Abstract
Background
Laparoscopic cholecystectomy (LC) seems to be more challenging in males than in females. The surgery seems to be longer in male patients. There also seems to be an increased rate of conversion to open surgery in male patients. We sought to objectively verify this widespread belief.
Methods
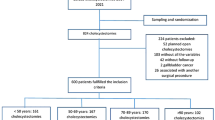
We performed a retrospective analysis of laparoscopic cholecystectomies performed between January 2004 and November 2009 in our hospital. Within this period 1844 cholecystectomies were performed in our community-based hospital. After a strict inclusion procedure, 1571 cases of LC for symptomatic gallbladder disease were analyzed (501 males, 1071 females). The time for surgery, defined as the interval from placement of the Veress needle to wound closure in minutes, and the rate of conversion to open surgery were the main parameters considered.
Results
The time for surgery in male patients was significantly longer compared to that for females (p < 0.0001). The male cohort was significantly older than the female cohort at the time of surgery (p < 0.001). The rate of conversion to open surgery was significantly higher in male patients (5.6%) compared to 2.9% for females (p < 0.0001).
Conclusion
Based on our analysis, LC had a significantly longer duration of surgery in the male cohort. The rate of conversion to open surgery was also significantly higher in male cohort. Thus, LC could be more challenging in male patients.




Similar content being viewed by others
References
Attili F, Carulli N, Roda E, Barbara B, Capocaccia L, Menotti A, Okoliksanyi L, Ricci G, Capocaccia R, Festi D, Lalloni L, Mariotti S, Sama C, Scafato E, M.I.COL Group (1995) Epidemiology of gallstone disease in Italy: prevalence data of the Multicenter Italian Study on Cholelithiasis (M.I.COL). Am J Epidemiol 141(2):158–165
Acalovschi M (2001) Cholesterol gallstones: from epidemiology to prevention. Postgrad Med J 77(906):221–229
Bateson MC (2000) Gallstones and cholecystectomy in modern Britain. Postgrad Med J 76(901):700–703
Shaffer EA (2005) Epidemiology and risk factors for gallstone disease: has the paradigm changed in the 21st century? Curr Gastroenterol Rep 7:132–140
Balzer K, Goebell H, Breuer N, Rü** KW, Leder LD (1986) Epidemiology of gallstones in a German industrial town (Essen) from 1940–1975. Digestion 33:189–197
Diehl AK (1991) Epidemiology and natural history of gallstone disease. Gastroenterol Clin North Am 20(1):1–19
Heaton KW, Braddon FE, Mountford RA, Hughes AO, Emmett PM (1991) Symptomatic and silent gall stones in the community. Gut 32:316–320
Strasberg SM (2008) Acute calculous cholecystitis. N Engl J Med 358(26):2804–2811
Afdhal NH (2007) Diseases of the gallbladder and bile ducts. In: Goldman L, Ausiello D (eds) Cecil textbook of medicine, 23rd edn. Saunders Elsevier, Philadelphia, Chap 159, pp 1152–1164
Fink-Bennett D, Freitas JE, Ripley SD, Bree RL (1985) The sensitivity of hepatobiliary imaging and real-time ultrasonography in the detection of acute cholecystitis. Arch Surg 120:904–906
Miller DR, Egbert RM, Braunstein P (1984) Comparison of ultrasound and hepatobiliary imaging in the early detection of acute total common bile duct obstruction. Arch Surg 119:1233–1237
Gurusamy KS, Samraj K (2007) Cholecystectomy versus no cholecystectomy in patients with silent gallstones. Cochrane Database Syst Rev 1:CD006230
Rehfuss ME (1936) Medical treatment of gall bladder disease. Am J Dig Dis 3(1):66–68
Eldar S, Sabo E, Nash E, Abrahanson J, Matter I (1997) Laparoscopic versus open cholecystectomy in acute cholecystits. Surg Laparosc Endosc 7(5):407–414
Chang TC, Lin MT, Wu MH, Wang MY, Lee PH (2009) Evaluation of early versus delayed laparoscopic cholecystectomy in the treatment of acute cholecystitis. Hepatogastroenterology 56(89):26–28
Keus F, Gooszen HG, Van Laarhoven CJ (2009) Systematic review: open, small-incision or laparoscopic cholecystectomy for symptomatic cholecystolithiasis. Aliment Pharmacol Ther 29(4):359–378
Keus F, de Jong JA, Gooszen HG, van Laarhoven CJ (2006) Laparoscopic versus open cholecystectomy for patients with symptomatic cholecystolithiasis. Cochrane Database Syst Rev 18(4):CD006231
Rivas H, Varela E, Scott D (2010) Single-incision laparoscopic cholecystectomy: initial evaluation of a large series of patients. Surg Endosc 24(6):1403–1412
Ponsky TA (2009) Single port laparoscopic cholecystectomy in adults and children: tools and techniques. J Am Coll Surg 209(5):e1–e6
Bucher P, Pugin F, Morel P (2010) From single-port access to laparoendoscopic single-site cholecystectomy. Surg Endosc 24(1):234–235
Salinas G, Saavedra L, Agurto H, Quispe R, Ramírez E, Grande J, Tamayo J, Sánchez V, Málaga D, Marks JM (2010) Early experience in human hybrid transgastric and transvaginal endoscopic cholecystectomy. Surg Endosc 24(5):1092–1098
Schlager A, Khalaileh A, Shussman N, Elazary R, Keidar A, Pikarsky AJ, Ben-Shushan A, Shibolet O, Horgan S, Talamini M, Zamir G, Rivkind AI, Mintz Y (2010) Providing more through less: current methods of retraction in SIMIS and NOTES cholecystectomy. Surg Endosc 24(7):1542–1546
Mann HB, Withney DR (1947) On a test of whether one of 2 random variables is stochastically larger than the other. Ann Math Stat 18:50–61
Ibrahim S, Hean TK, Ho LS, Ravintharan T, Chye TN, Chee CH (2006) Risk factors for conversion to open surgery in patients undergoing laparoscopic cholecystectomy. World J Surg 30(9):1698–1704
Pavlidis TE, Marakis GN, Symeonidis N, Psarras K, Ballas K, Rafailidis S, Sakantamis AK (2008) Considerations concerning laparoscopic cholecystectomy in the extremely elderly. J Laparoendosc Adv Surg Tech A 18(1):56–60
Annamaneni RK, Moraitis D, Cayten CG (2005) Laparoscopic cholecystectomy in the elderly. JSLS 9(4):408–410
Al-Mulhim AA (2008) Male gender is not a risk factor for the outcome of laparoscopic cholecystectomy: a single surgeon experience. Saudi J Gastroenterol 14(2):73–79
Yol S, Kartal A, Vatansev C, Aksoy F, Toy H (2006) Sex as a factor in conversion from laparoscopic cholecystectomy to open surgery. JSLS 10(3):359–363
Disclosures
Dr. Peter Ambe, Mr. Babak Janghorban Esfahani, Mr. Ibrahim Tasci, Mrs. Hildegard Christ, and Prof. Dr. Lothar Köhler have no conflicts of interest or financial ties to disclose
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Ambe, P., Esfahani, B.J., Tasci, I. et al. Is laparoscopic cholecystectomy more challenging in male patients?. Surg Endosc 25, 2236–2240 (2011). https://doi.org/10.1007/s00464-010-1539-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-010-1539-3