Abstract
Purpose
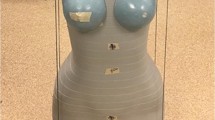
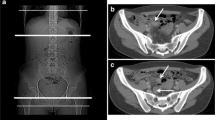
The purpose of this study was to determine if CT for appendicitis can be abbreviated to begin at the top of the L2 vertebral body level and still maintain the detection rate of appendicitis and other symptomatic pathology without omitting significant incidental findings.
Methods
Retrospective review of CT abdomen-pelvis exams for suspected appendicitis over a 5-month period was performed. The Z-axis scan length of the original full scans and theoretical limited scans from the top of L2 were recorded and calculated. Images were reviewed for incidental findings above the L2 vertebral body level and categorized by severity per American College of Radiology (ACR) white paper guidelines. Final diagnoses based on imaging findings were also recorded.
Results
One hundred nineteen patients (46 males, 73 females, mean age 29 ± 14) were included. Appendicitis was present in 26 cases (22%). Using a theoretical scan beginning at the top of the L2 vertebral body, none of the findings leading to diagnosis of appendicitis would have been missed. A total of 30 incidental findings were found above the L2 vertebral body. Per ACR white paper guidelines, 26 of these findings did not require additional imaging follow-up. Additional follow-up imaging was recommended for 3 of the findings above L2, and 1 right adrenal metastasis was found above L2 in a patient with previously undiagnosed NSCLC. This patient coincidentally also had appendicitis. No symptomatic pathology would have been missed had the scans begun at the top of the L2 vertebral body. Such an abbreviated scan would have resulted in a mean Z-axis reduction of 12.9 cm (30.3%).
Conclusions
CT using abbreviated Z-axis scan length can reduce radiation dose and provide necessary imaging needed to diagnose appendicitis or other symptomatic pathology without omitting significant incidental findings.


Similar content being viewed by others
References
Doria AS, Moineddin R, Kellenberger CJ, Epelman M, Beyene J, Schuh S, Babyn PS, Dick PT (2006) US or CT for diagnosis of appendicitis in children and adults? A meta-analysis. Radiology 241(1):83–94. doi:10.1148/radiol.2411050913
Kim K, Rhee JE, Lee CC, Kim KS, Shin JH, Kwak MJ, Kim JH, Suh GJ, Hahn SK, Singer AJ (2008) Impact of helical computed tomography in clinically evident appendicitis. Emerg Med J 25(8):477–481. doi:10.1136/emj.2006.044552
Tsao K, St Peter SD, Valusek PA, Spilde TL, Keckler SJ, Nair A, Ostlie DJ, Holcomb GW 3rd (2008) Management of pediatric acute appendicitis in the computed tomographic era. J Surg Res 147(2):221–224. doi:10.1016/j.jss.2008.03.004
Smith MP, Katz DS, Lalani T, Carucci LR, Cash BD, Kim DH, Piorkowski RJ, Small WC, Spottswood SE, Tulchinsky M, Yaghmai V, Yee J, Rosen MP (2015) ACR Appropriateness Criteria(R) right lower quadrant pain—suspected appendicitis. Ultrasound Q 31(2):85–91. doi:10.1097/RUQ.0000000000000118
Raman SS, Lu DS, Kadell BM, Vodopich DJ, Sayre J, Cryer H (2002) Accuracy of nonfocused helical CT for the diagnosis of acute appendicitis: a 5-year review. AJR Am J Roentgenol 178(6):1319–1325. doi:10.2214/ajr.178.6.1781319
Pickhardt PJ, Lawrence EM, Pooler BD, Bruce RJ (2011) Diagnostic performance of multidetector computed tomography for suspected acute appendicitis. Ann Intern Med 154(12):789–796, W-291. doi:10.7326/0003-4819-154-12-201106210-00006
Pooler BD, Lawrence EM, Pickhardt PJ (2012) Alternative diagnoses to suspected appendicitis at CT. Radiology 265(3):733–742. doi:10.1148/radiol.12120614
Addiss DG, Shaffer N, Fowler BS, Tauxe RV (1990) The epidemiology of appendicitis and appendectomy in the United States. Am J Epidemiol 132(5):910–925
Kim K, Kim YH, Kim SY, Kim S, Lee YJ, Kim KP, Lee HS, Ahn S, Kim T, Hwang SS, Song KJ, Kang SB, Kim DW, Park SH, Lee KH (2012) Low-dose abdominal CT for evaluating suspected appendicitis. N Engl J Med 366(17):1596–1605. doi:10.1056/NEJMoa1110734
Kim SY, Lee KH, Kim K, Kim TY, Lee HS, Hwang SS, Song KJ, Kang HS, Kim YH, Rhee JE (2011) Acute appendicitis in young adults: low- versus standard-radiation-dose contrast-enhanced abdominal CT for diagnosis. Radiology 260(2):437–445. doi:10.1148/radiol.11102247
