Abstract
Aim
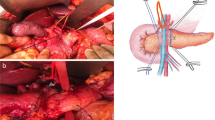
In addition to ischemia there is also anastomotic ends tension proven to be a risk factor for anastomotic leak. HT vascular ligation is accepted as a rule, in attempt to achieve tension-free anastomosis. LT is a preferred option, based on the more accurate preservation of proximal intestinal segment microperfusion and lower risk of damage to the hypogastric plexus. The aim of this study is evaluation of comparative indicators in high tie (HT) and low tie (LT) laparoscopic rectal resections.
Methods
A prospective nonrandomized comparative cohort study of patients in our department with cancer of the rectum in clinical stage I–III, operated on in laparoscopic approach over a 6-years period.
Results
For the period 2015–2020, a number of 208 laparoscopic surgeries have been done for rectal cancer. Patients were divided into three groups—group A with HT vascular ligation 116 pts. (69%), group B—53 pts. (25%), underwent low ligation—LT and group C—39pts. (19%) low tie plus lymph node dissection of the apical LN group (LT-appic LND). The distribution was made without randomization, based on the operators’ expertise. Anastomotic leaks were 3.8% in group A, 3.0% in group B and 2.9% in group C (p > 0.05) with no significance difference. There is no significant difference in the number of lymph nodes obtained in group A and group B, while in group C the number of the harvested lymph nodes was higher (p < 0.05). The indicators for intestinal / defecation dysfunction, as well as for urinary/sexual dysfunction, according to our data, are significantly more favorable in patients with LT, in contrast to the other two groups.
Conclusion
HT vascular ligation attempts to achieve tension-free anastomosis and more harvested lymph nodes. However, LT could be a preferred option, based on the lack of significant evidence for a difference in specific oncological survival and due to more accurate preservation of proximal intestinal segment microperfusion to prevent anastomosis dehiscence, also for its lower risk of damage to the hypogastric plexus. Splenic flexure mobilization provides elongation of the proximal intestinal segment, but has no proven effect on anastomotic leakage incidence. It increases surgical duration and is in fact necessary in up to 30% of the cases. At the present moment there is no precise data whether LT has an advantage in terms of prevention of autonomic nervous and urogenital dysfunction. New prospective randomized and highly probative studies are needed to standardize the procedures in specific clinical situations.










Similar content being viewed by others
References
Loeweneck H, Feifel G (1993) Lanz Wachsmuth Praktische Anatomie Bauch. Springer, Berlin
Lange MM, Buunen M, van de Velde CJ, Lange JF (2008) Level of arterial ligation in rectal cancer surgery: low tie preferred over high tie. A review. Dis Colon Rectum 51(7):1139–1145. https://doi.org/10.1007/s10350-008-9328-y
Tepper JE, O’Connell MJ, Niedzwiecki D et al (2001) Impact of number of nodes retrieved on outcome in patients with rectal cancer. J Clin Oncol 19:157–163
Prandi M, Lionetto R, Bini A et al (2002) Prognostic evaluation of stage B colon cancer patients is improved by an adequate lymphadenectomy: results of a secondary analysis of a large scale adjuvant trial. Ann Surg 235:458–463
Kanemitsu Y, Hirai T, Komori K, Kato T (2006) Survival benefit of high ligation of the inferior mesenteric artery in sigmoid colon or rectal cancer surgery. Br J Surg 93:609–615
Yasuda K, Kawai K, Ishihara S, Murono K, Otani K, Nishikawa T, Tanaka T, Kiyomatsu T, Hata K, Nozawa H, Yamaguchi H, Aoki S, Mishima H, Maruyama T, Sako A, Watanabe T (2016) Level of arterial ligation in sigmoid colon and rectal cancer surgery. World J Surg Oncol. https://doi.org/10.1186/s12957-016-0819-3
Sugarbaker PH (1993) Metastatic inefficiency: the scientific basis for resection of liver metastases from colorectal cancer. J Surg Oncol Suppl 3:158–160
Sauer I, Bacon HE (1952) A new approach for excision of carcinoma of the lower portion of the rectum and anal canal. Surg Gynecol Obstet 95:229–242
