Abstract
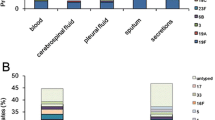
Streptococcus pneumoniae, Haemophilus influenzae, and Mycoplasma pneumoniae are the main pathogens causing community-acquired pneumonia (CAP). We identified S. pneumoniae (n = 241), H. influenzae (n = 123), and M. pneumoniae (n = 54) as causative pathogens from clinical findings and blood tests from pediatric CAP patients (n = 903) between April 2008 and April 2009. Identification of genes mediating antimicrobial resistance by real-time PCR was performed for all isolates of these three pathogens, as was antibiotic susceptibility testing using an agar dilution method or broth microdilution method. The genotypic (g) resistance rate was 47.7 % for penicillin-resistant S. pneumoniae (gPRSP) possessing abnormal pbp1a, pbp2x, and pbp2b genes, 62.6 % for β-lactamase-nonproducing, ampicillin-resistant (gBLNAR) H. influenzae possessing the amino acid substitutions Ser385Thr and Asn526Lys, and 44.4 % for macrolide-resistant M. pneumoniae (gMRMP) possessing a mutation of A2063G, A2064G, or C2617A. Serotype 6B (20.3 %) predominated in S. pneumoniae, followed by 19F (15.4 %), 14 (14.5 %), 23F (12.0 %), 19A (6.2 %), and 6C (5.4 %). Coverage for the isolates by heptavalent pneumococcal conjugate vaccine (PCV7) and PCV13, respectively, was calculated as 68.5 and 80.9 %. A small number of H. influenzae were identified as type b (6.5 %), type e (0.8 %), or type f (0.8 %); all others were nontypeable. Proper use of antibiotics based on information about resistance in CAP pathogens is required to control rapid increases in resistance. Epidemiological surveillance of pediatric patients also is needed to assess the effectiveness of PCV7 and Hib vaccines after their introduction in Japan.





Similar content being viewed by others
References
Don M, Canciani M, Korppi M. Community-acquired pneumonia in children: what’s old? What’s new? Acta Paediatr. 2010;99:1602–8.
Honkinen M, Lahti E, Österback R, Ruuskanen O, Waris M. Viruses and bacteria in sputum samples of children with community-acquired pneumonia. Clin Microbiol Infect. 2012;18:300–7.
Juvén T, Mertsola J, Waris M, Leinonen M, Meurman O, Roivainen M, et al. Etiology of community-acquired pneumonia in 254 hospitalized children. Pediatr Infect Dis J. 2000;19:293–8.
MaIntosh K. Community-acquired pneumonia in children. N Engl J Med. 2002;346:429–37.
Okada T, Morozumi M, Sakata H, Takayanagi R, Ishiwada N, Sato Y, et al. A practical approach estimating etiologic agents using real-time PCR in pediatric inpatients with community-acquired pneumonia. J Infect Chemother. 2012;. doi:10.1007/s10156-012-0422.
Sinaniotis CA, Sinaniotis AC. Community-acquired pneumonia in children. Curr Opin Pulm Med. 2005;11:218–25.
Chetty K, Thomson AH. Management of community-acquired pneumonia in children. Paediatr Drugs. 2007;9:401–11.
Chiba N, Morozumi M, Ubukata K. Application of the real-time PCR method for genotypic identification of β-lactam resistance in isolates from invasive pneumococcal diseases. Microb Drug Resist. 2012;18:149–56.
Esposito S, Cohen R, Domingo JD, Pecurariu OF, Greenberg D, Heininger U, et al. Antibiotic therapy for pediatric community-acquired pneumonia: do we know when, what and for how long to treat? Pediatr Infect Dis J. 2012;31:78–85.
Kishii K, Chiba N, Morozumi M, Hamano-Hasegawa K, Kurokawa I, Masaki J, et al. Diverse mutations in the ftsI gene in ampicillin-resistant Haemophilus influenzae isolates from pediatric patients with acute otitis media. J Infect Chemother. 2010;16:87–93.
Morozumi M, Takahashi T, Ubukata K. Macrolide-resistant Mycoplasma pneumoniae: characteristics of isolates and clinical aspects of community-acquired pneumonia. J Infect Chemother. 2010;16:78–86.
Bogaert D, De Groot R, Hermans PW. Streptococcus pneumoniae colonisation: the key to pneumococcal disease. Lancet Infect Dis. 2004;4:144–54.
Jourdain S, Smeesters PR, Denis O, Dramaix M, Sputael V, Malaviolle X, et al. Differences in nasopharyngeal bacterial carriage in preschool children from different socio-economic origins. Clin Microbiol Infect. 2011;17:907–14.
Murphy TF, Faden H, Bakaletz LO, Kyd JM, Forsgren A, Campos J, et al. Nontypeable Haemophilus influenzae as a pathogen in children. Pediatr Infect Dis J. 2009;28:43–8.
Hamano-Hasegawa K, Morozumi M, Nakayama E, Chiba N, Murayama SY, Takayanagi R, et al. Comprehensive detection of causative pathogens using real-time PCR to diagnose pediatric community-acquired pneumonia. J Infect Chemother. 2008;14:424–32.
Morozumi M, Nakayama E, Iwata S, Aoki Y, Hasegawa K, Kobayashi R, et al. Simultaneous detection of pathogens in clinical samples from patients with community-acquired pneumonia by real-time PCR with pathogen-specific molecular beacon probes. J Clin Microbiol. 2006;44:1440–6.
