Abstract
Background
Nonalcoholic fatty liver disease (NAFLD) refers to hepatic steatosis caused by something other than alcoholic liver injury, and often occurs after gastrointestinal surgeries such as pancreatoduodenectomy and gastrectomy. This study aimed to identify the risk factors for NAFLD after gastrectomy for gastric cancer.
Methods
A total of 721 patients who underwent gastrectomy for gastric cancer and plane abdominal computed tomography (CT) preoperatively and 1 year after surgery were included in this study. NAFLD was defined as having a mean hepatic CT attenuation value of < 40 Hounsfield units. We retrospectively examined the relationship between the onset of NAFLD and clinicopathological findings to identify the risk factors associated with the development of NAFLD after gastrectomy.
Results
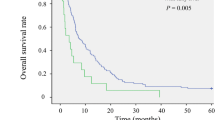
The incidence of postoperative NAFLD was 4.85% (35/721). The univariate analysis identified the following factors as being significantly associated with the incidence of NAFLD: age, preoperative BMI ≥ 25 kg/m2, tumor depth of pT3 ≤, lymph node metastasis grade of pN2 ≤, cholecystectomy, D2 lymphadenectomy, adjuvant chemotherapy, high preoperative cholinesterase serum level, and low grade of preoperative FIB-4 index. Adjuvant chemotherapy (p < 0.001) and high preoperative cholinesterase serum level (p = 0.021) were identified as independent risk factors for NAFLD 1 year after gastrectomy.
Conclusion
Our study showed that adjuvant chemotherapy with S-1 and high level of serum cholinesterase were considered as the risk factors for NAFLD occurring after gastrectomy for gastric cancer.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Nonalcoholic fatty liver disease (NAFLD) refers to hepatic steatosis caused by something other than alcoholic liver injury, and the prevalence of NAFLD is increasing worldwide [1]. NAFLD is associated with other metabolic diseases, including type 2 diabetes mellitus and dyslipidemia, and is also one of the most common causes of chronic liver disorders and can lead to liver cirrhosis or hepatocellular carcinoma [2,3,4].
Several recent studies have also shown that NAFLD is a late postoperative complication of pancreatoduodenectomy [5]. It has been reported that NAFLD after pancreatoduodenectomy is mainly associated with malnutrition and pancreatic exocrine deficiency [6]. Gastrectomy is a procedure that can also cause postoperative weight loss and nutritional deficiencies, similar to pancreatoduodenectomy. However, to our knowledge, no clinical studies have investigated the association between postoperative NAFLD and gastrectomy for gastric cancer. The purpose of this study was to identify the risk factors for NAFLD after gastrectomy for gastric cancer.
Materials and methods
Patients
Of the 804 consecutive patients who underwent gastrectomy for gastric cancer at National Defense Medical College (Saitama, Japan) between January 2007 and December 2014, we analyzed the results of 721 patients. The exclusion criteria were as follows: (1) a history of any types of hepatitis virus infection, (2) a history of autoimmune hepatitis, (3) a history of alcohol abuse, (4) the evidence of fatty liver on CT images before operation, (5) BMI 30 kg/m2 ≤, and (6) a lack of plane abdominal computed tomography (CT) scans taken before operation and/or 1 year after operation. Alcohol abuse was defined as consuming > 30 g of alcohol per day for males and > 20 g of alcohol per day for females.
Patients’ clinical records at the operation and pathological records were retrospectively evaluated for age, sex, body mass index (BMI), a history of diabetes mellitus, tumor depth, lymph node metastasis, pathological cancer stage, operation procedure, lymphadenectomy, reconstruction, post-operation infectious complications, neoadjuvant chemotherapy (NAC), adjuvant chemotherapy, and pancreatic enzyme administration. Patients’ pathological findings were recorded in accordance with the third English edition of the Japanese Classification of Gastric Carcinoma, which was edited by the Japanese Gastric Cancer Association [7]. Additionally, perioperative serum markers of nutrition and liver function, including total protein, albumin, total bilirubin, aspartate transaminase (AST), alanine transaminase (ALT), cholinesterase, total cholesterol, triglyceride levels, and FIB-4 index as well as any perioperative changes in terms of indicator level, were analyzed.
Our study included 555 males and 166 females with a mean age of 68.4 years old. Out of 721 patients, 35 (4.9%) developed NAFLD 1 year after gastrectomy (NAFLD group) and 686 (95.2%) patients did not (non-NAFLD group).
Operative procedure
We performed gastrectomy with lymphadenectomy for patients with gastric cancer in accordance with the Japanese gastric cancer treatment guidelines. After 2009, we introduced laparoscopic gastrectomy (laparoscopic distal gastrectomy, total gastrectomy, proximal gastrectomy, and pylorus-preserving gastrectomy) for selected patients with gastric cancer.
