Abstract
The intensive care unit (ICU) environment is rich in both medical device and electronic medical record (EMR) data. The ICU patient population is particularly vulnerable to medical error or delayed medical intervention both of which are associated with excess morbidity, mortality and cost. The development and deployment of smart alarms, computerized decision support systems (DSS) and “sniffers” within ICU clinical information systems has the potential to improve the safety and outcomes of critically ill hospitalized patients. However, the current generations of alerts, run largely through bedside monitors, are far from ideal and rarely support the clinician in the early recognition of complex physiologic syndromes or deviations from expected care pathways. False alerts and alert fatigue remain prevalent. In the coming era of widespread EMR implementation novel medical informatics methods may be adaptable to the development of next generation, rule-based DSS.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
1 Introduction
“Decision Support System” is a generic term for any computer application that enhances an individual’s or group’s ability to make decisions. Computerized decision support systems (DSS) became feasible with the development of microcomputers in the mid-1960s. These systems were initially researched and used in production scheduling, financial analysis and clinical medicine [1]. In the medical arena, where decision-making is predominantly driven by patient data and clinical knowledge, DSS finds a natural niche.
The fundamental goal of clinical medicine is to make decisions that match the patient with a correct diagnosis and treatment plan. However, with the advent of electronic medical records, the volume of new data being generated continues to grow and threatens overwhelming physicians with “information overload”. On that background, DSS has been proposed as a potential solution [2, 3]. As an example, ventilated patients in the intensive care unit (ICU) are attached to multiple diagnostic, monitoring and therapeutic devices, all generating data and alerts. An estimated 40 alarms can be activated by such patients at any given instance [4]. These alerts represent examples of DSS built on algorithms within medical devices required to have high sensitivity for critical events. Unfortunately these alerts rarely result in meaningful clinical interventions and often contribute to alert fatigue in the ICU.
2 Problems with alarm-based decision support
The Joint Commission on Accreditation of Healthcare Organizations defines a clinical alarm as any alarm that is intended to protect the individual receiving care or alert the staff that the individual is at increased risk and needs immediate assistance [5]. The complexity of the technology used in the ICU setting greatly contributes to the occurrence of errors and adverse events. The need for monitoring in acute care environment such as ICU and the operation room (OR) was clearly established by malpractice claims analysis. In the OR 32 % of negative outcomes cases were potentially preventable by additional monitoring [6].
Notably, adverse events in ICUs occur at a rate of 81 per 1,000 patient-days and serious errors occur at a rate of 150 per 1,000 patient-days [7]. Nearly half (45 %) of such adverse events in the Critical Care Safety Study were deemed preventable [7]. As designed, device-embedded alarms are intended to monitor vital cardiopulmonary functions and to increase patient safety and quality of care by allowing early detection of significant abnormalities [4]. However, in study by Tsien and Fackler, only 8 % of all alarms were determined to be true alarms with associated clinical significance [8]. Furthermore, one of the earliest attempt to classify the rate of false ICU alarms demonstrated that only eight out of 1,455 alerts indicated a life-treating situation [9]. In a landmark paper, Lawless investigated alarms in a pediatric ICU and demonstrated that 94 % of the generated alarms were not clinically important [10]. Schoenberg et al. also found that most of the alarms generated by bedside monitors were clinically insignificant and only distracted bedside providers [11].
Frequent and particularly false alerts, come with a cost. The most significant is alert fatigue. With high alarm frequency, care providers risk becoming “desensitized” [12] and/or confused [13]. High numbers of false-positive alarms push clinicians to change thresholds to inappropriate levels, or to simply ignore them. All of these responses can lead to serious adverse effects.
Sound pollution is another important disadvantage of false alarms. Noise levels in hospitals are escalating. Sound pressure levels in the ICU are frequently in excess of the permissible noise exposure recommended by the US Environmental Protection Agency (45 dBA per 24 h with peaks up to 96 dBAper 24 h above the threshold of hearing) [14]. Alarms contribute significantly to this increase. Noise, especially from alarms [15], has been implicated as the one of the five most common reasons for poor sleep quality in the ICU [16].
