Abstract
Purpose
The numerous first-line treatment regimens for human epidermal growth factor receptor 2 (HER2)-positive advanced breast cancer (ABC) necessitate a comprehensive evaluation to inform clinical decision-making. We conducted a Bayesian network meta-analysis (NMA) to compare the efficacy and safety of different interventions.
Methods
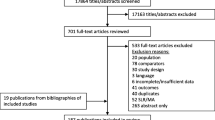
We systematically searched for relevant randomized controlled trials (RCTs) in Pubmed, Embase, Cochrane Library and online abstracts from inception to June 1, 2023. NMA was performed to calculate and analyze progression-free survival (PFS), overall survival (OS), objective response rate (ORR), and adverse events of grade 3 or higher (≥ 3 AEs).
Results
Out of the 10,313 manuscripts retrieved, we included 28 RCTs involving 11,680 patients. Regarding PFS and ORR, the combination of trastuzumab with tyrosine kinase inhibitors (TKIs) was more favorable than dual-targeted therapy. If only using trastuzumab, combination chemotherapy is superior to monochemotherapy in terms of PFS. It is important to note that the addition of anthracycline did not result in improved PFS. For patients with hormone receptor-positive HER2-positive diseases, dual-targeted combined with endocrine therapy showed better benefit in terms of PFS compared to dual-targeted alone, but it did not reach statistical significance. The comprehensive analysis of PFS and ≥ 3 AEs indicates that monochemotherapy combined with dual-targeted therapy still has the optimal balance between efficacy and safety.
Conclusion
Monochemotherapy (Docetaxel) plus dual-target (Trastuzumab and Pertuzumab) therapy remains the optimal choice among all first-line treatment options for ABC. The combination of trastuzumab with TKIs (Pyrotinib) demonstrated a significant improvement in PFS and ORR, but further data are warranted to confirm the survival benefit.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Human epidermal growth factor receptor 2 (HER2)-positive breast cancer (BC) accounts for 15–20% of all BC cases and is characterized by HER2 overexpression, aggressive tumor growth, and poor prognosis (Slamon et al. 1989). With the advent of targeted therapies, treatment outcomes for patients with HER2-positive BC have significantly improved, resulting in a 7-year disease-free survival rate of 93.3% (Romond et al. 2005; Tolaney et al. 2019). Despite standardized treatments, metastasis still occurs in 20–30% of patients with HER2-positive BC (Bear et al. 2015).
Advanced breast cancer (ABC), including both locally advanced breast cancer and metastatic breast cancer, represents a specific subgroup of breast cancer that is resistant to curative surgical interventions. Docetaxel combination with trastuzumab and pertuzumab used in CLEOPATRA trial defines the classic first-line treatment regimen for ABC (Giordano et al. 2022). However, the continuous emergence of drugs is gradually resha** the treatment landscape, these varying combinations targeted agents offer diverse benefits. For instances, the PHILA study (Xu et al. 2022), the introduction marked a significant departure from the established dual-targeted treatment paradigm for advanced settings, offering new promise for first-line therapy. This study showcased the potential of a trastuzumab and tyrosine kinase inhibitors (TKIs) combination regimen, which demonstrated a numerical advantage over dual-targeted therapy in terms of progression-free survival (PFS). Given the late emergence of pertuzumab, few clinical trials have directly compared it head-to-head with dual-targeted therapy. Consequently, there is a growing need for comprehensive comparisons of all first-line regimens to inform and guide physicians in their choice of therapeutic strategies.
Triple-positive breast cancer (TPBC) characterized as being hormone receptor (HR)-positive and HER2-positive, encompasses various subtypes including Luminal type B and HER2 overexpression type. These subtypes exhibit distinct molecular functions, biological processes, signaling pathways, and clinical behaviors. Furthermore, they demonstrate varying sensitivities to treatment and diverse intrinsic biological features, ultimately reflecting different responses to therapeutic interventions (Zhao et al. 2022).