Perioperative management
All patients were followed up with an oncologically appropriate plan. We prescribed NAC drugs to gastric cancer patients with advanced lymph node metastasis and to patients in which radial resection might be difficult. We mainly used S-1 (80 mg/m2/day) and cisplatin (60 mg/m2) for NAC. For stage II or III patients, postoperative adjuvant chemotherapy with S-1 (80 mg/m2/day) for 1 year was recommended. The patients were recommended to stop drinking from being diagnosed as having gastric cancer to 1 year after gastrectomy.
Evaluation of hepatic CT attenuation values
Unenhanced CT images were obtained via the single-breath-hold technique using a 64 multidetector CT scanner (Aquilion 64; Toshiba Medical Systems, Tokyo, Japan). All patients underwent unenhanced CT before the operation for the preoperative diagnosis of gastric cancer and 1 year after the operation for a postoperative follow-up observation. The average CT attenuation values of five arbitrary regions of the liver parenchyma without vessels were measured, and each region of interest was a circular area with a diameter of 20 mm (Fig. 1). In this study, NAFLD was defined as having a hepatic CT attenuation value of < 40 Hounsfield units in reference to the previous report [8]. These were evaluated retrospectively by a physician who was blinded to complaints, specific medical history, and findings of physical examination, surgery, laboratory evaluation, and imaging.
Statistical analysis
All statistical analyses were performed using the JMP Pro 14.0.0 software package (SAS Institute Inc, Cary, NC, USA). Student’s t test and Pearson’s Chi square test were performed, as appropriate.
Univariate and multivariate analyses were performed using the Cox proportional hazards regression model. The data are expressed as the mean ± standard deviation. A p value of < 0.05 was considered statistically significant.
Results
Patients’ characteristics and demographic data are shown in Table 1. There was no statistically significant difference in age, sex, diabetes mellitus history, surgical procedure, infectious complications after operation, and the incidence of NAC between NAFLD and non-NAFLD groups. The NAFLD group had significantly higher preoperative and postoperative (at 1 year after operation) BMI, deeper tumor depth, and higher grade of lymph node metastasis than the non-NAFLD group (p = 0.001, p = 0.009, p = 0.013, and p = 0.014, respectively). There was no significant difference in surgical approach such as open or laparoscopic surgery between the two groups. However, Billroth-I type reconstruction (42.9%), the D2 lymphadenectomy (74.3%) and resection of gallbladder (34.3%) were performed more frequently in the NAFLD group than the non-NAFLD group (24.9%, 47.3% and 15.6%, respectively). When patients were limited to distal gastrectomy, Billroth-I type reconstruction was performed in 13 cases (56.5%) in the NAFLD group and in 168 cases (53.0%) in the non-NAFLD group, and there was no significant difference in the development of NAFLD between the two groups. Although 105 cases were administered pancreatic enzymes after surgery at the discretion of the surgeon, there was no significant difference in the presence or absence of administration of pancreatic enzymes between the two groups. Although NAC did not affect the onset of NAFLD, the NAFLD group more frequently received adjuvant chemotherapy than the non-NAFLD group (p < 0.001). Next, we examined the clinicopathological characteristics which might affect the postoperative NAFLD in patients who underwent total gastrectomy (Supplemental Table 1). NAFLD occurred at a high rate in patients with adjuvant chemotherapy, cholecystectomy, and high BMI.
There were no significant perioperative changes in the levels of total protein, albumin, AST, ALT, total cholesterol, and triglyceride in both two groups (Table 2). As for liver function, the NAFLD group had higher postoperative total bilirubin levels, higher preoperative cholinesterase levels, and a larger increase in total bilirubin serum levels as compared to the non-NAFLD group. In addition, NAFLD group had a lower level of preoperative FIB-4 index. At 6 months after surgery, there were no significant differences in the AST and ALT levels, and FIB-4 index between the two groups (data not shown). Cholecystectomy did not affect the results of these liver function tests (data not shown).
Our univariate analysis identified the following factors as being significantly associated with the incidence of NAFLD: age (p = 0.003), preoperative BMI ≥ 25 kg/m2 (p = 0.005), tumor depth of pT3 ≤ (p = 0.016), lymph node metastasis grade of pN2 ≤ (p = 0.017), cholecystectomy (p = 0.005), D2 lymphadenectomy (p = 0.014), adjuvant chemotherapy (p < 0.001), high preoperative cholinesterase serum level (p = 0.029), and low grade of preoperative FIB-4 index (p < 0.001) (Table 3). The multivariate analysis of these nine factors identified adjuvant chemotherapy (p < 0.001) and high preoperative cholinesterase serum level (p = 0.021) as independent risk factors for NAFLD 1 year after gastrectomy.
