Abstract
Background/purpose
Adequate control of disease activity in rheumatoid arthritis (RA) depends, to a great extent, on the access to a rheumatologist. This study aimed to compare the disease outcomes of patients with RA, based on their healthcare regime affiliation.
Methods
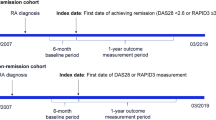
A retrospective observational study of Colombian patients with RA in three outpatient services of different regimes: Contributory (CR, workers and their families with a monthly income above a yearly defined threshold, approximately US$ 220, who allocate a percentage of their income to financing the national health fund and to get access to healthcare services), subsidized (SR, a vulnerable population with a monthly income below the threshold, who have access to healthcare through the national health fund; comparable to the USA Medicaid population), and an excellence clinical care center (C3, access to specialized care, regardless of their healthcare affiliation regime). Data were collected from clinical records for 2 years of follow-up and included demographics, lag times between appointments, and time in high disease activity. We used the Mantel-Cox test for the analysis of time to remission/low disease activity.
Results
A total of 240 patients were included (80 patients per regime). At the start of follow-up, mean age was 53.7 years; 21.6% of patients were men; 79.6% of patients had established RA; 72.9% of patients had high disease activity. Patients in the CR had longer lag times between scheduled appointments (p < 0.0001). During follow-up, SR had the highest proportion of patients with high disease activity. Survival curve analysis showed no significant difference between SR and CR groups (p = 0.2903), but was significantly different compared with the C3 group (p < 0.0001). Median survival in high disease activity was greater in the SR group (293 days), followed by CR (254 days), and finally by C3 (64 days).
Conclusion
Patients that were treated in the excellence clinical care center had better outcomes when compared with other regimes. These data support that healthcare regime may influence disease outcome in patients with RA.
Key Points • Prompt access to healthcare in patients with rheumatoid arthritis is pivotal for an adequate control of the disease, for timely adjustment of treatment, and to reduce both the societal burden of the disease and its impact on individual well-being. • As an example of “structural iatrogenesis,” healthcare regime affiliation appears to influence disease outcomes in patients with rheumatoid arthritis, in whom differences between regimes are observed. The most vulnerable patients appear to experience the worst outcomes. • Excellence clinical care centers for patients with rheumatoid arthritis should be implemented as an alternative to counteract structural healthcare barriers and as an approach to improve clinical outcomes through a tighter disease control. |

Similar content being viewed by others
Data availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Smolen JS, Aletaha D, Barton A, Burmester GR, Emery P, Firestein GS, Kavanaugh A, McInnes IB, Solomon DH, Strand V, Yamamoto K (2018) Rheumatoid arthritis. Nat Rev Dis Prim 4:18001. https://doi.org/10.1038/nrdp.2018.1
Londoño J, Peláez Ballestas I, Cuervo F, Angarita I, Giraldo R, Rueda JC, Ballesteros JG, Baquero R, Forero E, Cardiel M, Saldarriaga E, Vásquez A, Arias S, Valero L, González C, Ramírez J, Toro C, Santos AM (2018) Prevalence of rheumatic disease in Colombia according to the Colombian Rheumatology Association (COPCORD) strategy. Prevalence study of rheumatic disease in Colombian population older than 18 years. Rev Colomb Reumatol 25:245–256. https://doi.org/10.1016/j.rcreu.2018.08.003
Fernández-Ávila DG, Rincón-Riaño DN, Bernal-Macías S, Gutiérrez Dávila JM, Rosselli D (2019) Prevalence of rheumatoid arthritis in Colombia based on information from the Ministry of Health registry. Rev Colomb Reumatol 26:83–87. https://doi.org/10.1016/j.rcreu.2019.01.003