TPBC represents a distinct clinical entity. While HER2 positivity is generally an independent predictor of poor prognosis, high HR expression is associated with a better outcome (Parise and Caggiano 2016; Kay et al. 2021). Thus, patients with HR-positive/HER2-positive status tend to have a better prognosis than their HR-negative/HER2-positive counterparts but fare worse than HR-positive/HER2-negative patients. Notably, crosstalk between the HR and HER2 pathways complicates treatment, as monochemotherapy targeting either pathway alone can lead to suboptimal results and potential drug resistance. For example, the CLEOPATRA study (Swain et al. 2020) showed reduced benefits from dual-targeted chemotherapy in HR-positive patients compared to HR-negative patients. The BIG 1–98 study (Rasmussen et al. 2008) reported poorer outcomes for patients with HER2-positive BC treated with endocrine therapy alone. Our analysis indicates that combining dual-targeted therapy with endocrine therapy yields the highest SUCRA of PFS for TPBC patients, outperforming both monochemotherapy plus dual-targeted and monochemotherapy plus single-targeted and endocrine therapy (Fig. 5B). Although this recommendation is based on data from the phase II PERTAIN trial (Rimawi et al. 2018) alone, it is supported by findings from the MonarcHER (André et al. 2022) and SYSUCC-002 (Hua et al. 2022) studies, suggesting that this combined approach represents a promising and effective strategy for managing TPBC.
For patients with cardiac comorbidity or risk factors for heart disease, cardiac function testing is required to exclude contraindications for trastuzumab and anthracycline drugs. Our research has found that T-DM1, which has no significant cardiac toxicity, is a good alternative for such patients (Fig. 6).
While improved PFS is a notable outcome, it is not a definitive marker of treatment effectiveness unless it translates into a benefit in OS (Adunlin et al. 2015). Unfortunately, only the regimen of monochemotherapy plus dual-targeted therapy is currently benefiting on the OS (Supplemental File D3). We acknowledge that the OS data in many of these studies remain immature due to the lengthy process of OS data collection. As a result, only OS results from a small number of studies were included in our current analysis. We anticipate future research that comprehensively evaluates treatment options from the perspective of OS.
Limitations
All of our studies enrolled RCTs to improve accuracy and reliability and utilized PFS, OS, ORR and ≥ 3 AEs to comprehensively assess the efficacy and safety of the regimens. It was also analyzed for the triple-positive subgroup. But our study still have some shortcomings: we excluded single-arm studies to form a closed loop; Some studies did not publish information on randomization and allocation methods, which can lead to potential bias; Some studies did not include all endpoints, or the endpoints were immature, and our analysis based on existing published data would have resulted in potential bias; Some studies enrolled patients on first and second line treatments, and it was not possible to extract data on first-line treatments separately.
Conclusion
This NMA utilizing Bayesian modeling provides valuable insights into the first-line treatment options for HER2-positive ABC. Monochemotherapy (Docetaxel) plus dual-target (Trastuzumab and Pertuzumab) therapy emerged as the optimal choice based on their efficacy outcomes of OS and a comprehensive analysis of both PFS and ≥ 3 AEs. Additionally, the combination of trastuzumab with TKIs (Pyrotinib) offered a more favorable PFS and ORR, but further data are warranted to confirm the survival benefit.
Data availability
All data generated or analyzed during this study are included in the supplemental file of this published article.
