Abstract
Purpose
Nonoperative management (NOM) has been widely accepted as one of the standard treatments for patients with acute appendicitis. However, predictive factors for the failure of NOM have not been thoroughly investigated.
Methods
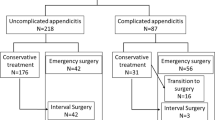
A total of 196 patients with acute appendicitis underwent NOM between April 2014 and December 2020. Of these 196 patients, 24 patients failed NOM and required emergency surgery (failure group: n = 24), while the other 172 patients were successfully treated with NOM (success group: n = 172). These two groups were compared, and the predictive factors for the failure of NOM were investigated.
Results
The number of patients who had a previous history of stroke was significantly increased in the failure group (12.5% vs. 2.9%, p = 0.026). Incarceration of an appendicolith on CT images was significantly associated with the failure group (20.8% vs. 1.7%, p < 0.001), while neither the presence of an appendicolith nor abscess was associated. The presence of periappendiceal fluid was significantly associated with the failure group (50.0% vs. 26.7%, p = 0.019). The incarceration of an appendicolith (p < 0.001, odds ratio = 19.85) and periappendiceal fluid (p = 0.009, odds ratio = 3.62) were found to be independent risk factors for failure of NOM. Neither the presence of an appendicolith nor abscess was associated with the recurrence of appendicitis.
Conclusions
The presence of an appendicolith or abscess was not a crucial factor for surgery. Incarceration of an appendicolith and periappendiceal fluid on CT images was predictive factors for the failure of NOM.



Similar content being viewed by others
Data availability
Not applicable.
Code availability
Not applicable.
References
Di Saverio S, Podda M, De Simone B et al (2020) Diagnosis and treatment of acute appendicitis: 2020 update of the WSES Jerusalem guidelines. World J Emerg Surg 15:27. https://doi.org/10.1186/s13017-020-00306-3
Sallinen V, Akl EA, You JJ et al (2016) Meta-analysis of antibiotics versus appendicectomy for nonperforated acute appendicitis. Br J Surg 103:656–667. https://doi.org/10.1002/bjs.10147
Harnoss JC, Zelienka I, Probst P et al (2017) Antibiotics versus surgical therapy for uncomplicated appendicitis: systematic review and meta-analysis of controlled trials (PROSPERO 2015: CRD42015016882). Ann Surg 265:889–900. https://doi.org/10.1097/SLA.0000000000002039
Podda M, Gerardi C, Cillara N et al (2019) Antibiotic treatment and appendectomy for uncomplicated acute appendicitis in adults and children: a systematic review and meta-analysis. Ann Surg 270:1028–1040. https://doi.org/10.1097/SLA.0000000000003225
Huang L, Yin Y, Yang L, Wang C, Li Y, Zhou Z (2017) Comparison of antibiotic therapy and appendectomy for acute uncomplicated appendicitis in children: a meta-analysis. JAMA Pediatr 171:426–434. https://doi.org/10.1001/jamapediatrics.2017.0057
Gorter RR, The SML, Gorter-Stam MAW et al (2017) Systematic review of nonoperative versus operative treatment of uncomplicated appendicitis. J Pediatr Surg 52:1219–1227. https://doi.org/10.1016/j.jpedsurg.2017.04.005
Georgiou R, Eaton S, Stanton MP, Pierro A, Hall NJ (2017) Efficacy and safety of nonoperative treatment for acute appendicitis: a meta-analysis. Pediatrics 139:e20163003. https://doi.org/10.1542/peds.2016-3003
Maita S, Andersson B, Svensson JF, Wester T (2020) Nonoperative treatment for nonperforated appendicitis in children: a systematic review and meta-analysis. Pediatr Surg Int 36:261–269. https://doi.org/10.1007/s00383-019-04610-1
Simillis C, Symeonides P, Shorthouse AJ, Tekkis PP (2010) A meta-analysis comparing conservative treatment versus acute appendectomy for complicated appendicitis (abscess or phlegmon). Surgery 147:818–829. https://doi.org/10.1016/j.surg.2009.11.013