Hida J, Yasutomi M, Maruyama T, Fujimoto K, Nakajima A, Uchida T, et al (1998) Indication for using high ligation of the inferior mesenteric artery in rectal cancer surgery. Examination of nodal metastases by the clearing method. Dis Colon Rectum 41(8):984–987
Bruch HP, Schwandner O, Schiedeck TH, Roblick UJ (1999) Actual standards and controversies on opzerative technique and lymph-node dissection in colorectal cancer. Langenbecks Arch Surg 384(2):167–175
Wexner SD (1998) Invited editorial. Dis Colon Rectum 41:987–989
You X, Liu Q, Wu J, Wang Y, Huang Ch, Cao G, Dai J, Chen D, Zhou Y (2020) High versus low ligation of inferior mesenteric artery during laparoscopic radical resection of rectal cancer. Medicine 99(12):e19437. https://doi.org/10.1097/MD.0000000000019437
Fujii C, Ishibe A, Ota M, Watanabe К, Watanabe J, Kunisaki C et al (2018) Randomized clinical trial of high versus low inferior mesenteric artery ligation during anterior resection for rectal cancer. BJS Open 2(4):195–202. https://doi.org/10.1002/bjs5.71
Boström P, Haapamäki MM, Matthiessen P, Ljung R, Rutegård J, Rutegård M (2015) High arterial ligation and risk of anastomotic leakage in anterior resection for rectal cancer in patients with increased cardiovascular risk. Colorectal Dis 17(11):1018–1027. https://doi.org/10.1111/codi.12971
Jafari MD, Lee KH, Halabi WJ, et al (2013) The use of indocyanine green fluorescence to assess anastomotic perfusion during robotic assisted laparoscopic rectal surgery. Surg Endosc 27:3003–3008
Jafari MD, Wexner SD, Martz JE, McLemore EC, Margolin DA, Sherwinter DA, et al. Perfusion assessment in laparoscopic left sided/anterior resection (PILLAR) II: A multi-institutional study. Ann Surg. A 2015 by Journal of the American College of Surgeons. Published by Elsevier Inc.open access article under the CC BY-NC-SA license,Vol. 220, No. 1, January 2015, pp 82–92 (http://creativecommons.org/licenses/by-nc-sa/3.0/),www.elementalhealthcare.co.uk
Hoer J, Roegels A, Prescher A, Klosterhalfen B, Tons C, Schumpelick V (2000) Preserving autonomic nerves in rectal surgery. Results of surgical preparation on human cadavers with fixed pelvic sections. Chirurg. 71(10):1222–1229
Nano M, Dal Corso H, Ferronato M, Solej M, Hor- nung JP, Dei PM (2004) Ligation of the inferior mesenteric artery in the surgery of rectal cancer: anatomical considerations. Dig Surg 21(2):123–126. https://doi.org/10.1159/000077347.
Zhou ZG, Hu M, Li Y, Lei WZ, Yu YY, Cheng Z et al (2004) Laparoscopic versus open total mesorectal excision with anal sphincter preservation for low rectal cancer. Surg Endosc 18(8):1211–1215. https://doi.org/10.1007/s00464-003-9170-1
Matsuda K, Hotta T, Takifuji K, Yokoyama S, Oku Y, Watanabe T et al (2015) Randomized clinical trial of defaecatory function after anterior resection for rectal cancer with high versus low ligation of the inferior mesenteric artery. Br J Surg 102(5):501–508. https://doi.org/10.1002/bjs.9739
Mari GM, Crippa J, Cocozza E, Berselli M, Livraghi L, Carzaniga P, Valenti F, Roscio F, Ferrari G, Mazzola M, Magistro C, Origi M, Forgione A, Zuliani W, Scandroglio I, Pugliese R, Costanzi ATM, Maggioni D (2019) Low ligation of inferior mesenteric artery in laparoscopic anterior resection for rectal cancer reduces genitourinary dysfunction: results from a randomized controlled trial (HIGHLOW Trial). Ann Surg 269(6):1018–1024. https://doi.org/10.1097/SLA.0000000000002947
Bonnet S, Berger A, Hentati N, Abid B, Chevallier JM, Wind PE et al (2012) High tie versus low tie vascular ligation of the inferior mesenteric artery in colorectal cancer surgery: impact on the gain in colon length and implications on the feasibility of anastomoses. Dis Colon Rectum 55(5):515–521. https://doi.org/10.1097/DCR.0b013e318246f1a2
Corder AP, Karanjia ND, Williams JD, Heald RJ (1992) Flush aortic tie versus selective preservation of the ascending left colic artery in low anterior resection for rectal carcinoma. Br J Surg 79(7):680–682. https://doi.org/10.1002/bjs.1800790730
Pezim ME, Nicholls RJ (1984) Survival after high or low ligation of the inferior mesenteric artery during curative surgery for rectal cancer. Ann Surg 200(6):729–733
