Abstract
Background
Lateral pelvic lymph node dissection (LPND) is a challenging procedure due to its technical difficulty and higher incidence of surgical morbidity. We compared short-term outcomes between laparoscopic and robotic LPND in patients with rectal cancer.
Methods
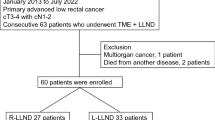
Between May 2006 and December 2014, prospectively collected data from consecutive patients undergoing robotic or laparoscopic total mesorectal excision (TME) with LPND were retrospectively compared. Patients’ demographics, perioperative outcomes, functional results, and initial oncologic outcomes were analyzed.
Results
Fifty and 35 patients underwent robotic or laparoscopic TME with LPND, respectively. Bilateral LPND was performed in 10 patients (20%) in the robotic group and 6 (17.1%) in the laparoscopic group. For unilateral pelvic dissection, the mean operative time was not significantly different between groups (robotic vs. laparoscopic group, 41.0 ± 15.8 min vs. 35.3 ± 13.4 min; P = 0.146), but the EBL was significantly lower in the robotic group (34.6 ± 21.9 mL vs. 50.6 ± 23.8 mL; P = 0.002). Two patients (4.0%) in the robotic group and 7 (20.0%) in the laparoscopic group underwent Foley catheter reinsertion for urinary retention postoperatively (P = 0.029). The mean number of harvested lateral pelvic lymph nodes (LPNs) was 6.6 (range 0–25) in the robotic group and 6.4 (range 1–14) in the laparoscopic group. Pathologic LPN metastatic rate was not different between groups (robotic vs. laparoscopic group, 28.0 vs. 41.2%; P = 0.243). During the median follow-up of 26.3 months, overall recurrence rate was not different between groups (robotic vs. laparoscopic group, 30.0 vs. 31.2%; P = 0.850). Three patients (6.0%) in the robotic group and 4 (11.4%) in the laparoscopic group developed local recurrence (P = 0.653).
Conclusions
Robotic TME with LPND is safe and feasible with favorable short-term surgical outcomes.
Similar content being viewed by others
References
Sauer I, Bacon HE (1951) Influence of lateral spread of cancer of the rectum on radicability of operation and prognosis. Am J Surg 81:111–120
Heald RJ, Ryall RD (1986) Recurrence and survival after total mesorectal excision for rectal cancer. Lancet 1:1479–1482
Sauer R, Becker H, Hohenberger W et al (2004) Preoperative versus postoperative chemoradiotherapy for rectal cancer. N Engl J Med 351:1731–1740
Bosset JF, Collette L, Calais G et al (2006) Chemotherapy with preoperative radiotherapy in rectal cancer. N Engl J Med 355:1114–1123
Garcia-Aguilar J, Cromwell JW, Marra C et al (2001) Treatment of locally recurrent rectal cancer. Dis Colon Rectum 44:1743–1748
Kim TH, Jeong SY, Choi DH et al (2008) Lateral lymph node metastasis is a major cause of locoregional recurrence in rectal cancer treated with preoperative chemoradiotherapy and curative resection. Ann Surg Oncol 15:729–737
Akiyoshi T, Ueno M, Matsueda K et al (2014) Selective lateral pelvic lymph node dissection in patients with advanced low rectal cancer treated with preoperative chemoradiotherapy based on pretreatment imaging. Ann Surg Oncol 21:189–196
Park JS, Choi GS, Lim KH et al (2012) Laparoscopic extended lateral pelvic node dissection following total mesorectal excision for advanced rectal cancer: initial clinical experience. Surg Endosc 25:3322–3329
Liang JT (2011) Technical feasibility of laparoscopic lateral pelvic lymph node dissection for patients with low rectal cancer after concurrent chemoradiation therapy. Ann Surg Oncol 18:153–159
Konishi T, Kuroyanagi H, Oya M et al (2011) Multimedia article. Lateral lymph node dissection with preoperative chemoradiation for locally advanced lower rectal cancer through a laparoscopic approach. Surg Endosc 25:2358–2359
Hellan M, Anderson C, Ellenhorn JD et al (2007) Short-term outcomes after robotic-assisted total mesorectal excision for rectal cancer. Ann Surg Oncol 14:3168–3173
Park JS, Choi GS, Lim KH et al (2010) Robotic-assisted versus laparoscopic surgery for low rectal cancer: case-matched analysis of short-term outcomes. Ann Surg Oncol 17:3195–3202
Kang J, Yoon KJ, Min BS et al (2013) The impact of robotic surgery for mid and low rectal cancer: a case-matched analysis of a 3-arm comparison—open, laparoscopic, and robotic surgery. Ann Surg 257:95–101
