Abstract
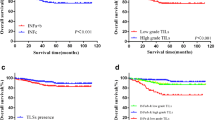
The immune microenvironment plays a pivotal role in cancer development and progression. Therefore, we studied the status of immune cells in esophageal adenocarcinoma (EAC) and adjacent Barrett’s esophagus (BE) and their association with the clinical course of patients. We included 87 patients with EAC who underwent surgical resection or endoscopic submucosal dissection. CD3, CD8, Foxp3, p53, and Ki-67 were immunolocalized in EAC and adjacent BE (N = 87) and BE without EAC (N = 13). BE adjacent to EAC exhibited higher CD3+ lamina propria lymphocyte (LPL) numbers than BE without EAC. Abundant Foxp3+ LPLs in BE were associated with dysplasia and increased Ki-67 labeling index (LI) in BE glandular cells and tended to link to aberrant p53 expression. Abundant CD8+ LPLs in adjacent BE were associated with worse prognosis of EAC patients (P = 0.019). Results of our present study firstly revealed the potential influence of the tissue immune microenvironment of BE adjacent to EAC on cancer development and eventual clinical outcome of EAC patients. T cell infiltration could play pivotal roles in facilitating the dysplasia–adenocarcinoma sequence in BE. The number of Foxp3+ T cells is increased at the early stage of carcinogenesis and could help identify patients harboring dysplastic and highly proliferating cells. CD8+ T cells could reflect unfavorable inflammatory response in adjacent tissue microenvironment and help predict worse prognosis of EAC patients.




Similar content being viewed by others
Abbreviations
- BE:
-
Barrett’s esophagus
- EAC:
-
esophageal adenocarcinoma
- EGJ:
-
esophagogastric junction
- ESD:
-
endoscopic submucosal dissection
- LPL:
-
lamina propria lymphocyte
- LSBE:
-
long-segment BE
- SSBE:
-
short-segment BE
- TIL:
-
tumor-infiltrating lymphocyte
References
(2017) Japanese classification of esophageal cancer, 11th edition: part I. Esophagus 14:1–36
Fitzgerald RC, di Pietro M, Ragunath K, Ang Y, Kang JY, Watson P, Trudgill N, Patel P, Kaye PV, Sanders S, O'Donovan M, Bird-Lieberman E, Bhandari P, Jankowski JA, Attwood S, Parsons SL, Loft D, Lagergren J, Moayyedi P, Lyratzopoulos G, de Caestecker J, British Society of Gastroenterology (2014) British Society of Gastroenterology guidelines on the diagnosis and management of Barrett’s oesophagus. Gut 63:7–42
Spechler SJ, Souza RF (2014) Barrett’s esophagus. N Engl J Med 371:836–845
Coleman HG, **e SH, Lagergren J (2018) The epidemiology of esophageal adenocarcinoma. Gastroenterology 154:390–405
Ueda Y, Osada H, Osugi H (2007) Thoracic and cardiovascular surgery in Japan during 2005. Annual report by the Japanese Association for Thoracic Surgery. Gen Thorac Cardiovasc Surg 55:377–399
Masuda M, Endo S, Natsugoe S et al (2015) Thoracic and cardiovascular surgery in Japan during. Gen Thorac Cardiovasc Surg:2018
Curtius K, Wright NA, Graham TA (2017) An evolutionary perspective on field cancerization. Nat Rev Cancer 18:19
Togashi Y, Shitara K, Nishikawa H (2019) Regulatory T cells in cancer immunosuppression - implications for anticancer therapy. Nat Rev Clin Oncol 16:356–371
Lind A, Siersema PD, Kusters JG, Konijn T, Mebius RE, Koenderman L (2018) The microenvironment in Barrett’s esophagus tissue is characterized by high FOXP3 and RALDH2 levels. Front Immunol 9:1375
Rubinkiewicz M, Migaczewski M, Hankus J et al (2016) Foxp3+ lymphocyte count in Barrett’s esophagus tissue is higher than in inflamed esophageal tissue. Folia Med Cracov 3:51–59
Waldner MJ, Neurath MF (2009) Colitis-associated cancer: the role of T cells in tumor development. Semin Immunopathol 31:249–256
Kavanagh ME, Conroy MJ, Clarke NE, Gilmartin NT, O'Sullivan KE, Feighery R, MacCarthy F, O'Toole D, Ravi N, Reynolds JV, O'Sullivan J, Lysaght J (2016) Impact of the inflammatory microenvironment on T-cell phenotype in the progression from reflux oesophagitis to Barrett oesophagus and oesophageal adenocarcinoma. Cancer Lett 370:117–124