The problem of information overload has been identified as a key factor in medical errors [17]. False alerts contribute to this problem. Ideally clinical providers should be alerted only when events are clinically significant and there is opportunity for correction. But this is difficult to define and implement in automated systems [18]. This difficulty stems from a lack of data to analyze alarms, lack of evidence-based rationale for the configuration of alarms and the disconnected state of current EMR components. Preliminary studies using rule-based alerts and computer-generated messages directed at clinicians have been shown to decrease the length of hospital stay [19].
Various approaches have been attempted in an effort to reduce the number of false alerts. Complex methods such as artificial intelligence, statistical approaches and human factors can all decrease the rate of false alerts, but these have not been widely implemented in medical devices. Simpler methods such as averaging repeated measurements, signal filtering or improving signal–noise ratio can also be moderately effective. For instance, the number of ineffective alarms in a Medical ICU was reduced by 67 % by automatically detecting airway suctioning, patient repositioning, oral care, and blood gas sampling, while concomitantly introducing a 19 s alarm delay [20]. Improved medical device interoperability and integration is another important strategy to reduce problems associated with the high level of false alerts found in these environments [21]. An excellent review by Imhoff covers these aspects of reducing false medical devices alerts [22].
3 Patient medical records
Originally, computerized systems were simply used for the automated collection of data from bedside monitors [23]. A limitation of this approach was the lack of associated context relating the data acquired to the environment from which it was extracted. Importantly, it is not until data is enriched with this additional context that it becomes meaningful information that can be appropriately acted upon by the health care team. Fortunately, with the increasing ability to automatically acquire and digitize this additional complimentary data, especially in data rich environments such as the ICU [24], computers are becoming an invaluable tool for processing data in a more meaningful way [25].
With the growing adoption of EMRs, more and more patient information is becoming available in a digital format. However, the lack of true integration of EMRs into the clinical workflow remains a critical barrier to their successful adoption [26]. Currently, EMR usability and acceptance is poor because of design without reference to the context and end user experience [27]. Integration of multidimensional clinical data from multiple source systems into a single database in real-time, will be crucial for the development of a platform for rule-based decision support systems of the future [28].
Notably, the US Department of Health and Human Services has recognized the potential advantages of EMRs in healthcare delivery and have actively promoted their adoption [29]. Recent federal legislation created a new path forward. The Health Information Technology for Economic and Clinical Health (HITECH) Act, a part of the American Recovery and Reinvestment Act (ARRA) of 2009, authorized expenditures to promote the adoption and use of EMR technologies [30, 31].
Clinical alerts and notifications through stand-alone bedside monitors are an important feature of the clinical electronic environment. They have been shown to improve both the quality [32, 33] and cost [34] of medical care. Clinical alerting systems and event monitors have also demonstrated improved efficiency by shortening the time to implementing appropriate treatments [35, 36]. However, bedside monitors are not designed for early recognition of complex physiologic syndromes. Novel medical informatics methods such as continuous syndromic surveillance screening, which is extensively used in the prevention of bioterrorism, represents an attractive alternative, particularly in the current era of growing adoption of EMRs.
4 Rule-based smart alerts
A new paradigm in medical care is the constant surveillance of multiple streams of patient information with the goal of early diagnosis of acute and potentially catastrophic illnesses [37, 38]. Implementation of EMRs allow for expansion of these techniques in the areas of clinical medicine, quality improvement, patient safety, and research [38].
The term “syndromic surveillance” refers to methods which rely on the early detection of discernible clinical case features before confirmed diagnoses are made [38]. This field has enjoyed substantial growth after the events of September 11, 2001, when real-time threat surveillance became a subject of a concentrated national effort [39]. The application of this technology in emergency and critical care medicine, where the timing of appropriate interventions is of high importance for patient outcome, it is obviously appealing.
Early attempts at the development of intelligent alarm systems, or sniffers, for the detection of complex clinical conditions have shown promising results. Sniffers for syndromes with established definitions have shown high sensitivity and specificity in multiple settings. Acute lung injury automatic detection strategies demonstrated a sensitivity of 96 % and a specificity of 89 % [40] [41, 42]. Real-time electronic alert algorithms for acute kidney injury (AKI), which are based on RIFLE classification criteria (risk, injury and failure) have shown a sensitivity of 100 % and a specificity of 96.8 % [43] in detection of this important syndrome. Early detection of severe sepsis and septic shock is a topic that has been actively researched over the years [44, 45].
