Abstract
Purpose
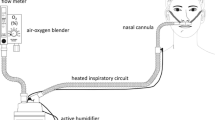
Heated humidified high-flow nasal cannula (HFNC) oxygen therapy is one of the most important oxygen therapy methods, which are commonly applied to relieve dyspnea in advanced cancer patients. Our study aims to observe the efficacy and safety of HFNC oxygen therapy on dyspnea patients with advanced cancer and explore the clinical application.
Methods
Sixty subjects with advanced cancer requiring oxygen therapy from a grade 3, class A hospital in China were recruited and randomized (1:1) to traditional nasal catheter oxygen therapy or HFNC. Primary outcomes were dyspnea, oral dryness, and sleep condition, which were recorded after 72-h treatment. Secondary outcomes were heart rate (HR), respiration rate (RR), SpO2, PaO2, and PaCO2, which were recorded after 2, 6, 24, and 72 h treatment.
Results
Seventy-two hours after treatment, there were significant improvements in all primary outcomes (P < 0.001). PaO2 and RR were statistically changed 2 h after HFNC treatment (P < 0.001). PaCO2 and HR were statistically changed 24 h after HFNC treatment (P < 0.001).
Conclusion
HFNC oxygen therapy has good effect, high safety, and is easy to be accepted by dyspnea patients with advanced cancer. It can be used as the first choice of oxygen therapy for these patients and has broad clinical prospects.
Trial registration.
This work was retrospectively registered in the Chinese Clinical Trials Registry (ChiCTR2100049582) on August 4, 2021.

Similar content being viewed by others
Availability of data and material
All data can be available on https://www.chictr.org.cn/index.aspx.
Code availability
SPSS version 22.0 (SPSS Inc., Chicago, IL, USA).
References
Sung H, Ferlay J, Siegel RL et al (2021) Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin 71:209–249. https://doi.org/10.3322/caac.21660
Tishelman C, Petersson L-M, Degner LF et al (2007) Symptom prevalence, intensity, and distress in patients with inoperable lung cancer in relation to time of death. J Clin Oncol 25:5381–5389. https://doi.org/10.1200/jco.2006.08.7874
Maltoni M, Caraceni A, Brunelli C et al (2005) Prognostic factors in advanced cancer patients: evidence-based clinical recommendations — a study by the Steering Committee of the European Association for Palliative Care. J Clin Oncol 23:6240–6248. https://doi.org/10.1200/jco.2005.06.866
Tanaka K, Akechi T, Okuyama T et al (2002) Impact of dyspnea, pain, and fatigue on daily life activities in ambulatory patients with advanced lung cancer. J Pain Symptom Manage 23:417–423. https://doi.org/10.1016/s0885-3924(02)00376-7
Gupta D, Lis CG, Grutsch JF (2007) The relationship between dyspnea and patient satisfaction with quality of life in advanced cancer. Support Care Cancer 15:533–538. https://doi.org/10.1007/s00520-006-0178-7
Reddy SK, Parsons HA, Elsayem A et al (2009) Characteristics and correlates of dyspnea in patients with advanced cancer. J Palliat Med 12:29–36. https://doi.org/10.1089/jpm.2008.0158
Bruera E, Schmitz B, Pither J et al (2000) The frequency and correlates of dyspnea in patients with advanced cancer. J Pain Symptom Manage 19:357–362. https://doi.org/10.1016/s0885-3924(00)00126-3
Lorenz KA, Lynn J, Dy SM et al (2008) Evidence for improving palliative care at the end of life: a systematic review. Ann Intern Med 148:147–159. https://doi.org/10.7326/0003-4819-148-2-200801150-00010
Simone CB 2nd, Jones JA (2013) Palliative care for patients with locally advanced and metastatic non-small cell lung cancer. Ann Palliat Med 2:178–188. https://doi.org/10.3978/j.issn.2224-5820.2013.08.02
Ben-Aharon I, Gafter-Gvili A, Leibovici L et al (2012) Interventions for alleviating cancer-related dyspnea: a systematic review and meta-analysis. Acta Oncol 51:996–1008. https://doi.org/10.3109/0284186x.2012.709638
Kallstrom TJ and American Association for Respiratory C. 2002 AARC Clinical Practice Guideline: oxygen therapy for adults in the acute care facility—2002 revision & update. Respir care. 47: 717-720.
