Abstract
Purpose
Adrenal venous sampling is generally considered the gold standard to identify unilateral hormone production in cases of primary hyperaldosteronism. The aim of this study is to evaluate whether the iodine-131-6-β-iodomethyl-19-norcholesterol (NP-59) test may represent an alternative in selected cases.
Methods
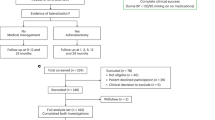
Patients submitted to laparoscopic adrenalectomy for suspected primary hyperaldosteronism (n = 27) were retrospectively reviewed. When nuclear medicine tests were preoperatively performed, their results were compared with the histopathologic findings and clinical improvement.
Results
Nuclear medicine tests were realized in 13 patients. In 11 (84.6%), a planar anterior and posterior NP-59 scintigraphy was performed and a SPECT/TC in two (15.4%). Scintigraphy indicated a preoperative lateralization in 12 out of 13 patients (92.3%). When the value of NP-59 tests was based on pathologic results, it showed a sensitivity of 90.9% and a positive predictive value of 83.3%. When the nuclear medicine test’s performance was based on postoperative blood pressure control, both sensitivity and positive predictive value were 91.6%.
Conclusions
Nuclear medicine tests represent a useful tool in the preoperative localisation of primary hyperaldosteronism with a high sensitivity and positive predictive value. In patients with contraindications to adrenal venous sampling like contrast allergies, or when it is inconclusive, scintigraphy can represent a useful and non-invasive alternative.

Similar content being viewed by others
Abbreviations
- NP-59:
-
Iodine-131-6-β-iodomethyl-19-norcholesterol
- PA:
-
Primary hyperaldosteronism
- IAH:
-
Idiopathic bilateral adrenal hyperplasia
- UAH:
-
Unilateral adrenal hyperplasia
- CT:
-
Computed tomography
- MRI:
-
Magnetic resonance imaging
- AVS:
-
Adrenal Venous Sampling
- PPV:
-
Positive predictive value
- ARR:
-
Aldosterone-to-renin ratio
- NM:
-
Nuclear medicine
- SPECT-CT:
-
Single-photon emission computed tomography
- BP:
-
Blood pressure
- TP:
-
True positive
- FN:
-
False negative
- FP:
-
False positive
- NH:
-
Nodular hyperplasia
- SUVmax :
-
Maximum standarized uptake values
References
Harvey AM (2014) Hyperaldosteronism: diagnosis, lateralization, and treatment. Surg Clin North Am 94:643–656
Mulatero P, Stowasser M, Loh KC, Fardella CE, Gordon RD, Mosso L et al (2004) Increased diagnosis of primary aldosteronism, including surgically correctable forms, in centers from five continents. J Clin Endocrinol Metab 89:1045–1050
Carey RM (2012) Primary aldosteronism. J Surg Oncol 106:575–579
Economopoulos KP, Phitayakorn R, Lubitz CC, Sadow PM, Parangi S, Stephen AE et al (2016) Should specific patient clinical characteristics discourage adrenal surgeons from performing laparoscopic transperitoneal adrenalectomy? Surgery 159:240–249
McKenzie TJ, Lillegard JB, Young WF Jr, Thompson GB (2009) Aldosteronomas—state of the art. Surg Clin North Am 89:1241–1253
Funder JW, Carey RM, Fardella C, Gomez-Sanchez CE, Mantero F, Stowasser M et al (2008) Case detection, diagnosis, and treatment of patients with primary aldosteronism: an endocrine society clinical practice guideline. J Clin Endocrinol Metab 93:3266–3281
White ML, Gauger PG, Doherty GM, Cho KJ, Thompson NW, Hammer GD et al (2008) The role of radiologic studies in the evaluation and management of primary hyperaldosteronism. Surgery 144:926–933 discussion 33
Rossi GP, Sacchetto A, Chiesura-Corona M, De Toni R, Gallina M, Feltrin GP et al (2001) Identification of the etiology of primary aldosteronism with adrenal vein sampling in patients with equivocal computed tomography and magnetic resonance findings: results in 104 consecutive cases. J Clin Endocrinol Metab 86:1083–1090
Hammarstedt L, Muth A, Wangberg B, Bjorneld L, Sigurjonsdottir HA, Gotherstrom G et al (2010) Adrenal lesion frequency: a prospective, cross-sectional CT study in a defined region, including systematic re-evaluation. Acta Radiol 51:1149–1156