Yang Z, Sun F, Ai S, Wang J, Guan W, Liu S (2019) Meta-analysis of studies comparing conservative treatment with antibiotics and appendectomy for acute appendicitis in the adult. BMC Surg 19:110. https://doi.org/10.1186/s12893-019-0578-5
Fugazzola P, Coccolini F, Tomasoni M, Stella M, Ansaloni L (2019) Early appendectomy vs. conservative management in complicated acute appendicitis in children: a meta-analysis. J Pediatr Surg 54:2234–2241. https://doi.org/10.1016/j.jpedsurg.2019.01.065
van Amstel P, Sluckin TC, van Amstel T et al (2020) Management of appendiceal mass and abscess in children; early appendectomy or initial nonoperative treatment? A systematic review and meta-analysis. Surg Endosc 34:5234–5249. https://doi.org/10.1007/s00464-020-07822-y
Aprahamian CJ, Barnhart DC, Bledsoe SE, Vaid Y, Harmon CM (2007) Failure in the nonoperative management of pediatric ruptured appendicitis: predictors and consequences. J Pediatr Surg 42:934–8. https://doi.org/10.1016/j.jpedsurg.2007.01.024 (discussion 938)
Mahida JB, Lodwick DL, Nacion KM et al (2016) High failure rate of nonoperative management of acute appendicitis with an appendicolith in children. J Pediatr Surg 51:908–911. https://doi.org/10.1016/j.jpedsurg.2016.02.056
Fuhrer AE, Sukhotnik I, Ben-Shahar Y, Weinberg M, Koppelmann T (2021) Predictive value of Alvarado score and pediatric appendicitis score in the success of nonoperative management for simple acute appendicitis in children. Eur J Pediatr Surg 31:95–101. https://doi.org/10.1055/s-0040-1718406
Talishinskiy T, Limberg J, Ginsburg H, Kuenzler K, Fisher J, Tomita S (2016) Factors associated with failure of nonoperative treatment of complicated appendicitis in children. J Pediatr Surg 51:1174–1176. https://doi.org/10.1016/j.jpedsurg.2016.01.006
Maxfield MW, Schuster KM, Bokhari J, McGillicuddy EA, Davis KA (2014) Predictive factors for failure of nonoperative management in perforated appendicitis. J Trauma Acute Care Surg 76:976–981. https://doi.org/10.1097/TA.0000000000000187
Walker C, Moosavi A, Young K et al (2019) Factors associated with failure of nonoperative management for complicated appendicitis. Am Surg 85:865–870
Collaborative CODA, Flum DR, Davidson GH et al (2020) A randomized trial comparing antibiotics with appendectomy for appendicitis. N Engl J Med 383:1907–1919. https://doi.org/10.1056/NEJMoa2014320
Ishiyama M, Yanase F, Taketa T et al (2013) Significance of size and location of appendicoliths as exacerbating factor of acute appendicitis. Emerg Radiol 20:125–130. https://doi.org/10.1007/s10140-012-1093-5
Shekarriz S, Keck T, Kujath P et al (2019) Comparison of conservative versus surgical therapy for acute appendicitis with abscess in five German hospitals. Int J Colorectal Dis 34:649–655. https://doi.org/10.1007/s00384-019-03238-w
Tekin A, Kurtoğlu HC, Can I, Oztan S (2008) Routine interval appendectomy is unnecessary after conservative treatment of appendiceal mass. Colorectal Dis 10:465–468. https://doi.org/10.1111/j.1463-1318.2007.01377.x
Mällinen J, Rautio T, Grönroos J et al (2019) Risk of appendiceal neoplasm in periappendicular abscess in patients treated with interval appendectomy vs follow-up with magnetic resonance imaging: 1-year outcomes of the peri-appendicitis acuta randomized clinical trial. JAMA Surg 154:200–207. https://doi.org/10.1001/jamasurg.2018.4373
Author information
Authors and Affiliations
Contributions
A.K. wrote the manuscript and performed data analysis. All authors contributed to acquire data and revise the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Kohga, A., Kawabe, A., Yajima, K. et al. Does the presence of an appendicolith or abscess predict failure of nonoperative management of patients with acute appendicitis?. Emerg Radiol 28, 977–983 (2021). https://doi.org/10.1007/s10140-021-01951-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10140-021-01951-0