Abbreviations
- HER2:
-
Human epidermal growth factor receptor 2
- BC:
-
Breast cancer
- ABC:
-
Advanced breast cancer
- TKIs:
-
Tyrosine kinase inhibitors
- PFS:
-
Progression-free survival
- TPBC:
-
Triple-positive breast cancer
- HR:
-
Hormone receptor
- RCTs:
-
Randomized controlled trials
- NMA:
-
Network meta-analysis
- PRISMA:
-
Preferred Reporting Items for Systematic reviews and Meta-analyses
- SABCS:
-
San Antonio Breast Cancer Symposium
- ASCO:
-
American Society of Clinical Oncology
- ESMO:
-
European Society for Medical Oncology
- OS:
-
Overall survival
- ORR:
-
Objective response rate
- ≥ 3 AEs:
-
Adverse events of grade 3 or higher
- HazR:
-
Hazard ratio
- CI:
-
Confidence Interval
- OR:
-
Odd ratio
- SUCRA:
-
Surface under the cumulative ranking curve
- ADC:
-
Antibody-drug conjugate
References
Adunlin G, Cyrus JW, Dranitsaris G (2015) Correlation between progression-free survival and overall survival in metastatic breast cancer patients receiving anthracyclines, taxanes, or targeted therapies: a trial-level meta-analysis. Breast Cancer Res Treat 154:591–608
André F, Nadal JC, Denys H, Goel S, Litchfield LM, Appiah A, Chen Y, Tolaney SM (2022) LBA18 Final overall survival (OS) for abemaciclib plus trastuzumab +/- fulvestrant versus trastuzumab plus chemotherapy in patients with HR+, HER2+ advanced breast cancer (monarcHER): a randomized, open-label, phase II trial. Ann Oncol 33:S1386–S1387
Awada A, Colomer R, Inoue K, Bondarenko I, Badwe RA, Demetriou G, Lee SC, Mehta AO, Kim SB, Bachelot T, Goswami C, Deo S, Bose R, Wong A, Xu F, Yao B, Bryce R, Carey LA (2016) Neratinib plus paclitaxel vs trastuzumab plus paclitaxel in previously untreated metastatic ERBB2-positive breast cancer: the NEfERT-T randomized clinical trial. JAMA Oncol 2:1557–1564
Baselga J, Manikhas A, Cortés J, Llombart A, Roman L, Semiglazov VF, Byakhov M, Lokanatha D, Forenza S, Goldfarb RH, Matera J, Azarnia N, Hudis CA, Rozencweig M (2019) Phase III trial of nonpegylated liposomal doxorubicin in combination with trastuzumab and paclitaxel in HER2-positive metastatic breast cancer. Ann Oncol 30:1017
Bear HD, Tang G, Rastogi P, Geyer CE Jr, Liu Q, Robidoux A, Baez-Diaz L, Brufsky AM, Mehta RS, Fehrenbacher L, Young JA, Senecal FM, Gaur R, Margolese RG, Adams PT, Gross HM, Costantino JP, Paik S, Swain SM, Mamounas EP, Wolmark N (2015) Neoadjuvant plus adjuvant bevacizumab in early breast cancer (NSABP B-40 [NRG Oncology]): secondary outcomes of a phase 3, randomised controlled trial. Lancet Oncol 16:1037–1048
Doi T, Shitara K, Naito Y, Shimomura A, Fujiwara Y, Yonemori K, Shimizu C, Shimoi T, Kuboki Y, Matsubara N, Kitano A, Jikoh T, Lee C, Fujisaki Y, Ogitani Y, Yver A, Tamura K (2017) Safety, pharmacokinetics, and antitumour activity of trastuzumab deruxtecan (DS-8201), a HER2-targeting antibody-drug conjugate, in patients with advanced breast and gastric or gastro-oesophageal tumours: a phase 1 dose-escalation study. Lancet Oncol 18:1512–1522
Gasparini G, Gion M, Mariani L, Papaldo P, Crivellari D, Filippelli G, Morabito A, Silingardi V, Torino F, Spada A, Zancan M, De Sio L, Caputo A, Cognetti F, Lambiase A, Amadori D (2007) Randomized Phase II Trial of weekly paclitaxel alone versus trastuzumab plus weekly paclitaxel as first-line therapy of patients with Her-2 positive advanced breast cancer. Breast Cancer Res Treat 101:355–365