Díaz-Rojas JA, Dávila-Ramírez FA, Quintana-López G, Aristizábal-Gutiérrez F, Brown P (2016) Rheumatoid arthritis prevalence in Colombia: an approach based on burden of disease study during 2005. Rev Colomb Reumatol 23:11–16. https://doi.org/10.1016/j.rcreu.2015.12.004
Singh JA, Saag KG, Bridges SL et al (2016) 2015 American College of Rheumatology Guideline for the treatment of rheumatoid arthritis. Arthritis Care Res 68:1–25. https://doi.org/10.1002/acr.22783
Smolen JS, Landewé RBM, Bijlsma JWJ, Burmester GR, Dougados M, Kerschbaumer A, McInnes IB, Sepriano A, van Vollenhoven RF, de Wit M, Aletaha D, Aringer M, Askling J, Balsa A, Boers M, den Broeder AA, Buch MH, Buttgereit F, Caporali R, Cardiel MH, de Cock D, Codreanu C, Cutolo M, Edwards CJ, van Eijk-Hustings Y, Emery P, Finckh A, Gossec L, Gottenberg JE, Hetland ML, Huizinga TWJ, Koloumas M, Li Z, Mariette X, Müller-Ladner U, Mysler EF, da Silva JAP, Poór G, Pope JE, Rubbert-Roth A, Ruyssen-Witrand A, Saag KG, Strangfeld A, Takeuchi T, Voshaar M, Westhovens R, van der Heijde D (2020) EULAR recommendations for the management of rheumatoid arthritis with synthetic and biological disease-modifying antirheumatic drugs: 2019 update. Ann Rheum Dis 79:685–699. https://doi.org/10.1136/annrheumdis-2019-216655
Verstappen SMM (2017) The impact of socio-economic status in rheumatoid arthritis. Rheumatology (Oxford) 56:1051–1052. https://doi.org/10.1093/rheumatology/kew428
(2015) Health and health care in Colombia. In: OECD Reviews of Health Systems: Colombia 2016. OECD, pp 37–72
Giedion U, Uribe MV (2009) Colombia’s universal health insurance system. Health Aff (Millwood) 28:853–863. https://doi.org/10.1377/hlthaff.28.3.853
Ministerio de Salud y Protección Social (2020) Cifras de aseguramiento en salud. https://www.minsalud.gov.co/proteccionsocial/Paginas/cifras-aseguramiento-salud.aspx
de Vries E, Uribe C, Pardo C, Lemmens V, van de Poel E, Forman D (2015) Gastric cancer survival and affiliation to health insurance in a middle-income setting. Cancer Epidemiol 39:91–96. https://doi.org/10.1016/j.canep.2014.10.012
Santos-Moreno P, Caballero-Uribe CV, Cardiel MH, Galarza-Maldonado C, Massardo L, Pineda C, Soriano E, Castro CA, Villarreal L, Buitrago D (2019) A consensus position paper from REAL-PANLAR Group about the methodological approach for the accreditation process of centers of excellence in rheumatoid arthritis in Latin America. J Clin Rheumatol 25:54–58. https://doi.org/10.1097/RHU.0000000000000773
Ministerio de Salud y Protección Social (2014) Guía de práctica clínica para la detección temprana, diagnóstico y tratamiento de la artritis reumatoide
England BR, Tiong BK, Bergman MJ, Curtis JR, Kazi S, Mikuls TR, O'Dell JR, Ranganath VK, Limanni A, Suter LG, Michaud K (2019) 2019 update of the American College of Rheumatology recommended rheumatoid arthritis disease activity measures. Arthritis Care Res 71:1540–1555. https://doi.org/10.1002/acr.24042
Smolen JS, Landewé R, Bijlsma J, Burmester G, Chatzidionysiou K, Dougados M, Nam J, Ramiro S, Voshaar M, van Vollenhoven R, Aletaha D, Aringer M, Boers M, Buckley CD, Buttgereit F, Bykerk V, Cardiel M, Combe B, Cutolo M, van Eijk-Hustings Y, Emery P, Finckh A, Gabay C, Gomez-Reino J, Gossec L, Gottenberg JE, Hazes JMW, Huizinga T, Jani M, Karateev D, Kouloumas M, Kvien T, Li Z, Mariette X, McInnes I, Mysler E, Nash P, Pavelka K, Poór G, Richez C, van Riel P, Rubbert-Roth A, Saag K, da Silva J, Stamm T, Takeuchi T, Westhovens R, de Wit M, van der Heijde D (2017) EULAR recommendations for the management of rheumatoid arthritis with synthetic and biological disease-modifying antirheumatic drugs: 2016 update. Ann Rheum Dis 76:960–977. https://doi.org/10.1136/annrheumdis-2016-210715
Tsuji H, Yano K, Furu M, Yamakawa N, Ikari K, Hashimoto M, Ito H, Fujii T, Yamamoto W, Ohmura K, Taniguchi A, Momohara S, Matsuda F, Allaart CF, Yamanaka H, Mimori T, Terao C (2017) Time-averaged disease activity fits better joint destruction in rheumatoid arthritis. Sci Rep 7:5856. https://doi.org/10.1038/s41598-017-05581-w
Navarro-Compán V, Gherghe AM, Smolen JS et al (2015) Relationship between disease activity indices and their individual components and radiographic progression in RA: a systematic literature review. Rheumatology (Oxford) 54:994–1007. https://doi.org/10.1093/rheumatology/keu413