A proactive, rather than reactive, approach to monitoring can help identify clinically relevant problems early and may result in more timely implementation of appropriate interventions. “Digital signatures”, algorithms that reliably identify specific provider actions, patient pre-morbid conditions, health states and response to intervention is a key component of future intelligent alert systems. A good example of the application of digital signatures to a clinical problem is the ventilator induced lung injury (VILI) sniffer. This sniffer provides fully automated screening of EMR data including ventilator settings, patient characteristics and provider actions. By integrating data from multiple sources and accessing the hospital communications systems, the VILI sniffer alerts the relevant bedside provider of a specific patient if it detects deviations from expected standards of care. In this case provider alerts are only generated if a patient at risk of acute lung injury is being ventilated with potentially injurious mechanical ventilator settings. Implementation of this rule-based alerting system demonstrated good positive predictive value, and was associated with decreased patient exposure to injurious ventilator settings associated with improved patient outcomes [46].
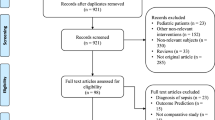
The ideal rule-based alerting system should operate reliably in the clinical setting and must enhance, rather than interfere with, the health care team’s workflow. Developers of such alerting systems need to account for the clinical condition, the patient characteristics and the specific healthcare environment in which care will be delivered. As an example, Fig. 1 represents a simple decision algorithm that can be enhanced with multidimensional monitoring including context variables.
The interpretation of a heart rate of 90 beats per minute is dependent on the clinical context. Typically, this heart rate would be considered normal and no alert would be generated. However, if a patient has a heart rate of 90 in the context of acute myocardial ischemia, suboptimal heart rate control is present and an alert may be desired.
5 Alerting delivery methods
Traditional surveillance and astute clinicians will always play a critical role in the accurate diagnosis of a clinical syndrome [47]. Several factors like workload, economics and unit culture can influence alarm response. Once the decision support system generates an alert, it can be delivered to care providers in various ways (e.g. terminal displays, audio and/or visual cues in nursing stations or the EMR, e-mail, wireless pager messages). Automated wireless pager systems are becoming a popular method for delivering patient-related information quickly to medical decision makers [48]. Pagers linked to clinical information systems can provide real-time clinical event notifications to clinicians [49]. For example, the surgical ICU physicians at Cedars-Sinai are automatically notified about critical laboratory values as soon as the information is entered into the computerized patient record [50]. However, as was discussed above, such solutions may contribute to information overload and “alarm fatigue”.
An alternative solution would be to develop task-specific user interfaces that prioritize high impact information and alerts [51, 52]. Such interfaces will be a key component of EMRs of the future. Ambient intelligence in a broad sense is any technology that has the capacity to respond to changing contexts, intelligently assisting humans in the completion of a desired task. A great example of ambient intelligence is consumer portable GPS systems. Used as a navigation device, a GPS will consistently deliver the right information to the right person at the right time and help a user make good decisions in unfamiliar surroundings. For medicine, this approach is around the corner with future integration of data feeds from clinical devices and components of the EMR.
6 Plan for action
6.1 Rigorous research and development is required to improve current alarm and rule-based DSS
-
Identifying clinically insignificant true positive alerts—eliminate “noise”.
-
Determine actionable alarm conditions—prioritize “meaningful alerts”.
-
Address alarm fatigue using a cognitive sciences approach.
-
Develop and validate digital signatures of complex conditions—identify “high priority information”.
-
Identifying the mode of alert delivery through an understanding of workflow and health care delivery models—deliver information the right way, to the right person, in support of the best care possible.
-
Education—health care providers need to understand the limitations and strengths of new decision support tools.
-
Incentivize commercial partners to work with clinicians to develop interconnected devices which deliver meaningful improvements in patient outcomes.