Milani GP, Plebani AM, Arturi E et al (2016) Using a high-flow nasal cannula provided superior results to low-flow oxygen delivery in moderate to severe bronchiolitis. Acta Paediatr 105:E368–E372. https://doi.org/10.1111/apa.13444
Chanques G, Riboulet F, Molinari N et al (2013) Comparison of three high flow oxygen therapy delivery devices: a clinical physiological cross-over study. Minerva Anestesiol 79:1344–1355
Ischaki E, Pantazopoulos I and Zakynthinos S. 2017 Nasal high flow therapy: a novel treatment rather than a more expensive oxygen device. Eur Respir Rev. 26. https://doi.org/10.1183/16000617.0028-2017.
Nagata K, Morimoto T, Fujimoto D et al (2015) Efficacy of high-flow nasal cannula therapy in acute hypoxemic respiratory failure: decreased use of mechanical ventilation. Respir Care 60:1390–1396. https://doi.org/10.4187/respcare.04026
Mercadante S, Giarratano A, Cortegiani A et al (2017) Application of palliative ventilation: potential and clinical evidence in palliative care. Support Care Cancer 25:2035–2039. https://doi.org/10.1007/s00520-017-3710-z
Roca O, Riera J, Torres F et al (2010) High-flow oxygen therapy in acute respiratory failure. Respir Care 55:408–413
Mauri T, Turrini C, Eronia N, Grasselli G, Volta CA, Bellani G, Presenti A (2018) Physiologic effects of high-flow nasal cannula in acute hypoxemic respiratory failure. Am J Respir Crit Care Med 113:80–80
Parke R, McGuinness S, Dixon R et al (2013) Open-label, phase II study of routine high-flow nasal oxygen therapy in cardiac surgical patients. Br J Anaesth 111:925–931. https://doi.org/10.1093/bja/aet262
Nishimura M (2016) High-flow nasal cannula oxygen therapy in adults: physiological benefits, indication, clinical benefits, and adverse effects. Respir Care 61:529–541. https://doi.org/10.4187/respcare.04577
Ruangsomboon O, Dorongthom T, Chakorn T et al (2020) High-flow nasal cannula versus conventional oxygen therapy in relieving dyspnea in emergency palliative patients with do-not-intubate status: a randomized crossover study. Ann Emerg Med 75:615–626. https://doi.org/10.1016/j.annemergmed.2019.09.009
McGinley BM, Patil SP, Kirkness JP et al (2007) A nasal cannula can be used to treat obstructive sleep apnea. Am J Respir Crit Care Med 176:194–200. https://doi.org/10.1164/rccm.200609-1336OC
Wilson RC, Jones PW (1989) A comparison of the visual analog scale and modified Borg scale for the measurement of dyspnea during exercise. Clin Sci 76:277–282. https://doi.org/10.1042/cs0760277
Muendel T, Feng S, Tatkov S et al (2013) Mechanisms of nasal high flow on ventilation during wakefulness and sleep. J Appl Physiol 114:1058–1065. https://doi.org/10.1152/japplphysiol.01308.2012
Otis AB, Fenn WO, Rahn H (1950) Mechanics of breathing in man. J Appl Physiol 2:592–607
Pisani L, Fasano L, Corcione N et al (2017) Change in pulmonary mechanics and the effect on breathing pattern of high flow oxygen therapy in stable hypercapnic COPD. Thorax 72:373–375. https://doi.org/10.1136/thoraxjnl-2016-209673
Adams CF, Geoghegan PH, Spence CJ et al (2018) Modelling nasal high flow therapy effects on upper airway resistance and resistive work of breathing. Respir Physiol Neurobiol 254:23–29. https://doi.org/10.1016/j.resp.2018.03.014
Kulkarni AP, Agarwal V (2008) Extubation failure in intensive care unit: predictors and management. Indian J Crit Care Med 12:1–9. https://doi.org/10.4103/0972-5229.40942
O’Driscoll BR, Howard LS, Davison AG et al (2011) Emergency oxygen use in adult patients: concise guidance. Clin Med 11:372–373. https://doi.org/10.7861/clinmedicine.11-4-372
Krinsley JS, Reddy PK and Iqbal A. 2012. What is the optimal rate of failed extubation? Crit Care, 16. https://doi.org/10.1186/cc11185.