Grigor C, Capell H, Stirling A, McMahon AD, Lock P, Vallance R, Porter D, Kincaid W (2004) Effect of a treatment strategy of tight control for rheumatoid arthritis (the TICORA study): a single-blind randomised controlled trial. Lancet 364:263–269. https://doi.org/10.1016/S0140-6736(04)16676-2
Rondón Sepulveda MA (2015) Sample size calculation. In: Ruiz-Morales A, Gómez-Restrepo C (eds) Clinical epidemiology: applied clinical research, 2nd edn. Panamericana, Bogota, Colombia, pp 76–90
Jones G, Sebba A, Gu J, Lowenstein MB, Calvo A, Gomez-Reino JJ, Siri DA, Tomšič M, Alecock E, Woodworth T, Genovese MC (2010) Comparison of tocilizumab monotherapy versus methotrexate monotherapy in patients with moderate to severe rheumatoid arthritis: the AMBITION study. Ann Rheum Dis 69:88–96. https://doi.org/10.1136/ard.2008.105197
Genovese MC, Bathon JM, Martin RW, Fleischmann RM, Tesser JR, Schiff MH, Keystone EC, Wasko MC, Moreland LW, Weaver AL, Markenson J, Cannon GW, Spencer-Green G, Finck BK (2002) Etanercept versus methotrexate in patients with early rheumatoid arthritis: two-year radiographic and clinical outcomes. Arthritis Rheum 46:1443–1450. https://doi.org/10.1002/art.10308
Versteeg GA, Steunebrink LMM, Vonkeman HE, ten Klooster PM, van der Bijl AE, van de Laar MAFJ (2018) Long-term disease and patient-reported outcomes of a continuous treat-to-target approach in patients with early rheumatoid arthritis in daily clinical practice. Clin Rheumatol 37:1189–1197. https://doi.org/10.1007/s10067-017-3962-5
de Andrade NPB, da Silva Chakr RM, Xavier RM, Viecceli D, Correa RHB, de Oliveira Filho CM, Brenol CV (2017) Long-term outcomes of treat-to-target strategy in established rheumatoid arthritis: a daily practice prospective cohort study. Rheumatol Int 37:993–997. https://doi.org/10.1007/s00296-017-3695-4
Tan BE, Lim AL, Kan SL, Lim CH, Ng YF, Tng SLC, Hassin NS, Chandran L, Hamid NA, Lee YYL (2017) Management of rheumatoid arthritis in clinical practice using treat-to-target strategy: where do we stand in the multi-ethnic Malaysia population? Rheumatol Int 37:905–913. https://doi.org/10.1007/s00296-017-3705-6
Santos-Moreno P, Alvis-Zakzuk NJ, Villarreal-Peralta L, Carrasquilla-Sotomayor M, Paternina-Caicedo A, Alvis-Guzmán N (2018) A comprehensive care program achieves high remission rates in rheumatoid arthritis in a middle-income setting. Experience of a Center of Excellence in Colombia. Rheumatol Int 38:499–505. https://doi.org/10.1007/s00296-017-3903-2
Bautista-Molano W, Fernández-Avila D, Jiménez R, Cardozo R, Marín A, Soler MP, Gómez O, Ruiz O (2016) Epidemiological profile of colombian patients with rheumatoid arthritis in a specialized care clinic. Reumatol Clin 12:313–318. https://doi.org/10.1016/j.reuma.2015.11.009
Machado-Alba JE, Ruiz AF, Medina Morales DA (2015) The epidemiology of rheumatoid arthritis in a cohort of Colombian patients. Rev Colomb Reumatol 22:148–152. https://doi.org/10.1016/j.rcreu.2015.05.006
Cardiel MH (2013) Estrategia «treat to target» en la artritis reumatoide: Beneficios reales. Reumatol Clin 9:101–105. https://doi.org/10.1016/j.reuma.2012.04.004
Arora S, Nika A, Trupin L, Abraham H, Block J, Sequeira W, Yazdany J, Jolly M (2018) Does systemic lupus erythematosus care provided in a lupus clinic result in higher quality of care than that provided in a general rheumatology clinic? Arthritis Care Res 70:1771–1777. https://doi.org/10.1002/acr.23569
Cifaldi M, Renaud J, Ganguli A, Halpern MT (2016) Disparities in care by insurance status for individuals with rheumatoid arthritis: analysis of the medical expenditure panel survey, 2006-2009. Curr Med Res Opin 32:2029–2037. https://doi.org/10.1080/03007995.2016.1227775
Minden SL, Hoaglin DC, Hadden L, Frankel D, Robbins T, Perloff J (2008) Access to and utilization of neurologists by people with multiple sclerosis. Neurology 70:1141–1149. https://doi.org/10.1212/01.wnl.0000306411.46934.ef
Arajo GTB, Caporale JE, Stefani S et al (2011) Is equity of access to health care achievable in Latin America? Value Health 14:8–12. https://doi.org/10.1016/j.jval.2011.05.037