Gelmon KA, Boyle FM, Kaufman B, Huntsman DG, Manikhas A, Di Leo A, Martin M, Schwartzberg LS, Lemieux J, Aparicio S, Shepherd LE, Dent S, Ellard SL, Tonkin K, Pritchard KI, Whelan TJ, Nomikos D, Nusch A, Coleman RE, Mukai H, Tjulandin S, Khasanov R, Rizel S, Connor AP, Santillana SL, Chapman JA, Parulekar WR (2015) Lapatinib or trastuzumab plus taxane therapy for human epidermal growth factor receptor 2-positive advanced breast cancer: final results of NCIC CTG MA.31. J Clin Oncol 33:1574–1583
Gianni L, Romieu GH, Lichinitser M, Serrano SV, Mansutti M, Pivot X, Mariani P, Andre F, Chan A, Lipatov O, Chan S, Wardley A, Greil R, Moore N, Prot S, Pallaud C, Semiglazov V (2013) AVEREL: a randomized phase III Trial evaluating bevacizumab in combination with docetaxel and trastuzumab as first-line therapy for HER2-positive locally recurrent/metastatic breast cancer. J Clin Oncol 31:1719–1725
Gianni L, Pienkowski T, Im YH, Tseng LM, Liu MC, Lluch A, Starosławska E, de la Haba-Rodriguez J, Im SA, Pedrini JL, Poirier B, Morandi P, Semiglazov V, Srimuninnimit V, Bianchi GV, Magazzù D, McNally V, Douthwaite H, Ross G, Valagussa P (2016) 5-year analysis of neoadjuvant pertuzumab and trastuzumab in patients with locally advanced, inflammatory, or early-stage HER2-positive breast cancer (NeoSphere): a multicentre, open-label, phase 2 randomised trial. Lancet Oncol 17:791–800
Giordano SH, Franzoi MAB, Temin S, Anders CK, Chandarlapaty S, Crews JR, Kirshner JJ, Krop IE, Lin NU, Morikawa A, Patt DA, Perlmutter J, Ramakrishna N, Davidson NE (2022) Systemic therapy for advanced human epidermal growth factor receptor 2-positive breast cancer: ASCO guideline update. J Clin Oncol 40:2612–2635
Guan Z, Xu B, DeSilvio ML, Shen Z, Arpornwirat W, Tong Z, Lorvidhaya V, Jiang Z, Yang J, Makhson A, Leung WL, Russo MW, Newstat B, Wang L, Chen G, Oliva C, Gomez H (2013) Randomized trial of lapatinib versus placebo added to paclitaxel in the treatment of human epidermal growth factor receptor 2-overexpressing metastatic breast cancer. J Clin Oncol 31:1947–1953
Hua X, Bi XW, Zhao JL, Shi YX, Lin Y, Wu ZY, Zhang YQ, Zhang LH, Zhang AQ, Huang H, Liu XM, Xu F, Guo Y, **a W, Hong RX, Jiang KK, Xue C, An X, Zhong YY, Wang SS, Huang JJ, Yuan ZY (2022) Trastuzumab plus endocrine therapy or chemotherapy as first-line treatment for patients with hormone receptor-positive and HER2-positive metastatic breast cancer (SYSUCC-002). Clin Cancer Res 28:637–645
Huober J, Fasching PA, Barsoum M, Petruzelka L, Wallwiener D, Thomssen C, Reimer T, Paepke S, Azim HA, Ragosch V, Kubista E, Baumgärtner AK, Beckmann MW, May C, Nimmrich I, Harbeck N (2012) Higher efficacy of letrozole in combination with trastuzumab compared to letrozole monotherapy as first-line treatment in patients with HER2-positive, hormone-receptor-positive metastatic breast cancer - results of the eLEcTRA trial. Breast 21:27–33
Hurvitz SA, Andre F, Jiang Z, Shao Z, Mano MS, Neciosup SP, Tseng LM, Zhang Q, Shen K, Liu D, Dreosti LM, Burris HA, Toi M, Buyse ME, Cabaribere D, Lindsay MA, Rao S, Pacaud LB, Taran T, Slamon D (2015) Combination of everolimus with trastuzumab plus paclitaxel as first-line treatment for patients with HER2-positive advanced breast cancer (BOLERO-1): a phase 3, randomised, double-blind, multicentre trial. Lancet Oncol 16:816–829
Hurvitz SA, Hegg R, Chung WP, Im SA, Jacot W, Ganju V, Chiu JWY, Xu B, Hamilton E, Madhusudan S, Iwata H, Altintas S, Henning JW, Curigliano G, Perez-Garcia JM, Kim SB, Petry V, Huang CS, Li W, Frenel JS, Antolin S, Yeo W, Bianchini G, Loi S, Tsurutani J, Egorov A, Liu Y, Cathcart J, Ashfaque S, Cortés J (2023) Trastuzumab deruxtecan versus trastuzumab emtansine in patients with HER2-positive metastatic breast cancer: updated results from DESTINY-Breast03, a randomised, open-label, phase 3 trial. Lancet 401:105–117