EMRs should serve as real-time tools that supports a more systematic approach to patient care. Moreover, they should be developed to assist in diagnostic and therapeutic decision making rather than as a simple replacement for paper charts.
Comprehensive EMRs and computerized physician order entry systems serves as sources of information on patient health states and provider actions already available. Mobile technologies, allowing users to interact with information at the point of need, have been developed. The key missing ingredients are valid rules that connect the available technology to digital signatures of patient health states, provider responses, and a palette of appropriate actions for the observed circumstances. The development and testing of those rules present important intellectual challenges and opportunities for health care providers building the EMR of the future [53]. With full EMR integration, modern technology can bring true DSS to the bedside.
References
Power DJ. A brief history of decision support systems. Decis Support Syst. 2007;4(1969):1–18.
McDonald CJ. Protocol-based computer reminders, the quality of care and the non-perfectability of man. N Engl J Med. 1976;295(24):1351–5. doi:10.1056/NEJM197612092952405.
Manor-Shulman O, Beyene J, Frndova H, Parshuram CS. Quantifying the volume of documented clinical information in critical illness. J Crit Care. 2008;23(2):245–50. doi:10.1016/j.jcrc.2007.06.003.
Chambrin MC, Ravaux P, Calvelo-Aros D, Jaborska A, Chopin C, Boniface B. Multicentric study of monitoring alarms in the adult intensive care unit (ICU): a descriptive analysis. Intensive Care Med. 1999;25(12):1360–6.
Byers JF, White SV. Patient safety: principles and practice. New York: Springer; 2004.
Tinker JH, Dull DL, Caplan RA, Ward RJ, Cheney FW. Role of monitoring devices in prevention of anesthetic mishaps: a closed claims analysis. Anesthesiology. 1989;71(4):541–6.
Rothschild JM, Landrigan CP, Cronin JW, Kaushal R, Lockley SW, Burdick E, Stone PH, Lilly CM, Katz JT, Czeisler CA, Bates DW. The critical care safety study: the incidence and nature of adverse events and serious medical errors in intensive care. Crit Care Med. 2005;33(8):1694–700.
Tsien CL, Fackler JC. Poor prognosis for existing monitors in the intensive care unit. Crit Care Med. 1997;25(4):614–9.
O’Carroll TM. Survey of alarms in an intensive therapy unit. Anaesthesia. 1986;41(7):742–4.
Lawless ST. Crying wolf: false alarms in a pediatric intensive care unit. Crit Care Med. 1994;22(6):981–5.
Schoenberg R, Sands DZ, Safran C. Making ICU alarms meaningful: a comparison of traditional versus trend-based algorithms. In: proceedings/AMIA Annual Symposium. 1999:379–383.
Graham KC, Cvach M. Monitor alarm fatigue: standardizing use of physiological monitors and decreasing nuisance alarms. Am J Crit Care. 2010;19(1):28–34. doi:10.4037/ajcc2010651. quiz 35.
Meredith C, Edworthy J. Are there too many alarms in the intensive care unit? An overview of the problems. J Adv Nurs. 1995;21(1):15–20.
Balogh D, Kittinger E, Benzer A, Hackl JM. Noise in the ICU. Intensive Care Med. 1993;19(6):343–6.
Kahn DM, Cook TE, Carlisle CC, Nelson DL, Kramer NR, Millman RP. Identification and modification of environmental noise in an ICU setting. Chest. 1998;114(2):535–40.
Little A, Ethier C, Ayas N, Thanachayanont T, Jiang D, Mehta S. A patient survey of sleep quality in the Intensive Care Unit. Minerva Anestesiol. 2012;78(4):406–14.
Institute of Medicine. To err is human. Building a safer health system. Washington: National Academy Press; 2000.
Norris PR, Dawant BM. Closing the loop in ICU decision support: physiologic event detection, alerts, and documentation. In: proceedings/AMIA Annual Symposium AMIA Symposium. 2001:498–502.
Shea S, Sideli RV, DuMouchel W, Pulver G, Arons RR, Clayton PD. Computer-generated informational messages directed to physicians: effect on length of hospital stay. J Am Med Inform Assoc. 1995;2(1):58–64.