Discussion
In our present study, the incidence of NAFLD after gastrectomy for gastric cancer was 5.4%. This incidence rate was lower than that associated with pancreatoduodenectomy, which is reported to be 8–40% [9]. Several studies reported that NAFLD after pancreatoduodenectomy was mainly associated with insufficient pancreatic exocrine levels caused by decrease in pancreatic volume, and could be prevented by the administration of pancreatic enzyme [5, 6, 10]. Although patients who have undergone gastrectomy suffered from weight loss and malnutrition like after pancreatoduodenectomy, to the best of our knowledge, no study has reported regarding the incidence of NAFLD after gastrectomy. In this study, we demonstrated that the administration of adjuvant chemotherapy with S-1 and high serum level of preoperative cholinesterase were independent risk factors for the development of NAFLD 1 year after gastrectomy. Billroth-I type reconstruction was identified as a risk factor for the onset of NAFLD by univariate analysis. However, when the cases were limited to distal gastrectomy, there was no significant difference in the onset of NAFLD between Billroth-I type reconstruction and other reconstruction methods (data not shown).
S-1 is an oral anticancer preparation composed of a mixture of tegafur [a prodrug of 5-fluorouracil (5-FU)], 5-chloro-2,4-dihydroxypyridine (a biochemical modulator that inhibits 5-FU biodegradation) and potassium oxonate (added to reduce the gastrointestinal toxicity of 5-FU) [11, 12]. Based on the results of randomized prospective controlled study conducted by the Japan Clinical Oncology group (JCOG), adjuvant chemotherapy with S-1 for stage II/III gastric cancer is effective and it is suggested that this therapy should be adopted as the standard treatment following curative D2 gastric dissection [13]. It is well known that 5-FU causes hepatic steatosis [14, 15]. There were reports that 34.9% of patients developed NAFLD after receiving adjuvant chemotherapy with 5-FU-containing regimens in colorectal cancer [16]. Laurent et al. reported that 5-FU induces oxidative stress in both cancer cells and normal cells [17]. Oxidative stress is known to cause mitochondrial abnormalities in hepatocytes, which play a role in fatty acid degradation, leading to fat accumulation in the liver and oxidative stress by 5-FU can explain that 5-FU induces NAFLD [18, 19]. Thus, it is reasonable that 5-FU derived from S-1 may cause NAFLD, and that patients with a more advanced stage of disease who were administered S-1 as adjuvant chemotherapy more frequently developed NAFLD.
After gastrectomy, not only the physiological food digestion process in the stomach is impaired, but also the absorption disorders are caused by various disappearances such as the absence of gastric acid and pepsin, decreased secretion of gastrointestinal hormones, and exocrine pancreatic disorders [20]. Although our present study showed that NAFLD group showed high preoperative cholinesterase, no significant difference was found in postoperative nutritional indicators between two groups. This suggests that perioperative nutritional deterioration does not significantly affect the development of NAFLD after gastrectomy. In our study with patients who underwent total gastrectomy, only adjuvant chemotherapy, high BMI, and cholecystectomy were selected as risk factors of NAFLD by multivariate analysis.
It is not surprising that NAFLD is strongly associated with obesity. It is reported that obese patients have prevalence of NAFLD as high as 80% and higher BMI was confirmed as the most useful predictive factor for onset of NAFLD [21]. Recent studies suggest that insulin resistance is involved in the pathogenesis of NAFLD, and patients with high BMI have a high frequency of multiple co-morbidities and are often insulin resistant. In this study, the reduction of BMI associated with gastrectomy did not influence the onset of NAFLD. Patients with high preoperative BMI were considered to be prone to NAFLD development by 5-FU oxidative stress.
NAFLD generally signifies overnutrition, but postoperative NAFLD has different clinical features. Since the incidence of post-pancreatoduodenectomy digestion dysfunctions, including delayed gastric emptying and pancreatic function decline, is high, surgeons often establish a nutritional route, commonly via jejunostomy. However, it is uncommon to perform jejunostomy after gastrectomy for gastric cancer treatment as complications, including leakage, tend to cause long-term nutritional decline. However, the association between post-gastrectomy complications and the incidence of NAFLD was not obvious in this study. It is reported that the patients who received pancreatic enzyme had a lesser rate of NAFLD compared with patients who did not receive pancreatic enzymes [22]. On the other hand, in our study, administration of pancreatic enzyme did not reduce the incidence of NAFLD. Several reports mentioned that NAFLD is more likely to occur, as the small remnant pancreatic volume after pancreatic resection is smaller [9, 10]. Pancreatic enzyme affects the recovery of pancreatic exocrine capacity and administration of pancreatic enzyme itself would be not involved in the onset of NAFLD. Thus, pancreatic enzyme did not contribute to the reduction of the incidence of NAFLD after gastrectomy.
