Abstract
Background and Aims
Cronkhite–Canada syndrome (CCS) is a noninherited condition, associated with high morbidity, and characterized by gastrointestinal hamartomatous polyposis, alopecia, onychodystrophy, hyperpigmentation, and diarrhea. All features may respond to immunosuppressive therapy, but little is known about the etiology. An autoimmune origin has been suggested but not proved. From a retrospectively selected cohort, we evaluated clinicopathologic features, including immunostaining for IgG4 (an antibody associated with autoimmunity), and therapeutic outcomes in a cohort of CCS patients to provide further insights into this disease.
Methods
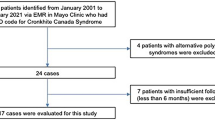
Cases included 14 consecutive CCS patients seen at the Mayo Clinic on whom tissue and follow-up were available. All histology was reviewed by an expert gastrointestinal pathologist. Immunostaining for IgG4 was performed on 42 polyps from CCS cases and on control tissues, including 46 histologically similar hamartomas [from juvenile polyposis syndrome (JPS)] and 20 normal mucosae (six stomach, three small bowel, and 11 colon). Clinical features and treatment outcomes were descriptive.
Results
All CCS cases had both upper and lower gastrointestinal polyps; most had typical dermatologic features of alopecia, hyperpigmentation, and onychodystrophy; and most had evidence of protein-losing enteropathy. Ten patients (71%) had adenomatous polyps and 2 (14%) had colorectal cancer. IgG4 immunostaining was positive (>5 cells/HPF) in 52% of CCS polyps compared to 12% of JPS polyps (P = 0.001); IgG4 staining was negative in all other control tissues. Of 11 CCS patients treated with oral corticosteroids, 91% achieved remission. Relapse was common with steroid tapering. Five patients who initially responded to corticosteroids were maintained in remission on azathioprine (2 mg/kg/day) with no relapse after a median of 4.5 years.
Conclusions
Immunostaining for the autoimmune-related IgG4 antibody is significantly increased in CCS polyps compared to disease and normal control tissues. Furthermore, immunosuppression by corticosteroids or long-term azathioprine may eradicate or lessen manifestations of CCS. These histologic findings and treatment responses are consistent with an autoimmune mechanism underlying CCS.


Similar content being viewed by others
Abbreviations
- CCS:
-
Cronkhite–Canada syndrome
- JPS:
-
Juvenile polyposis syndrome
- AIP:
-
Autoimmune pancreatitis
References
Cronkhite L, Canada W. Generalized gastrointestinal polyposis: An unusual syndrome of polyposis, pigmentation, alopecia, and onychotrophia. N Engl J Med. 1955;252:1011–1015.
Bacher T, Schonekas H, Steurer KT, Wunsch PH. The Cronkhite-Canada Syndrome. A rare differential diagnosis of generalized gastrointestinal polyposis. Dtsch Med Wochenschr. 1997;122:676–681.
Burnell RH. Cronkhite-Canada syndrome. Med J Aust. 1976;1:347–348.
Cotterill JA, Hughes JP, Day JL, Paulley JW, Turk E. The Cronkhite-Canada syndrome. Postgrad Med J. 1973;49:268–273.
Daniel ES, Ludwig SL, Lewin KJ, Ruprecht RM, Rajacich GM, Schwabe AD. The Cronkhite-Canada syndrome. An analysis of clinical and pathologic features and therapy in 55 patients. Medicine. 1982;61:293–309.
Freeman K, Anthony PP, Miller DS, Warin AP. Cronkhite-Canada syndrome. J R Soc Med. 1984;77:4–5.
Goto A. Cronkhite-Canada syndrome: Epidemiological study of 110 cases reported in Japan. Nihon Geka Hokan. 1995;64:3–14.
Nishiki M, Takasugi S, Kanao M, Okumichi T, Tamura T, Ezaki H. Cronkhite-Canada syndrome. A case report and analytical review of 37 other cases reported in Japan. Hiroshima J Med Sci. 1984;33:607–614.