Kobayashi H, Mochizuki H, Kato T et al (2009) Outcomes of surgery alone for lower rectal cancer with and without pelvic sidewall dissection. Dis Colon Rectum 52:567–576
Akiyoshi T, Watanabe T, Ueno M (2012) Is lateral pelvic lymph node dissection no longer necessary for low rectal cancer after neoadjuvant therapy and TME to reduce local recurrence? J Gastrointest Surg 16:2341–2342
Kojima M, Naya Y, Inoue W et al (1997) The American Urological Association symptom index for benign prostatic hyperplasia as a function of age, volume and ultrasonic appearance of the prostate. J Urol 157:2160–2165
Park JA, Choi GS, Park JS et al (2012) Initial clinical experience with robotic lateral pelvic lymph node dissection for advanced rectal cancer. J Korean Soc Coloproctol 28:265–270
Georgiou P, Tan E, Gouvas N et al (2009) Extended lymphadenectomy versus conventional surgery for rectal cancer: a meta-analysis. Lancet Oncol 10:1053–1062
Kusters M, Beets GL, van de Velde CJ et al (2009) A comparison between the treatment of low rectal cancer in Japan and the Netherlands, focusing on the patterns of local recurrence. Ann Surg 249:229–235
Syk E, Torkzad MR, Blomqvist L et al (2006) Radiological findings do not support lateral residual tumour as a major cause of local recurrence of rectal cancer. Br J Surg 93:113–119
Ueno H, Mochizuki H, Hashiguchi Y et al (2007) Potential prognostic benefit of lateral pelvic node dissection for rectal cancer located below the peritoneal reflection. Ann Surg 245:80–87
Moriya Y, Sugihara K, Akasu T et al (1997) Importance of extended lymphadenectomy with lateral node dissection for advanced lower rectal cancer. World J Surg 21:728–732
Lim SB, Yu CS, Kim CW et al (2013) Clinical implication of additional selective lateral lymph node excision in patients with locally advanced rectal cancer who underwent preoperative chemoradiotherapy. Int J Colorectal Dis 28:1667–1674
Watanabe T, Tsurita G, Muto T et al (2002) Extended lymphadenectomy and preoperative radiotherapy for lower rectal cancers. Surgery 132:27–33
Nagawa H, Muto T, Sunouchi K et al (2001) Randomized, controlled trial of lateral node dissection vs. nerve-preserving resection in patients with rectal cancer after preoperative radiotherapy. Dis Colon Rectum 44:1274–1280
Shingo N, Masayuki O, Yosuke S et al (2010) Feasibility of a lateral region sentinel node biopsy of lower rectal cancer guided in indocyanine green using a near-infrared camera system. Ann Surg Oncol 17:144–151
Kyo K, Sameshima S, Takahashi M et al (2006) Impact of autonomic nerve preservation and lateral node dissection on male urogenital function after total mesorectal excision for lower rectal cancer. World J Surg 30:1014–1019
Moriya Y (2006) Function preservation in rectal cancer surgery. Int J Clin Oncol 11:339–343
Fujita S, Akasu T, Mizusawa J et al (2012) Postoperative morbidity and mortality after mesorectal excision with and without lateral lymph node dissection for clinical stage II or stage III lower rectal cancer (JCOG0212): results from a multicentre, randomised controlled, non-inferiority trial. Lancet Oncol 13:616–621
Acknowledgements
This research was supported by Basic Science Research Program through the National Research Foundation of Korea (NRF) funded by the Ministry of Science, ICT and Future Planning (2016R1C1B2016002).
Author information
Authors and Affiliations
Contributions
HJK—analysis and writing of the manuscript. G-SC—responsibility to correspondence and study proposal. JSP, SYP, HJL, ITW, and IKP—enrollment of patients, data collection, and study proposal.
Corresponding author
Ethics declarations
Disclosure
Dr. Hye ** Kim, Gyu-Seog Choi, Jun Seok Park, Soo Yeun Park, Hee Jae Lee, In Taek Woo, and In Kyu Park have no conflicts of interest or financial ties to disclose.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Supplementary material 1 (WMV 207166 KB)
Rights and permissions
About this article
Cite this article
Kim, H.J., Choi, GS., Park, J.S. et al. Selective lateral pelvic lymph node dissection: a comparative study of the robotic versus laparoscopic approach. Surg Endosc 32, 2466–2473 (2018). https://doi.org/10.1007/s00464-017-5948-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-017-5948-4