Gorges M, Markewitz BA, Westenskow DR. Improving alarm performance in the medical intensive care unit using delays and clinical context. Anesth Analg. 2009;108(5):1546–52.
Arney D, Fischmeister S, Goldman JM, Lee I, Trausmuth R. Plug-and-play for medical devices: experiences from a case study. Biomed Instrum Technol. 2009;43(4):313–7. doi:10.2345/0899-8205-43.4.313.
Imhoff M, Kuhls S. Alarm algorithms in critical care monitoring. Anesth Analg. 2006;102(5):1525–37.
Milholland K. Patient data management systems (PDMS). Computer technology for critical care nurses. Comput Nurs. 1988;6(6):237–43.
Clemmer TP, Gardner RM. Data gathering, analysis, and display in critical care medicine. Respir Care. 1985;30(7):586–601.
Adhikari N, Lapinsky SE. Medical informatics in the intensive care unit: overview of technology assessment. J Crit Care. 2003;18(1):41–7. doi:10.1053/jcrc.2003.YJCRC9.
Sittig DF, Ash JS, Zhang J, Osheroff JA, Shabot MM. Lessons from “Unexpected increased mortality after implementation of a commercially sold computerized physician order entry system”. Pediatrics. 2006;118(2):797–801. doi:10.1542/peds.2005-3132.
Patel VL, Zhang J, Yoskowitz NA, Green R, Sayan OR. Translational cognition for decision support in critical care environments: a review. J Biomed Inform. 2008;41(3):413–31. doi:10.1016/j.jbi.2008.01.013.
Herasevich V, Pickering BW, Dong Y, Peters SG, Gajic O. Informatics infrastructure for syndrome surveillance, decision support, reporting, and modeling of critical illness. Mayo Clin Proc. 2010;85(3):247–54.
Chaudhry B, Wang J, Wu S, Maglione M, Mojica W, Roth E, Morton SC, Shekelle PG. Systematic review: impact of health information technology on quality, efficiency, and costs of medical care. Ann Intern Med. 2006;144(10):742–52.
Blumenthal D. Launching HITECH. N Eng J Med. 2010;362(5):382–5. doi:10.1056/NEJMp0912825.
Blumenthal D. Stimulating the adoption of health information technology. N Engl J Med. 2009;360(15):1477–9. doi:10.1056/NEJMp0901592.
Raschke RA, Gollihare B, Wunderlich TA, Guidry JR, Leibowitz AI, Peirce JC, Lemelson L, Heisler MA, Susong C. A computer alert system to prevent injury from adverse drug events: development and evaluation in a community teaching hospital. JAMA. 1998;280(15):1317–20.
Haug PJ, Gardner RM, Tate KE, Evans RS, East TD, Kuperman G, Pryor TA, Huff SM, Warner HR. Decision support in medicine: examples from the HELP system. Comput Biomed Res Int J. 1994;27(5):396–418.
Evans RS, Larsen RA, Burke JP, Gardner RM, Meier FA, Jacobson JA, Conti MT, Jacobson JT, Hulse RK. Computer surveillance of hospital-acquired infections and antibiotic use. JAMA. 1986;256(8):1007–11.
Mc Donald CJ. Use of a computer to detect and respond to clinical events: its effect on clinician behavior. Ann Intern Med. 1976;84(2):162–7.
Rivers E, Nguyen B, Havstad S, Ressler J, Muzzin A, Knoblich B, Peterson E, Tomlanovich M. Early goal-directed therapy in the treatment of severe sepsis and septic shock. N Engl J Med. 2001;345(19):1368–77.
Moorman JR, Lake DE, Griffin MP. Heart rate characteristics monitoring for neonatal sepsis. IEEE Trans Biomed Eng. 2006;53(1):126–32.
Mandl KD, Overhage JM, Wagner MM, Lober WB, Sebastiani P, Mostashari F, Pavlin JA, Gesteland PH, Treadwell T, Koski E, Hutwagner L, Buckeridge DL, Aller RD, Grannis S. Implementing syndromic surveillance: a practical guide informed by the early experience. J Am Med Inform Assoc. 2004;11(2):141–50.