Johnston S, Pippen J Jr, Pivot X, Lichinitser M, Sadeghi S, Dieras V, Gomez HL, Romieu G, Manikhas A, Kennedy MJ, Press MF, Maltzman J, Florance A, O’Rourke L, Oliva C, Stein S, Pegram M (2009) Lapatinib combined with letrozole versus letrozole and placebo as first-line therapy for postmenopausal hormone receptor-positive metastatic breast cancer. J Clin Oncol 27:5538–5546
Kaufman B, Mackey JR, Clemens MR, Bapsy PP, Vaid A, Wardley A, Tjulandin S, Jahn M, Lehle M, Feyereislova A, Révil C, Jones A (2009) Trastuzumab plus anastrozole versus anastrozole alone for the treatment of postmenopausal women with human epidermal growth factor receptor 2-positive, hormone receptor-positive metastatic breast cancer: results from the randomized phase III TAnDEM study. J Clin Oncol 27:5529–5537
Kay C, Martínez-Pérez C, Meehan J, Gray M, Webber V, Dixon JM, Turnbull AK (2021) Current trends in the treatment of HR+/HER2+ breast cancer. Future Oncol 17:1665–1681
Li T, Puhan MA, Vedula SS, Singh S, Dickersin K (2011) Network meta-analysis-highly attractive but more methodological research is needed. BMC Med 9:79
Li X, Yang C, Wan H, Zhang G, Feng J, Zhang L, Chen X, Zhong D, Lou L, Tao W, Zhang L (2017) Discovery and development of pyrotinib: A novel irreversible EGFR/HER2 dual tyrosine kinase inhibitor with favorable safety profiles for the treatment of breast cancer. Eur J Pharm Sci 110:51–61
Li RK, Tokunaga E, Adamchuk H, Vladimirov V, Yanez E, Lee KS, Bondarenko I, Vana A, Hilton F, Ishikawa T, Tajima K, Lipatov O (2022) Long-term safety and effectiveness of PF-05280014 (a Trastuzumab Biosimilar) treatment in patients with HER2-positive metastatic breast cancer: updated results of a randomized double-blind study. BioDrugs 36:55–69
Llombart-Cussac A, Cortés J, Paré L, Galván P, Bermejo B, Martínez N, Vidal M, Pernas S, López R, Muñoz M, Nuciforo P, Morales S, Oliveira M, de la Peña L, Peláez A, Prat A (2017) HER2-enriched subtype as a predictor of pathological complete response following trastuzumab and lapatinib without chemotherapy in early-stage HER2-positive breast cancer (PAMELA): an open-label, single-group, multicentre, phase 2 trial. Lancet Oncol 18:545–554
Marty M, Cognetti F, Maraninchi D, Snyder R, Mauriac L, Tubiana-Hulin M, Chan S, Grimes D, Antón A, Lluch A, Kennedy J, O’Byrne K, Conte P, Green M, Ward C, Mayne K, Extra JM (2005) Randomized phase II trial of the efficacy and safety of trastuzumab combined with docetaxel in patients with human epidermal growth factor receptor 2-positive metastatic breast cancer administered as first-line treatment: the M77001 study group. J Clin Oncol 23:4265–4274
Morikawa A, Peereboom DM, Thorsheim HR, Samala R, Balyan R, Murphy CG, Lockman PR, Simmons A, Weil RJ, Tabar V, Steeg PS, Smith QR, Seidman AD (2015) Capecitabine and lapatinib uptake in surgically resected brain metastases from metastatic breast cancer patients: a prospective study. Neuro-Oncol 17:289–295
Murthy RK, Loi S, Okines A, Paplomata E, Hamilton E, Hurvitz SA, Lin NU, Borges V, Abramson V, Anders C, Bedard PL, Oliveira M, Jakobsen E, Bachelot T, Shachar SS, Müller V, Braga S, Duhoux FP, Greil R, Cameron D, Carey LA, Curigliano G, Gelmon K, Hortobagyi G, Krop I, Loibl S, Pegram M, Slamon D, Palanca-Wessels MC, Walker L, Feng W, Winer EP (2020) Tucatinib, trastuzumab, and capecitabine for HER2-positive metastatic breast cancer. N Engl J Med 382:597–609
Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, Shamseer L, Tetzlaff JM, Akl EA, Brennan SE, Chou R, Glanville J, Grimshaw JM, Hróbjartsson A, Lalu MM, Li T, Loder EW, Mayo-Wilson E, McDonald S, McGuinness LA, Stewart LA, Thomas J, Tricco AC, Welch VA, Whiting P, Moher D (2021) The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ 372:n71
Parise C, Caggiano V (2016) Breast cancer mortality among Asian-American Women in California: variation according to ethnicity and tumor subtype. J Breast Cancer 19:112–121
Perez EA, Hurvitz SA, Amler LC, Mundt KE, Ng V, Guardino E, Gianni L (2014) Relationship between HER2 expression and efficacy with first-line trastuzumab emtansine compared with trastuzumab plus docetaxel in TDM4450g: a randomized phase II study of patients with previously untreated HER2-positive metastatic breast cancer. Breast Cancer Res 16:R50
Perez EA, Barrios C, Eiermann W, Toi M, Im YH, Conte P, Martin M, Pienkowski T, Pivot XB, Burris HA 3rd, Petersen JA, De Haas S, Hoersch S, Patre M, Ellis PA (2019) Trastuzumab emtansine with or without pertuzumab versus trastuzumab with taxane for human epidermal growth factor receptor 2-positive advanced breast cancer: Final results from MARIANNE. Cancer 125:3974–3984
Pivot X, Cortés J, Lüftner D, Lyman GH, Curigliano G, Bondarenko IM, Ahn JH, Im SA, Litwiniuk M, Shparyk YV, Ho GF, Kislov NV, Wojtukiewicz M, Sarosiek T, Chae YS, Ahn JS, Jang H, Kim S, Lee J, Yoon Y (2023) Cardiac safety and efficacy of SB3 trastuzumab biosimilar for ERBB2-positive early breast cancer: secondary analysis of a randomized clinical trial. JAMA Netw Open 6:e235822
Rasmussen BB, Regan MM, Lykkesfeldt AE, Dell’Orto P, Del Curto B, Henriksen KL, Mastropasqua MG, Price KN, Méry E, Lacroix-Triki M, Braye S, Altermatt HJ, Gelber RD, Castiglione-Gertsch M, Goldhirsch A, Gusterson BA, Thürlimann B, Coates AS, Viale G (2008) Adjuvant letrozole versus tamoxifen according to centrally-assessed ERBB2 status for postmenopausal women with endocrine-responsive early breast cancer: supplementary results from the BIG 1–98 randomised trial. Lancet Oncol 9:23–28
Rimawi M, Ferrero JM, de la Haba-Rodriguez J, Poole C, De Placido S, Osborne CK, Hegg R, Easton V, Wohlfarth C, Arpino G (2018) First-line trastuzumab plus an aromatase inhibitor, with or without pertuzumab, in human epidermal growth factor receptor 2-positive and hormone receptor-positive metastatic or locally advanced breast cancer (PERTAIN): a randomized open-label phase II trial. J Clin Oncol 36:2826–2835
Robert N, Leyland-Jones B, Asmar L, Belt R, Ilegbodu D, Loesch D, Raju R, Valentine E, Sayre R, Cobleigh M, Albain K, McCullough C, Fuchs L, Slamon D (2006) Randomized phase III study of trastuzumab, paclitaxel, and carboplatin compared with trastuzumab and paclitaxel in women with HER-2-overexpressing metastatic breast cancer. J Clin Oncol 24:2786–2792
Romond EH, Perez EA, Bryant J, Suman VJ, Geyer CE Jr, Davidson NE, Tan-Chiu E, Martino S, Paik S, Kaufman PA, Swain SM, Pisansky TM, Fehrenbacher L, Kutteh LA, Vogel VG, Visscher DW, Yothers G, Jenkins RB, Brown AM, Dakhil SR, Mamounas EP, Lingle WL, Klein PM, Ingle JN, Wolmark N (2005) Trastuzumab plus adjuvant chemotherapy for operable HER2-positive breast cancer. N Engl J Med 353:1673–1684