Lipper S, Kahn LB. Superficial cystic gastritis with alopecia. A forme fruste of the Cronkhite-Canada syndrome. Arch Pathol Lab Med. 1977;101:432–436.
Boardman L. Hereditable colon cancer syndromes: Recognition and prevention management. Gastroenterol Clin North Am. 2002;31:1107–1131.
Schreibman I, Baker M, Amos C, McGarrity T. The hamartomatous polyposis syndromes: A clinical and molecular review. Am J Gastroenterol. 2005;100:476–490.
Burke AP, Sobin LH. The pathology of Cronkhite-Canada polyps. A comparison to juvenile polyposis. Am J Surg Pathol. 1989;13:940–946.
Chadalavada R, Brown DK, Walker AN, Sedghi S. Cronkhite-Canada syndrome: Sustained remission after corticosteroid treatment. Am J Gastroenterol. 2003;98:1444–1446.
Doyle T, Jarvis R. Reversal of changes in Cronkhite-Canada syndrome. Australas Radiol. 1984;28:19–22.
Goto A. Cronkhite-Canada syndrome: Observations about treatment, course and prognosis of 123 cases reported in Japan. Nihon Geka Hokan. 1988;57:427–433.
Lin HJ, Tsai YT, Lee SD, et al. The Cronkhite-Canada syndrome with a focus on immunity and infection, report of a case. J Clin Gastroenterol. 1987;9:560–570.
Takahashi H, Yamamoto M, Suzuki C, et al. The birthday of a new syndrome: IgG4-related diseases constitute a clinical entity. Autoimmun Rev. 2010;9:591–594.
Nishimori I, Otsuki M. Autoimmune pancreatitis and IgG4-associated sclerosing cholangitis. Best Pract Res Clin Gastroenterol. 2009;23:11–23.
Kim M-W, Moon S-H, Kamisawa T. Major duodenal papilla in autoimmune pancreatitis. Dig Surg. 2010;27:110–114.
Hamano H, Kawa S, Horiuchi A, et al. High serum IgG4 concentrations in patients with sclerosing pancreatitis. N Engl J Med. 2001;344:732–738.
Moon S-H, Kim M-H, Park DH, et al. Is a 2-week steroid trial after initial negative investigation for malignancy useful in differentiating autoimmune pancreatitis from pancreatic cancer? A prospective outcome study. Gut. 2008;57:1704–1712.
Hamano H, Kawa S, Uehara T, et al. Immunoglobulin G4-related lymphoplasmocytic sclerosing cholangitis that mimics infiltrating hilar cholangiocarcinoma: Part of a spectrum of autoimmune pancreatitis? Gastrointest Endosc. 2005;62:152–157.
Awazuhara H, Kawai H, Maruchi N. Major allergens in soybean and clinical significance of IgG4 antibodies investigated by IgE- and IgG4-immunoblotting with sera from soybean-sensitive patients. Clin Exp Allergy. 1997;27:325–332.
el Rafei A, Peters SM, Harris N, Bellanti JA. Diagnostic value of IgG4 measurements in patients with food allergy. Ann Allergy. 1989;62:94–99.
Zar S, Mincher L, Benson MJ, Kumar D. Food-specific IgG4 antibody-guided exclusion diet improves symptoms and rectal compliance in irritable bowel syndrome. Scand J Gastroenterol. 2005;40:800–807.
Nagata J, Kijima H, Hasumi K, Suzuki T, Shirai T, Mine T. Adenocarcinoma and multiple adenomas of the large intestine, associated with Cronkhite-Canada syndrome. Dig Liver Dis. 2003;35:434–438.
Nonomura A, Ohta G, Ibata T, Shinozaki K, Nishino T. Cronkhite-Canada syndrome associated with sigmoid cancer case report and review of 54 cases with the syndrome. Acta Pathol Jpn. 1980;30:825–845.