Kishii K, Morozumi M, Chiba N, Ono A, Ubukata K. Direct detection by real-time PCR of ftsI gene mutations affecting MICs of β-lactam agents for Haemophilus influenzae isolates from meningitis. J Infect Chemother. 2011;17:671–7.
Morozumi M, Hasegawa K, Kobayashi R, Inoue N, Iwata S, Kuroki H, et al. Emergence of macrolide-resistant Mycoplasma pneumoniae with a 23S rRNA gene mutation. Antimicrob Agents Chemother. 2005;49:2302–6.
Clinical and Laboratory Standards Institute. Performance standards for antimicrobial susceptibility testing: 18th informational supplement. CLSI document M100-S18. Wayne, PA: CLSI; 2008
Ubukata K, Chiba N, Hasegawa K, Shibasaki Y, Sunakawa K, Nonoyama M, et al. Differentiation of beta-lactamase-negative ampicillin-resistant Haemophilus influenzae from other H. influenzae strains by a disc method. J Infect Chemother. 2002;8:50–8.
Chiba N, Kobayashi R, Hasegawa K, Morozumi M, Nakayama E, Tajima T, et al. Antibiotic susceptibility according to genotype of penicillin-binding protein and macrolide resistance genes, and serotype of Streptococcus pneumoniae isolates from community-acquired pneumonia in children. J Antimicrob Chemother. 2005;56:756–60.
Ubukata K, Shibasaki Y, Yamamoto K, Chiba N, Hasegawa K, Takeuchi Y, Sunakawa K, Inoue M, Konno M. Association of amino acid substitutions in penicillin-binding protein 3 with beta-lactam resistance in beta-lactamase-negative ampicillin-resistant Haemophilus influenzae. Antimicrob Agents Chemother. 2001;45:1693–9.
Witherden EA, Montgomery J, Henderson B, Tristram SG. Prevalence and genotypic characteristics of beta-lactamase-negative ampicillin-resistant Haemophilus influenzae in Australia. J Antimicrob Chemother. 2011;66:1013–5.
Pilishvili T, Lexau C, Farley MM, Hadler J, Harrison LH, Bennett NM, et al. Sustained reductions in invasive pneumococcal disease in the era of conjugate vaccine. J Infect Dis. 2010;201:32–41.
Isaacman DJ, McIntosh ED, Reinert RR. Burden of invasive pneumococcal disease and serotype distribution among Streptococcus pneumoniae isolates in young children in Europe: impact of the 7-valent pneumococcal conjugate vaccine and considerations for future conjugate vaccines. Int J Infect Dis. 2010;14:197–209.
Ubukata K, Chiba N, Morozumi M, Iwata S, Sunakawa K, and the Working Group of nationwide Surveillance for Bacterial Meningitis. Longitudinal surveillance of Haemophilus influenzae isolates from pediatric patients with meningitis throughout Japan, 2000 to 2011. J Infect Chemother. doi:10.1007/s10156-012-0448-x.
Chang A, Kaur R, Michel LV, Casey JR, Pichichero M. Haemophilus influenzae vaccine candidate outer membrane protein P6 is not conserved in all strains. Hum Vaccin. 2011;7:102–5.
Noda K, Kodama S, Umemoto S, Nomi N, Hirano T, Suzuki M. Th17 cells contribute to nontypeable Haemophilus influenzae-specific protective immunity induced by nasal vaccination with P6 outer membrane protein and α-galactosylceramide. Microbiol Immunol. 2011;55:574–81.
Okada T, Morozumi M, Tajima T, Hasegawa M, Sakata H, Ohnari S, et al. Rapid effectiveness of minocycline or doxycycline against macrolide-resistant Mycoplasma pneumoniae infection in a 2011 outbreak among Japanese children. Clin Infect Dis. doi:10.1093/cid/cis784.
Uehara S, Sunakawa K, Eguchi H, Ouchi K, Okada K, Kurosaki T, et al. Japanese guidelines for the management of respiratory infectious diseases in children 2007 with focus on pneumonia. Pediatr Int. 2011;53:264–76.
Acknowledgments
We thank the members of the Acute Respiratory Diseases Study Group: Drs. Takeshi Tajima and Eiichi Nakayama (Hakujikai Memorial Hospital), Reiko Takayanagi, Shinobu Ishizawa, Mika Numata, and Michiyo Kojima (Tohoku Rosai Hospital), Naohisa Kawamura and Koichi Shimizu (Osaka Rosai Hospital), Naruhiko Ishiwada and Junko Tanaka (Chiba University Hospital), Yoshitake Sato (Health Insurance Society of General Ota Hospital, Fuji Heavy Industries Ltd.), Kazunobu Ouchi (Kawasaki Medical School Hospital), Tsunekazu Haruta and Takuya Tamura (Kobe City Medical Center General Hospital), and Tomohiro Oishi (Niigata University Medical and Dental Hospital). This study was supported in part by a grant under the category “Research on Emerging and Re-emerging Infectious Diseases” (numbers H21-002 and H22-013) from the Japanese Ministry of Health, Labour and Welfare (to K. Ubukata).
Author information
Authors and Affiliations
Corresponding author
About this article
Cite this article
Morozumi, M., Chiba, N., Okada, T. et al. Antibiotic susceptibility in relation to genotype of Streptococcus pneumoniae, Haemophilus influenzae, and Mycoplasma pneumoniae responsible for community-acquired pneumonia in children. J Infect Chemother 19, 432–440 (2013). https://doi.org/10.1007/s10156-012-0500-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10156-012-0500-x