Rugo HS, Pennella EJ, Gopalakrishnan U, Hernandez-Bronchud M, Herson J, Koch HF, Loganathan S, Deodhar S, Marwah A, Manikhas A, Bondarenko I, Mukhametshina G, Nemsadze G, Parra JD, Abesamis-Tiambeng MLT, Baramidze K, Akewanlop C, Vynnychenko I, Sriuranpong V, Mamillapalli G, Roy S, Yanez Ruiz EP, Barve A, Fuentes-Alburo A, Waller CF (2021) Final overall survival analysis of the phase 3 HERITAGE study demonstrates equivalence of trastuzumab-dkst to trastuzumab in HER2-positive metastatic breast cancer. Breast Cancer Res Treat 188:369–377
Shao Z, Pang D, Yang H, Li W, Wang S, Cui S, Liao N, Wang Y, Wang C, Chang YC, Wang H, Kang SY, Seo JH, Shen K, Laohawiriyakamol S, Jiang Z, Li J, Zhou J, Althaus B, Mao Y, Eng-Wong J (2020) Efficacy, safety, and tolerability of pertuzumab, trastuzumab, and docetaxel for patients with early or locally advanced ERBB2-positive breast cancer in Asia: the PEONY phase 3 randomized clinical trial. JAMA Oncol 6:e193692
Slamon DJ, Godolphin W, Jones LA, Holt JA, Wong SG, Keith DE, Levin WJ, Stuart SG, Udove J, Ullrich A et al (1989) Studies of the HER-2/neu proto-oncogene in human breast and ovarian cancer. Science 244:707–712
Slamon DJ, Leyland-Jones B, Shak S, Fuchs H, Paton V, Bajamonde A, Fleming T, Eiermann W, Wolter J, Pegram M, Baselga J, Norton L (2001) Use of chemotherapy plus a monoclonal antibody against HER2 for metastatic breast cancer that overexpresses HER2. N Engl J Med 344:783–792
Swain SM, Miles D, Kim SB, Im YH, Im SA, Semiglazov V, Ciruelos E, Schneeweiss A, Loi S, Monturus E, Clark E, Knott A, Restuccia E, Benyunes MC, Cortés J (2020) Pertuzumab, trastuzumab, and docetaxel for HER2-positive metastatic breast cancer (CLEOPATRA): end-of-study results from a double-blind, randomised, placebo-controlled, phase 3 study. Lancet Oncol 21:519–530
Tolaney SM, Guo H, Pernas S, Barry WT, Dillon DA, Ritterhouse L, Schneider BP, Shen F, Fuhrman K, Baltay M, Dang CT, Yardley DA, Moy B, Marcom PK, Albain KS, Rugo HS, Ellis MJ, Shapira I, Wolff AC, Carey LA, Overmoyer B, Partridge AH, Hudis CA, Krop IE, Burstein HJ, Winer EP (2019) Seven-Year Follow-up analysis of adjuvant paclitaxel and trastuzumab trial for node-negative, human epidermal growth factor receptor 2-positive breast cancer. J Clin Oncol 37:1868–1875
Tolaney SM, Romualdo BS, Zefei J, Yeon HP, Mothaffar R, Cristina S, Andreas S, Masakazu T, Tinghui Y, Jagdish S, Pia H, Sibylle L (2022) Abstract OT1-14-02: Phase 3 study of trastuzumab deruxtecan (T-DXd) with or without pertuzumab vs a taxane, trastuzumab and pertuzumab in first-line (1L), human epidermal growth factor receptor 2-positive (HER2+) metastatic breast cancer (mBC): DESTINY-Breast09. Cancer Res 82:1402
Valero V, Forbes J, Pegram MD, Pienkowski T, Eiermann W, von Minckwitz G, Roche H, Martin M, Crown J, Mackey JR, Fumoleau P, Rolski J, Mrsic-Krmpotic Z, Jagiello-Gruszfeld A, Riva A, Buyse M, Taupin H, Sauter G, Press MF, Slamon DJ (2011) Multicenter phase III randomized trial comparing docetaxel and trastuzumab with docetaxel, carboplatin, and trastuzumab as first-line chemotherapy for patients with HER2-gene-amplified metastatic breast cancer (BCIRG 007 study): two highly active therapeutic regimens. J Clin Oncol 29:149–156
Wang X, Huang J (2022) 239P Pyrotinib in combination with docetaxel as first-line treatment for HER2-positive metastatic breast cancer (PANDORA): a single-arm, multicenter phase II trial. Ann Oncol 33:S646–S647
Wardley AM, Pivot X, Morales-Vasquez F, Zetina LM, de Fátima Dias M, Gaui DO, Reyes J, Jassem C, Barton P, Button VH, Torres AA (2010) Randomized phase II trial of first-line trastuzumab plus docetaxel and capecitabine compared with trastuzumab plus docetaxel in HER2-positive metastatic breast cancer. J Clin Oncol 28:976–983