Katayama Y, Kimura M, Konn M. Cronkhite-Canada syndrome associated with a rectal cancer and adenomatous changes in colonic polyps. Am J Surg Pathol. 1985;9:65–71.
Malhotra R, Sheffield A. Cronkhite-Canada syndrome associated with colon carcinoma and adenomatous changes in C–C polyps. Am J Gastroenterol. 1988;83:772–776.
Jain A, Nanda S, Chakraborty P, et al. Cronkhite-Canada syndrome with adenomatous and carcinomatous transformation of colonic polyp. Indian J Gastroenterol. 2003;22:189–190.
Kaneko Y, Kato H, Tachimori Y, et al. Triple carcinomas in Cronkhite-Canada syndrome. Jpn J Clin Oncol. 1991;21:194–202.
Murai N, Fukuzaki T, Nakamura T, et al. Cronkhite-Canada syndrome associated with colon cancer: Report of a case. Surg Today. 1993;23:825–829.
Watanabe T, Kudo M, Shirane H, et al. Cronkhite-Canada syndrome associated with triple gastric cancers: A case report. Gastrointest Endosc. 1999;50:688–691.
Yamaguchi K, Ogata Y, Akagi Y, et al. Cronkhite-Canada syndrome associated with advanced rectal cancer treated by a subtotal colectomy: Report of a case. Surg Today. 2001;31:521–526.
Zugel NP, Hehl JA, Jechart G, Tannapfel A, Wienbeck M, Witte J. Colorectal carcinoma in Cronkhite-Canada syndrome. Z Gastroenterol. 2001;39:365–367.
Radha Krishna Y, Ghoshal UC, Pandey R, et al. Cronkhite-Canada syndrome with Adenomatous polyposis. J Postgrad Med. 2008;54:144–146.
Nakatsubo N, Wakasa R, Kiyosaki K, et al. Cronkhite-Canada syndrome associated with carcinoma of the sigmoid colon: Report of a Case. Jpn J Surg. 1997;27:345–348.
Yashiro M, Kobayashi H, Kubo N, Nishiguchi Y, Wakasa K, Hirakawa K. Cronkhite-Canada syndrome containing colon cancer and serrated adenoma lesions. Digestion. 2004;69:57–62.
Misra SP, Misra V, Dwivedi M, Singh PA, Gupta SC. Cronkhite–Canada syndrome without colonic polyps. Endoscopy. 1997;29:333.
Naitoh H, Eimoto T, Kamachi H. An autopsy case of Cronkhite-Canada syndrome develo** after hemicolectomy for colonic cancer. Gan No Rinsho. 1986;32:1619–1624.
van der Zee JS, van Swieten P, Aalberse RC. Inhibition of complement activation by IgG4 antibodies. Clin Exp Immunol. 1986;64:415–422.
Takeuchi Y, Yoshikawa M, Tsukamoto N, et al. Cronkhite-Canada syndrome with colon cancer, portal vein thrombosis, high titer of antinuclear antibodies, and membranous glomerulonephritis. J Gastroenterol. 2003;38:791–795.
Kamisawa T, Shimosegawa T, Okazaki K, et al. Standard steroid treatment for autoimmune pancreatitis. Gut. 2009;58:1504–1507.
Chari ST, Smyrk TC, Levy MJ, et al. Diagnosis of autoimmune pancreatitis: The Mayo Clinic experience. Clin Gastroenterol Hepatol. 2006;4:1010–1016.
Pannala R, Chari ST. Corticosteroid treatment for autoimmune pancreatitis. Gut. 2009;58:1438–1439.
Conflict of interest
No conflicts of interest exist.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Sweetser, S., Ahlquist, D.A., Osborn, N.K. et al. Clinicopathologic Features and Treatment Outcomes in Cronkhite–Canada Syndrome: Support for Autoimmunity. Dig Dis Sci 57, 496–502 (2012). https://doi.org/10.1007/s10620-011-1874-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10620-011-1874-9