Centers for Disease Control Prevention. Biological and chemical terrorism: strategic plan for preparedness and response. Recommendations of the CDC strategic planning workgroup. MMWR. 2000;49 (RR-4).
Herasevich V, Yilmaz M, Khan H, Hubmayr RD, Gajic O. Validation of an electronic surveillance system for acute lung injury. Intensive Care Med. 2009;35(6):1018–23.
Azzam HC, Khalsa SS, Urbani R, Shah CV, Christie JD, Lanken PN, Fuchs BD. Validation study of an automated electronic acute lung injury screening tool. JAMIA. 2009;16(4):503–8. doi:10.1197/jamia.M3120.
Koenig HC, Finkel BB, Khalsa SS, Lanken PN, Prasad M, Urbani R, Fuchs BD. Performance of an automated electronic acute lung injury screening system in intensive care unit patients. Crit Care Med. 2011;39(1):98–104. doi:10.1097/CCM.0b013e3181feb4a0.
Colpaert K, Hoste EA, Steurbaut K, Benoit D, Van Hoecke S, De Turck F, Decruyenaere J. Impact of real-time electronic alerting of acute kidney injury on therapeutic intervention and progression of RIFLE class. Crit Care Med. 2012;40(4):1164–70. doi:10.1097/CCM.0b013e3182387a6b.
Nelson JL, Smith BL, Jared JD, Younger JG. Prospective trial of real-time electronic surveillance to expedite early care of severe sepsis. Ann Emerg Med. 2011;57(5):500–4. doi:10.1016/j.annemergmed.2010.12.008.
Herasevich V, Afessa B, Chute CG, Gajic O. Designing and testing computer based screening engine for severe sepsis/septic shock. AMIA Annual Symposium proceedings/AMIA Symposium. 2008;966.
Herasevich V, Tsapenko M, Kojicic M, Ahmed A, Kashyap R, Venkata C, Shahjehan K, Thakur SJ, Pickering BW, Zhang J, Hubmayr RD, Gajic O. Limiting ventilator-induced lung injury through individual electronic medical record surveillance. Crit Care Med. 2011;39(1):34–9.
Mandl KD, Overhage JM, Wagner MM, Lober WB, Sebastiani P, Mostashari F, Pavlin JA, Gesteland PH, Treadwell T, Koski E, Hutwagner L, Buckeridge DL, Aller RD, Grannis S. Implementing syndromic surveillance: a practical guide informed by the early experience. JAMIA. 2004;11(2):141–50. doi:10.1197/jamia.M1356.
Reddy MC, Pratt W, McDonald DW, Shabot MM. Challenges to physicians’ use of a wireless alert pager. AMIA Annu Symp Proc. 2003:544–548.
Duncan RG, Shabot MM. Secure remote access to a clinical data repository using a wireless personal digital assistant (PDA). Proceedings/AMIA Annual Symposium. 2000:210–214.
Major K, Shabot MM, Cunneen S. Wireless clinical alerts and patient outcomes in the surgical intensive care unit. Am Surg. 2002;68(12):1057–60.
Zhu X, Lord W. Using a context-aware medical application to address information needs for extubation decisions. AMIA Annual Symposium proceedings/AMIA Symposium AMIA Symposium. 2005;1169.
Ahmed A, Chandra S, Herasevich V, Gajic O, Pickering BW. The effect of two different electronic health record user interfaces on intensive care provider task load, errors of cognition, and performance. Crit Care Med. 2011;39(7):1626–34. doi:10.1097/CCM.0b013e31821858a0.
Pickering BW, Litell JM, Herasevich V, Gajic O. Clinical review: the hospital of the future—building intelligent environments to facilitate safe and effective acute care delivery. Crit Care. 2012;16(2):220. doi:10.1186/cc11142.
Conflict of interest
The authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Herasevich, V., Kor, D.J., Subramanian, A. et al. Connecting the dots: rule-based decision support systems in the modern EMR era. J Clin Monit Comput 27, 443–448 (2013). https://doi.org/10.1007/s10877-013-9445-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10877-013-9445-6