Abstract
Purpose
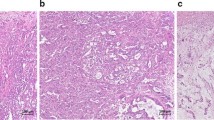
Liver metastases are the major cause of cancer-related death in colorectal cancer patients with a tendency to recur in over 50 % of the cases even after curatively intended surgery. Prognosis after liver resection, however, can neither be based on macroscopic or light microscopic evaluation of the metastases nor on clinical data alone. This is a pilot study in order to determine a potential influence of chromosomal aberrations on overall survival and relapse rate after curative liver resection.
Methods
Twenty randomly selected cases (10 patients with a survival of more and 10 patients with a survival of less than 5 years after resection) were studied by array comparative genomic hybridization.
Results
The distributions concerning age, gender, stage and grading of primary tumor, percentage of patients with chemotherapy, number and distribution of the liver metastases, Nordlinger and Fong scores showed no differences between long- and short-term survivors and no correlation to any chromosomal aberration. However, the relapse rate of patients with (partial) monosomy 4 was lower and the long-time survival better than in the other patients.
Conclusions
Loss of chromosome 4 in colorectal liver metastases seems not only to be associated with the progression of the primary tumor as reported in the literature, but also with the long-term survival and the cumulative relapse rate after complete resection of colorectal liver metastases.



Similar content being viewed by others
References
Blazer DG 3rd, Kishi Y et al (2008) Pathologic response to preoperative chemotherapy: a new outcome end point after resection of hepatic colorectal metastases. J Clin Oncol 26(33):5344–5351
Brosens RP, Belt EJ et al (2010) Deletion of chromosome 4q predicts outcome in stage II colon cancer patients. Anal Cell Pathol 33(2):95–104
Bruin SC, Klijn C et al (2010) Specific genomic aberrations in primary colorectal cancer are associated with liver metastases. BMC Cancer 10:662
Chua TC, Saxena A et al (2010) Systematic review of randomized and nonrandomized trials of the clinical response and outcomes of neoadjuvant systemic chemotherapy for resectable colorectal liver metastases. Ann Surg Oncol 17(2):492–501
de Haas RJ, Wicherts DA et al (2010) Tumor marker evolution: comparison with imaging for assessment of response to chemotherapy in patients with colorectal liver metastases. Ann Surg Oncol 17(4):1010–1023
Diep CB, Kleivi K et al (2006) The order of genetic events associated with colorectal cancer progression inferred from meta-analysis of copy number changes. Genes Chromosom Cancer 45(1):31–41
Fong Y, Fortner J et al (1999) Clinical score for predicting recurrence after hepatic resection for metastatic colorectal cancer: analysis of 1001 consecutive cases. Ann Surg 230(3):309–318 (discussion 318–321)
Gordon KJ, Kirkbride KC et al (2009) Bone morphogenetic proteins induce pancreatic cancer cell invasiveness through a Smad1-dependent mechanism that involves matrix metalloproteinase-2. Carcinogenesis 30(2):238–248
Iwatsuki S, Dvorchik I et al (1999) Hepatic resection for metastatic colorectal adenocarcinoma: a proposal of a prognostic scoring system. J Am Coll Surg 189(3):291–299
Knosel T, Schluns K et al (2004) Chromosomal alterations during lymphatic and liver metastasis formation of colorectal cancer. Neoplasia 6(1):23–28
Koch M, Kienle P et al (2005) Detection of hematogenous tumor cell dissemination predicts tumor relapse in patients undergoing surgical resection of colorectal liver metastases. Ann Surg 241(2):199–205
Konopke R, Kersting S et al (2009) Prognostic factors and evaluation of a clinical score for predicting survival after resection of colorectal liver metastases. Liver Int 29(1):89–102
Lee WS, Kim MJ et al (2008) Risk factor stratification after simultaneous liver and colorectal resection for synchronous colorectal metastasis. Langenbeck’s Arch Surg 393(1):13–19
