Abstract
Purpose
To compare the efficacy of chlorhexidine-gluconate versus povidone iodine in preoperative skin preparation in the prevention of surgical site infections (SSIs) in clean-contaminated upper abdominal surgeries.
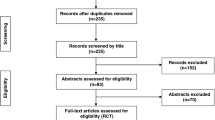
Methods
This was a prospective randomized controlled trial conducted on patients undergoing clean-contaminated upper abdominal surgeries. A total of 351 patients 18–70 years old were randomized into two groups; chlorhexidine and povidone iodine skin preparation before surgery.
Results
The incidence of SSIs in the chlorhexidine group was 10.8 %, in comparison to 17.9 % in the povidone iodine group. The odds ratio was 0.6 in favor of chlorhexidine use, but the results were not statistically significant (P = 0.06). In the first postoperative week, SSIs developed in 7 % of patients in the chlorhexidine group and 14.1 % in the povidone iodine group (P = 0.03), and in the second postoperative week, SSIs were present in 4.1 % of the patients in the chlorhexidine group and 4.4 % in the povidone iodine group, which was not statistically significant (P = 0.88).
Conclusions
The incidence of SSIs after clean-contaminated upper abdominal surgeries was lower with the use of chlorhexidine skin preparation than with povidone iodine preparation, although the results were not statistically significant. However, the odds ratio between the two groups favored the use of chlorhexidine over povidone iodine for preventing SSIs.


Similar content being viewed by others
References
Leaper DJ. Risk factors for and epidemiology of surgical site infections. Surg Infect. 2010;11:283–7.
Zhan C, Miller MR. Excess length of stay, charges, and mortality attributable to medical injuries during hospitalization. JAMA. 2003;290:1868–74.
Kirkland KB, Briggs JP, Trivette SL, et al. The impact of surgical-site infections in the 1990s: attributable mortality, excess length of hospitalization, and extra costs. Infect Control Hosp Epidemiol. 1999;20:725–30.
Mangram AJ, Horan TC, Pearson ML, Silver LC, Jarvis WR, The Hospital Infection Control Practices Advisory Committee. Guideline for the prevention of surgical site infection. Infect Control Hosp Epidemil. 1999; 20:247–80.
Kulaylat MN, Dayton MT. Surgical complications. In: Townsend CM, Beauchamp RD, Evers BM, Mattox KL, editors. Sabiston textbook of surgery. 18th ed. Philadelphia: Saunders; 2008. p. 331–4.
Lilani SP, Jangale N, Chowdhary A, Daver GB. Surgical site infection in clean and clean-contaminated cases. Indian J Med Microbiol. 2005;23:249–52.
Kamat US, Fereirra AMA, Kulkarni MS, Motghare DD. A prospective study of surgical site infections in a teaching hospital in Goa. Indian J Surg. 2008;70:120–4.
National Nosocomial Infections Surveillance Systems (NNIS). System report: data summary from January 1992–June 2001. Am J Infect Control. 2001;29:404–21.
Malangoni MA, Cheadle WG, Dodson TF, et al. Roundtable discussion: new opportunities for reducing risk of surgical site infection. Surg Infect. 2006;7:23–9.
US Food and Drug Administration. Tentative final monograph for healthcare antiseptic drug products: proposed rules. 21 CRF Parts 333 and 369. Fed Regist Part III. 1994;59:31401–2.
Alexander WJ, Solomkin J, Edwards M. Updated Recommendations for Control of Surgical Site Infections. Ann Surg. 2011;253:1082–93.
Digison MB, BSN RN. A review of anti-septic agents for pre-operative skin preparation. Plast Surg Nurs. 2007; 27:185–189.
Schenck H, Simak P, Haedicke E. Structure of polyvinylpyrrolidone-lodine (Povidone-lodine). J Pharm Sci. 1979;68:1505–9.
Lacey RW. Antibacterial activity of povidone iodine towards non-sporing bacteria. J Appl Bacteriol. 1979;46:443–9.
Edmiston CE, Okoli O, Graham MB, Sinski S, Seabrook GR. Evidence for using chlorhexidine gluconate preoperative cleansing to reduce the risk of surgical site infection. AORN J. 2010;92:509–18.
Cecilio RL, Pine FJ, Palileo E, Rasco B, Isaac C, Siasoco RE. Microbiological efficacy of chlorhexidine: an in vitro study on 400 bacterial isolates from four Metro Manila hospitals. Phil J Microbiol Infect Dis. 1983;12:7–13.
Mulberrry G, Snyder AT, Heilman J, Pyrek J, Stahl J. Evaluation of a waterless, scrubless chlorhexidine gluconate/ethanol surgical scrub for antimicrobial efficacy. Am J Infect Control. 2001;29:377–82.
Holder C, Zellinger M. Daily bathing with chlorhexidine in the ICU to prevent central line-associated infections. J Clin Outcome Manag. 2009;16:509–13.
Hranjec T, Swenson BR, Sawyer RG. Surgical Site Infection Prevention: how we do it. Surg Infect. 2010;11:289–93.
Hayek U, Emerson JM, Gardner AM. A placebo-controlled trial of the effect of two preoperative baths or showers with chlorhexidine detergent on postoperative wound infection rates. J Hosp Infect. 1987;10:165–72.
Mimoz O, Karim A, Mercat A, et al. Chlorhexidine compared with povidone-iodine as skin preparation before blood culture: a randomized controlled trial. Ann Intern Med. 1999;131:834–7.
Milstone AM, Passaretti CL, Perl TM. Chlorhexidine: expanding the armamentarium for infection control and prevention. Clin Infect Dis. 2008;46:274–81.
Edmiston CE Jr, Krepel CJ, Seabrook GR, Lewis BD, Brown KR, Towne JB. Preoperative shower revisited: can high topical antiseptic levels be achieved on the skin surface prior to surgical admission? J Am Coll Surg. 2008;207:233–9.
Darouiche RO, Wall MJ, Itani KMF, et al. Chlorhexidine-alcohol versus povidine-iodine for surgical-site antisepsis. N Engl J Med. 2010;362:18–26.
Culligan PJ, Kubik K, Murphy M, Blackwell L, Snyder J. A randomized trial that compared povione iodine and chiorhexidine as antiseptics for vaginal hysterectomy. Am J Obstet Gynecol. 2005;192:422–5.
Noorani A, Rabey N, Walsh SR, Davies RJ. Systematic review and meta-analysis of preoperative antisepsis with chlorhexidine versus povidone-iodine in clean- contaminated surgery. Br J Surg. 2010;97:1614–20.
Levin I, Amer-Alshiek J, Avni A, Lessing BJ, Satel A, Almog B. Chlorhexidine and alcohol versus povidone-iodine for antisepsis in gynecological surgery. J Women Health. 2011;20:321–4.
Swenson BR, Hedrick TL, Metzger R, et al. Effects of preoperative skin preparation on postoperative wound infection rates: a prospective study of 3 skin preparation protocols. Infect Control Hosp Epidemiol. 2009;30:964–71.
Acknowledgments
There were no funding resources for this study.
Conflict of interest
There are no conflicts of interest to declare.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Srinivas, A., Kaman, L., Raj, P. et al. Comparison of the efficacy of chlorhexidine gluconate versus povidone iodine as preoperative skin preparation for the prevention of surgical site infections in clean-contaminated upper abdominal surgeries. Surg Today 45, 1378–1384 (2015). https://doi.org/10.1007/s00595-014-1078-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00595-014-1078-y