Raza K, Stack R, Kumar K, Filer A, Detert J, Bastian H, Burmester GR, Sidiropoulos P, Kteniadaki E, Repa A, Saxne T, Turesson C, Mann H, Vencovsky J, Catrina A, Chatzidionysiou A, Hensvold A, Rantapää-Dahlqvist S, Binder A, Machold K, Kwiakowska B, Ciurea A, Tamborrini G, Kyburz D, Buckley CD (2011) Delays in assessment of patients with rheumatoid arthritis: variations across Europe. Ann Rheum Dis 70:1822–1825. https://doi.org/10.1136/ard.2011.151902
Rodríguez-Polanco E, Al Snih S, Kuo Y-F et al (2011) Lag time between onset of symptoms and diagnosis in Venezuelan patients with rheumatoid arthritis. Rheumatol Int 31:657–665. https://doi.org/10.1007/s00296-009-1358-9
Stonington S, Coffa D (2019) Structural iatrogenesis - a 43-year-old man with “opioid misuse”. N Engl J Med 380:701–704. https://doi.org/10.1056/NEJMp1811473
GEO-RA Group (2017) Latitude gradient influences the age of onset of rheumatoid arthritis: a worldwide survey. Clin Rheumatol 36(3):485–497. https://doi.org/10.1007/s10067-016-3481-9
Acknowledgments
We want to thank Dr. Cosmo Fowler, Dr. Alejandro De la Hoz, and Dr. Myriam Frydman for their time and insights on our manuscript.
Code availability
Not applicable.
Funding
This study was supported by a grant from the Colombian Association of Rheumatology.
Author information
Authors and Affiliations
Contributions
All authors contributed to the conception and design of the study. Material preparation, data collection, and analysis were performed by Julián E. Barahona-Correa, Jorge Flórez-Suárez, and Gerardo Quintana-López. The manuscript was drafted by Julián E. Barahona-Correa and Jorge Flórez-Suárez and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Disclosures
None.
Ethics approval
As a descriptive non-interventional study, this study was considered a no-risk research; thus, a waiver of written informed consent was obtained. The collected data were de-identified and handled by authorized study personnel. Data were used for research purposes only, in agreement with the Helsinki declaration and resolution number 008430 of 1993 issued by the Ministry of Health from the Republic of Colombia.
Consent to participate
See previous subtitle.
Consent for publication
Not applicable.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Transparency disclosure: The present work is an expansion of a prior interim analysis that is being considered for publication in the Colombian Journal of Rheumatology. This interim analysis was submitted as it received an award in the Colombian Congress of Rheumatology that requested, as a condition, to submit a manuscript with the presented data to the journal. The results of the present work have been published as an abstract in conference proceedings or submitted as interim analysis, in the following references:
ACR Annual Meeting 2019
Barahona-Correa J, et al. Differences in Clinical Outcomes According to the Healthcare Regime in Colombian Patients with Rheumatoid Arthritis [abstract]. Arthritis Rheumatol. 2019; 71 (suppl 10). (Abstract number: 1156) https://acrabstracts.org/abstract/differences-in-clinical-outcomes-according-to-the-healthcare-regime-in-colombian-patients-with-rheumatoid-arthritis/.
Colombian Congress of Rheumatology
Barahona-Correa JE, et al. Diferencias en la oportunidad de acceso y desenlaces de pacientes con artritis reumatoide en distintos regímenes de salud en Colombia. Rev. Colomb Reumatol. 2019; 26 (Supl Congr): 17. (Abstract number: 22) https://www.elsevier.es/es-revista-revista-colombiana-reumatologia-374-pdf-X0121812319636366
Colombian Journal of Rheumatology - Interim analysis submission (Short communication)
Submission number: RCREU-D-20-00036
Rights and permissions
About this article
Cite this article
Barahona-Correa, J.E., Flórez-Suárez, J., Coral-Alvarado, P. et al. Does healthcare regime affiliation influence the clinical outcomes of patients with rheumatoid arthritis?. Clin Rheumatol 40, 877–886 (2021). https://doi.org/10.1007/s10067-020-05347-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10067-020-05347-2