Moeller W, Celik G, Feng S et al (2015) Nasal high flow clears anatomical dead space in upper airway models. J Appl Physiol 118:1525–1532. https://doi.org/10.1152/japplphysiol.00934.2014
Moeller W, Feng S, Domanski U et al (2017) Nasal high flow reduces dead space. J Appl Physiol 122:191–197. https://doi.org/10.1152/japplphysiol.00584.2016
Dysart K, Miller TL, Wolfson MR et al (2009) Research in high flow therapy: mechanisms of action. Respir Med 103:1400–1405. https://doi.org/10.1016/j.rmed.2009.04.007
Lee JH, Rehder KJ, Williford L et al (2013) Use of high flow nasal cannula in critically ill infants, children, and adults: a critical review of the literature. Intensive Care Med 39:247–257. https://doi.org/10.1007/s00134-012-2743-5
Kumar H, Spence CJT, Tawhai MH (2015) Modeling the pharyngeal pressure during adult nasal high flow therapy. Respir Physiol Neurobiol 219:51–57. https://doi.org/10.1016/j.resp.2015.06.011
Maggiore SM, Idone FA, Vaschetto R et al (2014) Nasal high-flow versus venturi mask oxygen therapy after extubation. Am J Respir Crit Care Med 190:282–288. https://doi.org/10.1164/rccm.201402-0364OC
Groves N, Tobin A (2007) High flow nasal oxygen generates positive airway pressure in adult volunteers. Aust Crit Care 20:126–131
Parke RL, Eccleston ML, McGuinness SP (2011) The effects of flow on airway pressure during nasal high-flow oxygen therapy. Respir Care 56:1151–1155. https://doi.org/10.4187/respcare.01106
Yao J-J, Peng M-M, Zou G-H et al (2020) Effects of flow on carbon dioxide washout and nasal airway pressure in healthy adult volunteers during the constant-flow mode in a non-invasive ventilator. Chin Med J 133:2515–2517. https://doi.org/10.1097/cm9.0000000000001079
Corley A, Caruana LR, Barnett AG et al (2011) Oxygen delivery through high-flow nasal cannulae increase end-expiratory lung volume and reduce respiratory rate in post-cardiac surgical patients. Br J Anaesth 107:998–1004. https://doi.org/10.1093/bja/aer265
Spoletini G, Alotaibi M, Blasi F et al (2015) Heated humidified high-flow nasal oxygen in adults mechanisms of action and clinical implications. Chest 148:253–261. https://doi.org/10.1378/chest.14-2871
Williams R, Rankin N, Smith T et al (1996) Relationship between the humidity and temperature of inspired gas and the function of the airway mucosa. Crit Care Med 24:1920–1929. https://doi.org/10.1097/00003246-199611000-00025
Lellouche F, Maggiore SM, Lyazidi A et al (2009) Water content of delivered gases during non-invasive ventilation in healthy subjects. Intensive Care Med 35:987–995. https://doi.org/10.1007/s00134-009-1455-y
Yao JJ, Li W, Peng MM, et al. The comfort assessment in healthy adults during constant-flow mode in noninvasive ventilator. Clinical Respiratory Journal. https://doi.org/10.1111/crj.13459.
Jones PG, Kamona S, Doran O et al (2016) Randomized controlled trial of humidified high-flow nasal oxygen for acute respiratory distress in the emergency department: the HOT-ER study. Respir Care 61:291–299. https://doi.org/10.4187/respcare.04252
Funding
This work was supported by Qilu Hospital of Shandong University [2018-6].
Author information
Authors and Affiliations
Contributions
Conceptualization: ZX, PL; methodology: ZX, PL; formal analysis and investigation: ZX, PL, CZ; writing — original draft preparation: ZX, PL, CZ, DM; writing — review and editing: ZX, PL, CZ, DM; funding acquisition: DM; supervision: DM.
Corresponding author
Ethics declarations
Ethics approval
All procedures performed in studies involving human participants were in accordance with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. The trial was approved by the First Hospital of Zibo City in China Ethics Committee (No.2019016).
Consent to participate
Informed consent was obtained from all individual participants included in the study.
Consent for publication
Consent for publication was obtained from all individual participants included in the study.
Conflict of interest
The authors declare no competing interests.
Additional declarations for articles in Life Science Journals that report the results of studies involving humans and/or animals
Not applicable.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Xu, Z., Li, P., Zhang, C. et al. Effect of heated humidified high-flow nasal cannula (HFNC) oxygen therapy in dyspnea patients with advanced cancer, a randomized controlled clinical trial. Support Care Cancer 30, 9093–9100 (2022). https://doi.org/10.1007/s00520-022-07330-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00520-022-07330-w