Liehr T, Manvelyan M (2009) Characterization of archived formalin-fixed/paraffin-embedded or cryofixed tissue, including nucleus extraction. In: Liehr T (ed) Fluorescence in situ hybridization (FISH)—application guide. Springer, Berlin, pp 147–156
Mollevi DG, Serrano T et al (2007) Mutations in TP53 are a prognostic factor in colorectal hepatic metastases undergoing surgical resection. Carcinogenesis 28(6):1241–1246
Munoz-Bellvis L, Fontanillo C et al (2012) Unique genetic profile of sporadic colorectal cancer liver metastasis versus primary tumors as defined by high-density single-nucleotide polymorphism arrays. Modern Pathol 25(4):590–601
Nagashima I, Takada T et al (2004) A new scoring system to classify patients with colorectal liver metastases: proposal of criteria to select candidates for hepatic resection. J Hepatobiliary Pancreat Surg 11(2):79–83
Nash GM, Gimbel M et al (2010) KRAS mutation correlates with accelerated metastatic progression in patients with colorectal liver metastases. Ann Surg Oncol 17(2):572–578
Nordlinger B, Guiguet M et al (1996) Surgical resection of colorectal carcinoma metastases to the liver. A prognostic scoring system to improve case selection, based on 1568 patients. Association Francaise de Chirurgie. Cancer 77(7):1254–1262
Pilgrim CH, Thomson BN et al (2012) The develo** clinical problem of chemotherapy-induced hepatic injury. ANZ J Surg 82(1–2):23–29
Reddy SK, Tsung A et al (2012) Does neoadjuvant chemotherapy reveal disease precluding surgical treatment of initially resectable colorectal cancer liver metastases? J Surg Oncol 105(1):55–59
Rees M, Tekkis PP et al (2008) Evaluation of long-term survival after hepatic resection for metastatic colorectal cancer: a multifactorial model of 929 patients. Ann Surg 247(1):125–135
Robinson SM, Wilson CH et al (2012) Chemotherapy-associated liver injury in patients with colorectal liver metastases: a systematic review and meta-analysis. Ann Surg Oncol 19(13):4287–4299
Settmacher U, Dittmar Y et al (2011) Predictors of long-term survival in patients with colorectal liver metastases: a single center study and review of the literature. Int J Colorectal Dis 26(8):967–981
Shimada H, Tanaka K et al (2009) Treatment for colorectal liver metastases: a review. Langenbeck’s Arch Surg 394(6):973–983
Small RM, Lubezky N et al (2009) Response to chemotherapy predicts survival following resection of hepatic colo-rectal metastases in patients treated with neoadjuvant therapy. J Surg Oncol 99(2):93–98
Tamandl D, Klinger M et al (2011) Sinusoidal obstruction syndrome impairs long-term outcome of colorectal liver metastases treated with resection after neoadjuvant chemotherapy. Ann Surg Oncol 18(2):421–430
Tanaka T, Watanabe T et al (2009) Chromosome 18q deletion as a novel molecular predictor for colorectal cancer with simultaneous hepatic metastasis. Diagn Mol Pathol 18(4):219–225
Vogelaar FJ, Mesker WE et al (2010) Clinical impact of different detection methods for disseminated tumor cells in bone marrow of patients undergoing surgical resection of colorectal liver metastases: a prospective follow-up study. BMC Cancer 10:153
Zeitoun G, Buecher B et al (2006) Retention of chromosome arm 5q in stage II colon cancers identifies 83 % of liver metastasis occurrences. Genes Chromosom Cancer 45(1):94–102
Conflict of interest
The authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Additional information
Nadine Aust and Silke Schüle share the first authorship.
Rights and permissions
About this article
Cite this article
Aust, N., Schüle, S., Altendorf-Hofmann, A.K. et al. Loss of chromosome 4 correlates with better long-term survival and lower relapse rate after R0-resection of colorectal liver metastases. J Cancer Res Clin Oncol 139, 1861–1867 (2013). https://doi.org/10.1007/s00432-013-1505-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00432-013-1505-2