Ke TW, Geniales CR, Chen WTL (2018) The role of splenic flexure mobilization in laparoscopic rectal surgery for rectal cancer. Mini-invasive Surg 2:35. https://doi.org/10.20517/2574-1225.2018.46
Reddy SH, Gupta V, Yadav TD, Singh G, Sahni D (2016) Lengthening of left colon after rectal resection: what all is adequate? A prospective cohort study. Int J Surg 31:27–32. https://doi.org/10.1016/j.ijsu.2016.05.042
Longo W, Reddy V, Audisio R (2014) Modern Management of Cancer of the Rectum. 2nd ed. Springer. https://www.springer.com/gp/book/9781447103318
Gouvas N, Gogos-Pappas G, Tsimogiannis K, Agalianos C, Tsimoyiannis E, Dervenis C, Xynos E (2014) Impact of splenic flexure mobilization on short-term outcomes after laparoscopic left colectomy for colorectal cancer. Surg Laparosc Endosc Percutan Tech 24(5):470–474. https://doi.org/10.1097/SLE.0b013e31829ce62a
Girard E, Trilling B, Rabattu PY, Sage PY, Taton N, Robert Y et al (2019) Level of inferior mesenteric artery ligation in low rectal cancer surgery: high tie preferred over low tie. Tech Coloproctol 23(3):267–271. https://doi.org/10.1007/s10151-019-01931-0
Kennedy R, Jenkins I, Finan PJ (2008) Controversial topics in surgery: splenic flexure mobilisation for anterior resection performed for sigmoid and rectal cancer. Ann R Coll Surg Engl 90(8):638–642. https://doi.org/10.1308/003588408X358774
Hajibandeh S, Hajibandeh S, Maw A (2020) Meta-analysis and trial sequential analysis of randomized controlled trials comparing high and low ligation of the inferior mesenteric artery in rectal cancer surgery. Dis Colon Rectum 63(7):988–999. https://doi.org/10.1097/DCR.0000000000001693
Barry MJ, Fowler FJ, Jr, O'Leary MP, Bruskewitz RC, Holtgrewe HL, Mebust WK (1992) The American Urological Association symptomc index for benign prostatic hyperplasia. The measurement committee of the American Urological Association. J Urol 148:1549–1557
Rosen RC, Riley A, Wagner G, Osterloh IH, Kirkpatrick J, Mishra A (1997) The international index of erectile function (IIEF): a multidimensional scale for assessment of erectile dysfunction. Urology 49:822–830
Sirikurnpiboon S, Angkurawaranon C, Pinyoteppratarn R, Vitoopinyoparb K, Muyphuag B, Chantawibul S, Ratanachu-ek T. (2017). Low ligation inferior mesenteric artery versus selective sigmoidal artery ligation in sigmoid colon cancer: a comparative study. Int Surg J 4:3201. https://doi.org/10.18203/2349-2902.isj20174489
Goldstein NS, Sanford W, Coffey M, Layfield LJ (1996) Lymph node recovery from colorectal resection specimens removed for adenocarcinoma. Trends over time and a recommendation for a minimum number of lymph nodes to be recovered. Am J Clin Pathol. 106:209–216
Rutegård M, Hassmén N, Hemmingsson O, Haapamäki MM, Matthiessen P, Rutegård J. (2016) Anterior resection for rectal cancer and visceral blood flow: an explorative study. Scand J Surg 105(2):78–83. https://doi.org/10.1177/1457496915593692.
Hinoi T, Okajima M, Shimomura M, Egi H, Ohdan H, Konishi F et al (2013) Effect of left colonic artery preservation on anastomotic leakage in laparoscopic anterior resection for middle and low rectal cancer. World J Surg 37(12):2935–2943. https://doi.org/10.1007/s00268-013-2194-3
Tsu**aka S, Kawamura YJ, Tan KY, Mizokami K, Sasaki J, Maeda T et al (2012) Proximal bowel necrosis after high ligation of the inferior mesenteric artery in colorectal surgery. Scand J Surg 101(1):21–25. https://doi.org/10.1177/145749691210100105
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
The participants in the team of this study declare that they do not have any financial obligations or benefits from conducting and the consequences of this study. Drs. Manol Bonev Sokolov, Boril Petrov, Svilen Maslyankov, Kostadin Angelov, Margarita Atanasova, Dochka Tzoneva and Petar Gribnev have no conflicts of interest or financial ties to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Sokolov, M., Petrov, B., Maslyankov, S. et al. Technical considerations depending on the level of vascular ligation in laparoscopic rectal resection. Surg Endosc 36, 1961–1969 (2022). https://doi.org/10.1007/s00464-021-08479-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-021-08479-x