Tantibhaedhyangkul U, Tatevian N, Gilger MA et al (2009) Increased esophageal regulatory T cells and eosinophil characteristics in children with eosinophilic esophagitis and gastroesophageal reflux disease. Ann Clin Lab Sci 39(2):99–107
Siewert JR, Stein HJ (1998) Classification of adenocarcinoma of the oesophagogastric junction. Br J Surg 85:1457–1459
Magi-Galluzzi C, Maddala T, Falzarano SM, Cherbavaz DB, Zhang N, Knezevic D, Febbo PG, Lee M, Lawrence HJ, Klein EA (2016) Gene expression in normal-appearing tissue adjacent to prostate cancers are predictive of clinical outcome: evidence for a biologically meaningful field effect. Oncotarget 7:33855–33865
Richiardi L, Fiano V, Grasso C, Zugna D, Delsedime L, Gillio-Tos A, Merletti F (2013) Methylation of APC and GSTP1 in non-neoplastic tissue adjacent to prostate tumour and mortality from prostate cancer. PLoS One 8:e68162
Moons LM, Kusters JG, Bultman E et al (2005) Barrett’s oesophagus is characterized by a predominantly humoral inflammatory response. J Pathol 207:269–276
Salgado R, Denkert C, Demaria S, Sirtaine N, Klauschen F, Pruneri G, Wienert S, van den Eynden G, Baehner FL, Penault-Llorca F, Perez EA, Thompson EA, Symmans WF, Richardson AL, Brock J, Criscitiello C, Bailey H, Ignatiadis M, Floris G, Sparano J, Kos Z, Nielsen T, Rimm DL, Allison KH, Reis-Filho JS, Loibl S, Sotiriou C, Viale G, Badve S, Adams S, Willard-Gallo K, Loi S (2015) The evaluation of tumor-infiltrating lymphocytes (TILs) in breast cancer: recommendations by an international TILs working group 2014. Ann Oncol 26:259–271
Hwang WT, Adams SF, Tahirovic E, Hagemann IS, Coukos G (2012) Prognostic significance of tumor-infiltrating T cells in ovarian cancer: a meta-analysis. Gynecol Oncol 124:192–198
Konno-Kumagai T, Fujishima F, Nakamura Y, Nakano T, Nagai T, Kamei T, Sasano H (2019) Programmed death-1 ligands and tumor infiltrating T lymphocytes in primary and lymph node metastasis of esophageal cancer patients. Dis Esophagus 32
Salama P, Phillips M, Grieu F, Morris M, Zeps N, Joseph D, Platell C, Iacopetta B (2009) Tumor-infiltrating FOXP3+ T regulatory cells show strong prognostic significance in colorectal cancer. Journal of clinical oncology : official journal of the American Society of Clinical Oncology 27:186–192
Chiba T, Ohtani H, Mizoi T, Naito Y, Sato E, Nagura H, Ohuchi A, Ohuchi K, Shiiba K, Kurokawa Y, Satomi S (2004) Intraepithelial CD8+ T-cell-count becomes a prognostic factor after a longer follow-up period in human colorectal carcinoma: possible association with suppression of micrometastasis. Br J Cancer 91:1711–1717
Frey DM, Droeser RA, Viehl CT, Zlobec I, Lugli A, Zingg U, Oertli D, Kettelhack C, Terracciano L, Tornillo L (2010) High frequency of tumor-infiltrating FOXP3(+) regulatory T cells predicts improved survival in mismatch repair-proficient colorectal cancer patients. Int J Cancer 126:2635–2643
Naito Y, Saito K, Shiiba K, Ohuchi A, Saigenji K, Nagura H, Ohtani H (1998) CD8+ T cells infiltrated within cancer cell nests as a prognostic factor in human colorectal cancer. Cancer Res 58:3491–3494
Kastelein F, Biermann K, Steyerberg EW, Verheij J, Kalisvaart M, Looijenga LHJ, Stoop HA, Walter L, Kuipers EJ, Spaander MCW, Bruno MJ, on behalf of the ProBar-study group (2013) Aberrant p53 protein expression is associated with an increased risk of neoplastic progression in patients with Barrett’s oesophagus. Gut 62:1676–1683
Kaye PV, Ilyas M, Soomro I, Haider SA, Atwal G, Menon S, Gill S, Richards C, Harrison R, West K, Ragunath K (2016) Dysplasia in Barrett’s oesophagus: p53 immunostaining is more reproducible than haematoxylin and eosin diagnosis and improves overall reliability, while grading is poorly reproducible. Histopathology 69:431–440
van Olphen S, Biermann K, Spaander MC et al (2015) SOX2 as a novel marker to predict neoplastic progression in Barrett's esophagus. Am J Gastroenterol 110:1420–1428