Wu J, Jiang Z, Liu Z, Yang B, Yang H, Tang J, Wang K, Liu Y, Wang H, Fu P, Zhang S, Liu Q, Wang S, Huang J, Wang C, Wang S, Wang Y, Zhen L, Zhu X, Wu F, Lin X, Zou J (2022) Neoadjuvant pyrotinib, trastuzumab, and docetaxel for HER2-positive breast cancer (PHEDRA): a double-blind, randomized phase 3 trial. BMC Med 20:498
Xu B, Yan M, Ma F, Hu X, Feng J, Ouyang Q, Tong Z, Li H, Zhang Q, Sun T, Wang X, Yin Y, Cheng Y, Li W, Gu Y, Chen Q, Liu J, Cheng J, Geng C, Qin S, Wang S, Lu J, Shen K, Liu Q, Wang X, Wang H, Luo T, Yang J, Wu Y, Yu Z, Zhu X, Chen C, Zou J (2021a) Pyrotinib plus capecitabine versus lapatinib plus capecitabine for the treatment of HER2-positive metastatic breast cancer (PHOEBE): a multicentre, open-label, randomised, controlled, phase 3 trial. Lancet Oncol 22:351–360
Xu B, Zhang Q, Sun T, Li W, Teng Y, Hu X, Bondarenko I, Adamchuk H, Zhang L, Trukhin D, Wang S, Zheng H, Tong Z, Shparyk Y, Wang Q (2021b) Efficacy, safety, and immunogenicity of HLX02 compared with reference trastuzumab in patients with recurrent or metastatic HER2-positive breast cancer: a randomized phase III equivalence trial. BioDrugs 35:337–350
Xu B, Yan M, Ma F, Li W, Ouyang Q, Tong Z, Teng Y, Wang S, Wang Y, Geng C, Luo T, Zhong J, Zhang Q, Liu Q, Zeng X, Sun T, Mo Q, Dong F, Wu S, Zhu X (2022) LBA19 Pyrotinib or placebo in combination with trastuzumab and docetaxel for HER2-positive metastatic breast cancer (PHILA): A randomized phase III trial. Ann Oncol 33:1387
Xu B, Li W, Zhang Q, Li Q, Wang X, Li H, Sun T, Yin Y, Zheng H, Feng J, Zhu H, Siddiqui A, Macharia H, Knott A (2023) Pertuzumab, trastuzumab, and docetaxel for Chinese patients with previously untreated HER2-positive locally recurrent or metastatic breast cancer (PUFFIN): final analysis of a phase III, randomized, double-blind, placebo-controlled study. Breast Cancer Res Treat 197:503–513
Zhao S, Liu XY, ** X, Ma D, **ao Y, Shao ZM, Jiang YZ (2019) Molecular portraits and trastuzumab responsiveness of estrogen receptor-positive, progesterone receptor-positive, and HER2-positive breast cancer. Theranostics 9:4935–4945
Funding
The authors declare that no funds, grants, or other support were received during the preparation of this manuscript.
Author information
Authors and Affiliations
Contributions
ZJ and SCG conceived the study. WJX and YYS had full access to all the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis. WJX and ZJ designed the search strategy. WJX and YYS screened the abstracts and full texts, acquired the data, and judged the risk of bias in the studies. WJX and LQS performed data analyses. WJX wrote the first draft of this manuscript. ZJ and SCG critically revised the manuscript. All the authors have approved the final version of the manuscript. All authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Conflict of interest
The authors have no relevant financial or non-financial interests to disclose.
Ethical approval
The Ethics Committee of the College of Clinical Oncology of Fujian Medical University has confirmed that no ethical approval is required.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Wang, J., Yu, Y., Lin, Q. et al. Efficacy and safety of first-line therapy in patients with HER2-positive advanced breast cancer: a network meta-analysis of randomized controlled trials. J Cancer Res Clin Oncol 150, 21 (2024). https://doi.org/10.1007/s00432-023-05530-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00432-023-05530-3