Seo H, Lee KH, Kim HJ, Kim K, Kang SB, Kim SY, Kim YH (2009) Diagnosis of acute appendicitis with sliding slab ray-sum interpretation of low-dose unenhanced CT and standard-dose iv contrast-enhanced CT scans. AJR Am J Roentgenol 193(1):96–105. doi:10.2214/AJR.08.1237
van der Molen AJ, Geleijns J (2007) Overranging in multisection CT: quantification and relative contribution to dose--comparison of four 16-section CT scanners. Radiology 242(1):208–216. doi:10.1148/radiol.2421051350
McCollough CH (2008) CT dose: how to measure, how to reduce. Health Phys 95(5):508–517. doi:10.1097/01.HP.0000326343.35884.03
Fefferman NR, Roche KJ, Pinkney LP, Ambrosino MM, Genieser NB (2001) Suspected appendicitis in children: focused CT technique for evaluation. Radiology 220(3):691–695. doi:10.1148/radiol.2203001826
Rao PM, Rhea JT, Novelline RA, McCabe CJ, Lawrason JN, Berger DL, Sacknoff R (1997) Helical CT technique for the diagnosis of appendicitis: prospective evaluation of a focused appendix CT examination. Radiology 202(1):139–144. doi:10.1148/radiology.202.1.8988203
Kamel IR, Goldberg SN, Keogan MT, Rosen MP, Raptopoulos V (2000) Right lower quadrant pain and suspected appendicitis: nonfocused appendiceal CT—review of 100 cases. Radiology 217(1):159–163. doi:10.1148/radiology.217.1.r00oc34159
de Leon AD, ** Y, Champine J, Costa DN (2014) Achieving ideal computed tomographic scan length in patient with suspected urolithiasis. J Comput Assist Tomogr 38(2):264–267. doi:10.1097/RCT.0000000000000016
Corwin MT, Bekele W, Lamba R (2014) Bony landmarks on computed tomographic localizer radiographs to prescribe a reduced scan range in patients undergoing multidetector computed tomography for suspected urolithiasis. J Comput Assist Tomogr 38(3):404–407. doi:10.1097/RCT.0b013e3182ab5f35
Corwin MT, Chang M, Fananapazir G, Seibert A, Lamba R (2015) Accuracy and radiation dose reduction of a limited abdominopelvic CT in the diagnosis of acute appendicitis. Abdom Imaging 40(5):1177–1182. doi:10.1007/s00261-014-0280-0
Berland LL, Silverman SG, Gore RM, Mayo-Smith WW, Megibow AJ, Yee J, Brink JA, Baker ME, Federle MP, Foley WD, Francis IR, Herts BR, Israel GM, Krinsky G, Platt JF, Shuman WP, Taylor AJ (2010) Managing incidental findings on abdominal CT: white paper of the ACR incidental findings committee. J Am Coll Radiol 7(10):754–773. doi:10.1016/j.jacr.2010.06.013
Heller MT, Harisinghani M, Neitlich JD, Yeghiayan P, Berland LL (2013) Managing incidental findings on abdominal and pelvic CT and MRI, part 3: white paper of the ACR Incidental Findings Committee II on splenic and nodal findings. J Am Coll Radiol 10(11):833–839. doi:10.1016/j.jacr.2013.05.020
Harish MG, Konda SD, MacMahon H, Newstead GM (2007) Breast lesions incidentally detected with CT: what the general radiologist needs to know. Radiographics 27(Suppl 1):S37–S51. doi:10.1148/rg.27si075510
Bendeck SE, Nino-Murcia M, Berry GJ, Jeffrey RB Jr (2002) Imaging for suspected appendicitis: negative appendectomy and perforation rates. Radiology 225(1):131–136. doi:10.1148/radiol.2251011780
Malone AJ Jr, Wolf CR, Malmed AS, Melliere BF (1993) Diagnosis of acute appendicitis: value of unenhanced CT. AJR Am J Roentgenol 160(4):763–766. doi:10.2214/ajr.160.4.8456661
Federle MP (1997) Focused appendix CT technique: a commentary. Radiology 202(1):20–21. doi:10.1148/radiology.202.1.8988184
Song JH, Chaudhry FS, Mayo-Smith WW (2008) The incidental adrenal mass on CT: prevalence of adrenal disease in 1,049 consecutive adrenal masses in patients with no known malignancy. AJR Am J Roentgenol 190(5):1163–1168. doi:10.2214/AJR.07.2799
Ozao-Choy J, Kim U, Vieux U, Menes TS (2011) Incidental findings on computed tomography scans for acute appendicitis: prevalence, costs, and outcome. Am Surg 77(11):1502–1509
Furtado CD, Aguirre DA, Sirlin CB, Dang D, Stamato SK, Lee P, Sani F, Brown MA, Levin DL, Casola G (2005) Whole-body CT screening: spectrum of findings and recommendations in 1192 patients. Radiology 237(2):385–394. doi:10.1148/radiol.2372041741
Author information
Authors and Affiliations
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Patel, D.C., Huang, Yh., Meyer, J. et al. Abdominal-pelvic scanning parameters revisited: a case for Z-axis reduction in patients with clinical suspicion for acute appendicitis. Emerg Radiol 24, 661–666 (2017). https://doi.org/10.1007/s10140-017-1539-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10140-017-1539-x