Sikkema M, Kerkhof M, Steyerberg EW, Kusters JG, van Strien PMH, Looman CWN, van Dekken H, Siersema PD, Kuipers EJ (2009) Aneuploidy and overexpression of Ki67 and p53 as markers for neoplastic progression in Barrett’s esophagus: a case-control study. Am J Gastroenterol 104:2673–2680
Altaf K, **ong JJ, la Iglesia D et al (2017) Meta-analysis of biomarkers predicting risk of malignant progression in Barrett's oesophagus. Br J Surg 104:493–502
Odze RD. WHO classification of tumours, 5th edition, Volume 1: Digestive System Tumours 2019:32–5
Hong MK, Laskin WB, Herman BE, Johnston MH, Vargo JJ, Steinberg SM, Allegra CJ, Johnston PG (1995) Expansion of the Ki-67 proliferative compartment correlates with degree of dysplasia in Barrett’s esophagus. Cancer 75:423–429
Nakamura T, Shima T, Saeki A et al (2007) Expression of indoleamine 2, 3-dioxygenase and the recruitment of Foxp3-expressing regulatory T cells in the development and progression of uterine cervical cancer. Cancer Sci 98:874–881
Luo Q, Zhang S, Wei H, Pang X, Zhang H (2015) Roles of Foxp3 in the occurrence and development of cervical cancer. Int J Clin Exp Pathol 8:8717–8730
Olguín JE, Medina-Andrade I, Molina E, Vázquez A, Pacheco-Fernández T, Saavedra R, Pérez-Plasencia C, Chirino YI, Vaca-Paniagua F, Arias-Romero LE, Gutierrez-Cirlos EB, León-Cabrera SA, Rodriguez-Sosa M, Terrazas LI (2018) Early and partial reduction in CD4+Foxp3+ regulatory T cells during colitis-associated colon cancer induces CD4+ and CD8+ T cell activation inhibiting tumorigenesis. J Cancer 9:239–249
Stein AV, Dislich B, Blank A, Guldener L, Kröll D, Seiler CA, Langer R (2017 Jan) High intratumoural but not peritumoural inflammatory host response is associated with better prognosis in primary resected oesophageal adenocarcinomas. Pathology 49(1):30–37
Noble F, Mellows T, McCormick Matthews LH et al (2016) Tumour infiltrating lymphocytes correlate with improved survival in patients with oesophageal adenocarcinoma. Cancer Immunol Immunother 65(6):651–662
Hynes CF, Kwon DH, Vadlamudi C, Lofthus A, Iwamoto A, Chahine JJ, Desale S, Margolis M, Kallakury BV, Watson TJ, Haddad NG, Marshall MB (2018) Programmed death ligand 1: a step toward Immunoscore for esophageal cancer. Ann Thorac Surg 106(4):1002–1007
Zingg U, Montani M, Frey DM, Dirnhofer S, Esterman AJ, Went P, Oertli D (2010) Tumour-infiltrating lymphocytes and survival in patients with adenocarcinoma of the oesophagus. Eur J Surg Oncol 36(7):670–677
Pech O, Behrens A, May A, Nachbar L, Gossner L, Rabenstein T, Manner H, Guenter E, Huijsmans J, Vieth M, Stolte M, Ell C (2008) Long-term results and risk factor analysis for recurrence after curative endoscopic therapy in 349 patients with high-grade intraepithelial neoplasia and mucosal adenocarcinoma in Barrett's oesophagus. Gut 57:1200–1206
Acknowledgments
We would like to acknowledge Ms. Yayoi Aoyama and Ms. Yasuko Furukawa for technical support.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation, data collection, and analysis were performed by Yusuke Gokon, Fumiyoshi Fujishima, Hirotaka Ishida, Taku Yamagata, Takashi Sawai, Miwa Uzuki, Hirofumi Ichikawa, Yuko Itakura, Kazutomi Takahashi, Nobuhisa Yajima, Motohisa Hagiwara, Akiko Nishida, Yohei Ozawa, Tsutomu Sakuma, Rikiya Kanba, Kazuhiro Sakamoto, Masashi Zuguchi, and Masahiro Saito. The first draft of the manuscript was written by Yusuke Gokon and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
The study protocol was approved by the ethics committee or institutional review board of each participating institution (Accession number of Tohoku University Hospital 2017–1-325). Informed consent was obtained for experimentation with human subjects.
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Gokon, Y., Fujishima, F., Taniyama, Y. et al. Immune microenvironment in Barrett’s esophagus adjacent to esophageal adenocarcinoma: possible influence of adjacent mucosa on cancer development and progression. Virchows Arch 477, 825–834 (2020). https://doi.org/10.1007/s00428-020-02854-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00428-020-02854-0