FIB-4 index is a simple marker for liver fibrosis, which can be calculated only from age, AST, ALT, and platelet count, and is a parameter that has better discrimination ability in differentiation of stage 3 or a higher stage of fibrosis compared to other scores [23]. In this study, the lower the preoperative FIB-4 index score is, the higher the incidence of postoperative NAFLD will be. This result was probably related to the fact that the patients in the non-NAFLD group were significantly older than the patients in the NAFLD group. There was no correlation between the incidence of NAFLD and FIB-4 index at the time of onset of NAFLD and perioperative changes in FIB-4 index, suggesting that the preoperative degree of liver fibrosis did not affect the development of NAFLD after gastrectomy.
In this study, although there was no association between the presence or absence of pancreatic resection and NAFLD, it was suggested that the presence of cholecystectomy may be a risk of develo** NAFLD. Nervi et al. showed that cholecystectomy is associated with NAFLD using data from the Third United States National Health and Nutrition Examination Survey in their study [24]. They suggested bile acids in systemic metabolic regulation may be the key to develo** NAFLD after cholecystectomy.
The limitations of this study include the lack of a control group for statistical analysis due to the retrospective nature of our study, the relatively small number of people who developed NAFLD, and that the study was only conducted at a single center. In addition, histological assessment of liver fibrosis by liver biopsy was not performed.
In conclusion, our study showed that adjuvant chemotherapy with S-1 and high serum level of preoperative cholinesterase were considered as the risk factors for NAFLD occurring after gastrectomy for gastric cancer. Further study regarding the use of other adjuvant chemotherapies to prevent NAFLD development during gastrectomy is required to ensure the safety of gastric cancer patients during treatment.
References
Vernon G, Baranova A, Younossi ZM. Systematic review: the epidemiology and natural history of non-alcoholic fatty liver disease and non-alcoholic steatohepatitis in adults. Aliment Pharmacol Ther. 2011;34(3):274–85.
Caldwell SH, Crespo DM. The spectrum expanded: cryptogenic cirrhosis and the natural history of non-alcoholic fatty liver disease. J Hepatol. 2004;40(4):578–84.
Younossi ZM, Koenig AB, Abdelatif D, Fazel Y, Henry L, Wymer M. Global epidemiology of nonalcoholic fatty liver disease-meta-analytic assessment of prevalence, incidence, and outcomes. Hepatology (Baltimore, MD). 2016;64(1):73–84.
Sanna C, Rosso C, Marietti M, Bugianesi E. Non-alcoholic fatty liver disease and extra-hepatic cancers. Int J Mol Sci. 2016;17(5):717.
Nishikawa M, Aosasa S, Moriya T, Noro T, Hase K, Yamamoto J. The impact of postoperative adjuvant chemotherapy on the development of nonalcoholic fatty liver disease after pancreatoduodenectomy. J Surg Res. 2016;205(1):127–35.
Nakagawa N, Murakami Y, Uemura K, Sudo T, Hashimoto Y, Kondo N, et al. Nonalcoholic fatty liver disease after pancreatoduodenectomy is closely associated with postoperative pancreatic exocrine insufficiency. J Surg Oncol. 2014;110(6):720–6.
Japanese Gastric Cancer Association. Japanese gastric cancer treatment guidelines 2014 (ver 4). Gastric Cancer. 2017;20(1):1–19.
Boyce CJ, Pickhardt PJ, Kim DH, Taylor AJ, Winter TC, Bruce RJ, et al. Hepatic steatosis (fatty liver disease) in asymptomatic adults identified by unenhanced low-dose CT. Am J Roentgenol. 2010;194(3):623–8.
Kato H, Isaji S, Azumi Y, Kishiwada M, Hamada T, Mizuno S, et al. Development of nonalcoholic fatty liver disease (NAFLD) and nonalcoholic steatohepatitis (NASH) after pancreaticoduodenectomy: proposal of a postoperative NAFLD scoring system. J Hepatobiliary Pancreat Sci. 2010;17(3):296–304.
