activated protein kinase pathway in hepatocytes. J Cell Physiol 235(2):880–890
Vogel ME et al (2017) Bilirubin prevents atherosclerotic lesion formation in low-density lipoprotein receptor‐deficient mice by inhibiting endothelial VCAM‐1 and ICAM‐1 signaling.Journal of the American Heart Association6 (4), e004820
Wu B et al (2019) Heme catabolic pathway in inflammation and immune disorders. Front Pharmacol 10:825
DiNicolantonio JJ et al (2018) Antioxidant bilirubin works in multiple ways to reduce risk for obesity and its health complications.Open Heart5 (2), e000914
Tian J et al (2016) Association between bilirubin and risk of non-alcoholic fatty liver Disease based on a prospective cohort study. Sci Rep 6(1):1–9
Puri K et al (2013) Serum bilirubin level is inversely associated with nonalcoholic steatohepatitis in children. J Pediatr Gastroenterol Nutr 57(1):114–118
Kunutsor SK et al (2020) Circulating total bilirubin and risk of non-alcoholic fatty liver disease in the PREVEND study: observational findings and a mendelian randomization study. Eur J Epidemiol 35:123–137
Yao Z et al (2013) Using molecular docking-based binding energy to predict toxicity of binary mixture with different binding sites. Chemosphere 92(9):1169–1176
Carradori S et al (2022) Resveratrol Analogues as dual inhibitors of Monoamine Oxidase B and Carbonic anhydrase VII: a New Multi-Target Combination for neurodegenerative Diseases? Molecules 27(22):7816
Stec DE et al (2016) Bilirubin binding to PPARα inhibits lipid accumulation. PLoS ONE 11(4):e0153427
Hinds TD Jr et al (2016) Does bilirubin prevent hepatic steatosis through activation of the PPARα nuclear receptor? Medical hypotheses 95, 54–57
Hinds TD Jr et al (2020) Bilirubin nanoparticles reduce diet-induced hepatic steatosis, improve fat utilization, and increase plasma β-hydroxybutyrate. Front Pharmacol 11:594574
Gordon DM et al (2019) RNA sequencing in human HepG2 hepatocytes reveals PPAR-α mediates transcriptome responsiveness of bilirubin. Physiol Genom 51(6):234–240
Pan S et al (2019) MicroRNA-128 is involved in dexamethasone-induced lipid accumulation via repressing SIRT1 expression in cultured pig preadipocytes. J Steroid Biochem Mol Biol 186:185–195
Jiang Y et al (2019) Signaling network of forkhead family of transcription factors (FOXO) in dietary restriction. Cells 9(1):100
Zhang X et al (2019) Unraveling the regulation of hepatic gluconeogenesis. Front Endocrinol 9:802
Higgins CB et al (2022) SIRT1 selectively exerts the metabolic protective effects of hepatocyte nicotinamide phosphoribosyltransferase. Nat Commun 13(1):1–17
Shi T, Dansen TB (2020) Reactive oxygen species induced p53 activation: DNA damage, redox signaling, or both? Antioxid Redox Signal 33(12):839–859
Shah ZH et al (2012) A deacetylase-deficient SIRT1 variant opposes full-length SIRT1 in regulating tumor suppressor p53 and governs expression of cancer-related genes. Mol Cell Biol 32(3):704–716
Liou C-J et al (2018) Fisetin protects against hepatic steatosis through regulation of the Sirt1/AMPK and fatty acid β-oxidation signaling pathway in high-fat diet-induced obese mice. Cell Physiol Biochem 49(5):1870–1884
Li C-X et al (2019) Allyl isothiocyanate ameliorates lipid accumulation and inflammation in nonalcoholic fatty liver disease via the Sirt1/AMPK and NF-κB signaling pathways. World J Gastroenterol 25(34):5120
Wang L et al (2018) Endoplasmic reticulum stress related molecular mechanisms in nonalcoholic fatty liver disease (NAFLD). Curr Drug Targets 19(9):1087–1094
Zhang X et al (2020) Galangin Improved Non-Alcoholic Fatty Liver Disease in Mice by Promoting Autophagy. Drug Design, Development and Therapy 14, 3393
Li Y et al (2020) Role of mechanistic target of Rapamycin and Autophagy in Alcohol-Induced Adipose Atrophy and Liver Injury. Am J Pathol 190(1):158–175
Tanaka S et al (2016) Rubicon inhibits autophagy and accelerates hepatocyte apoptosis and lipid accumulation in nonalcoholic fatty liver disease in mice. Hepatology 64(6):1994–2014
Acknowledgements
This research has been extracted from the M.Sc. thesis of Omid Vakili and was supported by Grant Number 97-01-01-17291 from Vice-chancellor for Research Affairs of Shiraz University of Medical Sciences, Shiraz, Iran.
Funding
This work was supported by Vice-chancellor for Research Affairs of Shiraz University of Medical Sciences (Grant number 97-01-01-17291).
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation, data collection, and analyses were performed by [Omid Vakili], [Javad Saffari-Chaleshtori], [Mohammad Borji], and [Sayed Mohammad Shafiee]. The first draft of the manuscript was written by [Omid Vakili] and all authors commented on previous versions of the manuscript. Supervision and project administration were conducted by [Sayed Mohammad Shafiee]. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors do not have any financial or non-financial interests to declare.
Ethical approval
This is an observational study. The Research Ethics Committee of Shiraz University of Medical Sciences has confirmed that no ethical approval is required.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Vakili, O., Borji, M., Saffari-Chaleshtori, J. et al. Ameliorative effects of bilirubin on cell culture model of non-alcoholic fatty liver disease. Mol Biol Rep 50, 4411–4422 (2023). https://doi.org/10.1007/s11033-023-08339-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11033-023-08339-y