Abstract
Background
Morbid obesity is strongly associated with nonalcoholic fatty liver disease. However, the effect of underlying liver disease on clinical outcomes following bariatric surgery has not been well studied. This study aims to determine the effect of underlying liver disease on short-term outcomes in bariatric patients using the model of end-stage liver disease (MELD) scoring system as a practical measure of hepatic dysfunction.
Methods
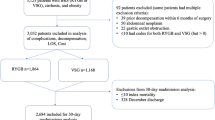
A retrospective cohort analysis was performed using data from the American College of Surgeons’ National surgery quality improvement program participant use files. The study population consisted of patients that underwent elective laparoscopic-stapled bariatric surgery for morbid obesity between 2005 and 2012. Patients were excluded if they had a bleeding disorder or renal failure requiring dialysis. The optimal MELD cut-off score to predict 30-day adverse events was determined and used to stratify patients into two groups. The primary outcome was 30-day adverse events, defined as a postoperative complication or reoperation. The secondary outcome was 30-day mortality. A multiple logistic regression was performed to adjust the odds ratio (OR) estimate for 30-day adverse events based on the MELD cut-off score.
Results
38,875 patients were included in the study population. A MELD score of 7.9 was determined to be the optimal cut-off to predict 30-day adverse events based on the maximized linear combination of specificity and sensitivity. After adjusting for confounding, the OR estimates for 30-day adverse events and mortality using the cut-off score as the key predictor were 1.22 [95 % CI 1.06–1.41] and 2.33 [95 % CI 1.19–4.56], respectively.
Conclusions
Using this large national surgical registry, bariatric patients with MELD scores ≥7.9 had a significant but marginal risk of 30-day adverse events and mortality. This suggests that severity of liver disease may affect bariatric surgery outcomes and should be considered during preoperative evaluations.
Similar content being viewed by others
References
De Ridder R, Schoon E, Smulders J, van Hout G, Stockbrügger R, Koek G (2007) Review article: non-alcoholic fatty liver disease in morbidly obese patients and the effect of bariatric surgery. Aliment Pharmacol Ther 26(Suppl 2):195–201
Teli M, James O, Burt A (1995) The natural history of nonalcoholic fatty liver: a follow-up study. Hepatology 22:1714–1719
Hanje J, Patel T (2007) Preoperative evaluation of patients with liver disease. Nat Clin Pract Gastroenterol Hepatol 4(5):266–276
O’Leary J, Yachimski P, Friedman L (2009) Surgery in the patient with liver disease. Clin Liver Dis 13(2):211
Khuri SF, Henderson WG, Daley J (2007) The patient safety in surgery study: background, study design, and patient populations. J Am Coll Surg 204(6):1089–1102
Khuri SF, Daley J, Henderson W (1997) Risk adjustment of the postoperative mortality rate for the comparative assessment of the quality of surgical care: results of the national veterans affairs surgical risk study. J Am Coll Surg 185(4):315–327
Daley J, Khuri SF, Henderson W (1997) Risk adjustment of the postoperative morbidity rate for the comparative assessment of the quality of surgical care: results of the national veterans affairs surgical risk study. J Am Coll Surg 185(4):328–340
Daley J, Forbes MG, Young GJ (1997) Validating risk-adjusted surgical outcomes: site visit assessment of process and structure national va surgical risk study. J Am Coll Surg 185(4):341–351
Khuri SF, Henderson WG, Daley J (2008) Successful implementation of the department of veterans affairs’ national surgical quality improvement program in the private sector: the patient safety in surgery study. Ann Surg 248(2):329–336
Ribeireiro T, Swain J, Sarr M, Kendrick M, Que F, Sanderson S, Krishnan A, Viker K, Watt K, Charlton M (2011) NAFLD and insulin resistance do not increase the risk of postoperative complications among patients undergoing bariatric surgery—A prospective analysis. Obes Surg 21:310–315
Brolin R, Bradley L, Taliwal R (1998) Unexpected cirrhosis discovered during elective obesity operations. Arch Surg 133(1):84–88
Weingarten TN, Swain JM, Kendrick ML (2011) Nonalcoholic steatohepatitis (NASH) does not increase complications after laparoscopic bariatric surgery. Obes Surg 21(11):1714–1720
Shimizu H, Phuong V, Maia M, Kroh M, Chand B, Schauer P, Brethauer S (2013) Bariatric surgery in patients with cirrhosis. Surg Obes Relat Dis 9(1):1–6
Dallal R, Mattar S, Lord J, Watson A, Cottam D, Eid G (2004) Results of laparoscopic gastric bypass in patients with cirrhosis. Obes Surg 14(1):47–53
Mosko JD, Nguyen GC (2011) Increased perioperative mortality following bariatric surgery among patients with cirrhosis. Clin Gastroenterol Hepatol 9(10):897–901
Takata M, Campos G, Ciovica R, Rabl C, Rogers S, Cello J (2008) Laparoscopic bariatric surgery improves candidacy in morbidly obese patients awaiting transplantation. Surg Obes Relat Dis 4(2):159–164
Disclosures
There are no conflicts of interests to disclose.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Elnahas, A., Nguyen, G.C., Okrainec, A. et al. The effect of underlying liver disease on short-term outcomes following bariatric surgery. Surg Endosc 28, 2708–2712 (2014). https://doi.org/10.1007/s00464-014-3532-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-014-3532-8