Sato R, Kishiwada M, Kuriyama N, Azumi Y, Mizuno S, Usui M, et al. Paradoxical impact of the remnant pancreatic volume and infectious complications on the development of nonalcoholic fatty liver disease after pancreaticoduodenectomy. J Hepatobiliary Pancreat Sci. 2014;21(8):562–72.
Shirasaka T, Shimamato Y, Ohshimo H, Yamaguchi M, Kato T, Yonekura K, et al. Development of a novel form of an oral 5-fluorouracil derivative (S-1) directed to the potentiation of the tumor selective cytotoxicity of 5-fluorouracil by two biochemical modulators. Anticancer Drugs. 1996;7(5):548–57.
Tatsumi K, Fukushima M, Shirasaka T, Fujii S. Inhibitory effects of pyrimidine, barbituric acid and pyridine derivatives on 5-fluorouracil degradation in rat liver extracts. Jp J Cancer Res. 1987;78(7):748–55.
Sakuramoto S, Sasako M, Yamaguchi T, Kinoshita T, Fujii M, Nashimoto A, et al. Adjuvant chemotherapy for gastric cancer with S-1, an oral fluoropyrimidine. N Engl J Med. 2007;357(18):1810–20.
Peppercorn PD, Reznek RH, Wilson P, Slevin ML, Gupta RK. Demonstration of hepatic steatosis by computerized tomography in patients receiving 5-fluorouracil-based therapy for advanced colorectal cancer. Br J Cancer. 1998;77(11):2008–11.
Sorensen P, Edal AL, Madsen EL, Fenger C, Poulsen MR, Petersen OF. Reversible hepatic steatosis in patients treated with interferon alfa-2a and 5-fluorouracil. Cancer. 1995;75(10):2592–6.
Miyake K, Hayakawa K, Nishino M, Morimoto T, Mukaihara S. Effects of oral 5-fluorouracil drugs on hepatic fat content in patients with colon cancer. Aca Radiol. 2005;12(6):722–7.
Laurent A, Nicco C, Chereau C, Goulvestre C, Alexandre J, Alves A, et al. Controlling tumor growth by modulating endogenous production of reactive oxygen species. Cancer Res. 2005;65(3):948–56.
Tilg H, Moschen AR. Evolution of inflammation in nonalcoholic fatty liver disease: the multiple parallel hits hypothesis. Hepatology (Baltimore, MD). 2010;52(5):1836–46.
Zorzi D, Laurent A, Pawlik TM, Lauwers GY, Vauthey JN, Abdalla EK. Chemotherapy-associated hepatotoxicity and surgery for colorectal liver metastases. Br J Surg. 2007;94(3):274–86.
Huddy JR, Macharg FMS, Lawn AM, Preston SR. Exocrine pancreatic insufficiency following esophagectomy. Dis Esophagus. 2013;26(6):594–7.
Williams CD, Stengel J, Asike MI, Torres DM, Shaw J, Contreras M, et al. Prevalence of nonalcoholic fatty liver disease and nonalcoholic steatohepatitis among a largely middle-aged population utilizing ultrasound and liver biopsy: a prospective study. Gastroenterology.
Sato T, Matsuo Y, Shiga K, Morimoto M, Miyai H, Takeyama H. Factors that predict the occurrence of and recovery from non-alcoholic fatty liver disease after pancreatoduodenectomy. Surgery. 2016;160(2):318–30.
Shah AG, Lydecker A, Murray K, Tetri BN, Contos MJ, Sanyal AJ. Comparison of noninvasive markers of fibrosis in patients with nonalcoholic fatty liver disease. Clin Gastroenterol Hepatol. 2009;7(10):1104–12.
Nervi F, Arrese M. Cholecystectomy and NAFLD: does gallbladder removal have metabolic consequences? Am J Gastroenterol. 2013;108(6):959–61.
Funding
All authors certify that they have no commercial associations that might pose a conflict of interest in connection with the submitted article.
Author information
Authors and Affiliations
Contributions
KK, MN and HT contributed to study conception and design. KK, TS, HN and MN contributed to acquisition of data. KK and HT contributed to analysis and interpretation of data. KK and HT contributed to drafting of the article. MH, SH, YY, RT, SN, NI, YI, ST, KH, YK and HU contributed to critical revision of the article.
Corresponding author
Ethics declarations
Ethical approval
All procedures followed were in accordance with the Helsinki Declaration of 1964 and later versions. The study protocol was approved by the Institutional Review Board of the National Defense Medical College.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Kouzu, K., Tsujimoto, H., Nishikawa, M. et al. Risk factors for nonalcoholic fatty liver disease after gastrectomy for gastric cancer. Gastric Cancer 23, 356–362 (2020). https://doi.org/10.1007/s10120-019-01009-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10120-019-01009-8