Rossi GP, Auchus RJ, Brown M, Lenders JW, Naruse M, Plouin PF et al (2014) An expert consensus statement on use of adrenal vein sampling for the subty** of primary aldosteronism. Hypertension 63:151–160
Aronova A, Iii TJ, Zarnegar R (2014) Management of hypertension in primary aldosteronism. World J Cardiol 6:227–233
Abad-Cardiel M, Alvarez-Alvarez B, Luque-Fernandez L, Fernandez C, Fernandez-Cruz A, Martell-Claros N (2013) Hypertension caused by primary hyperaldosteronism: increased heart damage and cardiovascular risk. Rev Esp Cardiol (Engl Ed) 66:47–52
Sigurjonsdottir HA, Gronowitz M, Andersson O, Eggertsen R, Herlitz H, Sakinis A et al (2012) Unilateral adrenal hyperplasia is a usual cause of primary hyperaldosteronism. Results from a Swedish screening study BMC Endocr Disord 12:17
Chao CT, Wu VC, Kuo CC, Lin YH, Chang CC, Chueh SJ et al (2013) Diagnosis and management of primary aldosteronism: an updated review. Ann Med 45:375–383
Nishikawa T, Omura M, Satoh F, Shibata H, Takahashi K, Tamura N et al (2011) Guidelines for the diagnosis and treatment of primary aldosteronism—the Japan Endocrine Society 2009. Endocr J 58:711–721
Lumachi F, Marzola MC, Zucchetta P, Tregnaghi A, Cecchin D, Favia G et al (2003) Non-invasive adrenal imaging in primary aldosteronism. Sensitivity and positive predictive value of radiocholesterol scintigraphy, CT scan and MRI. Nucl Med Commun 24:683–688
Yen RF, Wu VC, Liu KL, Cheng MF, Wu YW, Chueh SC et al (2009) 131I-6beta-iodomethyl-19-norcholesterol SPECT/CT for primary aldosteronism patients with inconclusive adrenal venous sampling and CT results. J Nucl Med 50:1631–1637
Chen YC, Su YC, Wei CK, Chiu JS, Tseng CE, Chen SJ et al (2011) Diagnostic value of I-131 NP-59 SPECT/CT scintigraphy in patients with subclinical or atypical features of primary aldosteronism. J Biomed Biotechnol 2011:209787
Sarkar SD, Cohen EL, Beierwaltes WH, Ice RD, Cooper R, Gold EN (1977) A new and superior adrenal imaging agent, 131I-6beta-iodomethyl-19-nor-cholesterol (NP-59): evaluation in humans. J Clin Endocrinol Metab 45:353–362
Nocaudie-Calzada M, Huglo D, Lambert M, Ernst O, Proye C, Wemeau JL et al (1999) Efficacy of iodine-131 6beta-methyl-iodo-19-norcholesterol scintigraphy and computed tomography in patients with primary aldosteronism. Eur J Nucl Med 26:1326–1332
Kazerooni EA, Sisson JC, Shapiro B, Gross MD, Driedger A, Hurwitz GA et al (1990) Diagnostic accuracy and pitfalls of [iodine-131]6-beta-iodomethyl-19-norcholesterol (NP-59) imaging. J Nucl Med 31:526–534
Ikeda DM, Francis IR, Glazer GM, Amendola MA, Gross MD, Aisen AM (1989) The detection of adrenal tumors and hyperplasia in patients with primary aldosteronism: comparison of scintigraphy, CT, and MR imaging. AJR Am J Roentgenol 153:301–306
Gross MD, Shapiro B, Grekin RJ, Freitas JE, Glazer G, Beierwaltes WH et al (1984) Scintigraphic localization of adrenal lesions in primary aldosteronism. Am J Med 77:839–844
Chen YC, Wei CK, Chen PF, Tzeng JE, Chuang TL, Wang YF (2009) Seeking the invisible: I-131 NP-59 SPECT/CT for primary hyperaldosteronism. Kidney Int 75:663
Hennings J, Sundin A, Hagg A, Hellman P (2010) 11C-metomidate positron emission tomography after dexamethasone suppression for detection of small adrenocortical adenomas in primary aldosteronism. Langenbeck’s Arch Surg 395:963–967
Burton TJ, Mackenzie IS, Balan K, Koo B, Bird N, Soloviev DV et al (2012) Evaluation of the sensitivity and specificity of (11)C-metomidate positron emission tomography (PET)-CT for lateralizing aldosterone secretion by Conn’s adenomas. J Clin Endocrinol Metab 97:100–109
Powlson AS, Gurnell M, Brown MJ (2015) Nuclear imaging in the diagnosis of primary aldosteronism. Curr Opin Endocrinol Diabetes Obes 22:150–156
Hahner S, Kreissl MC, Fassnacht M, Haenscheid H, Bock S, Verburg FA et al (2013) Functional characterization of adrenal lesions using [123I]IMTO-SPECT/CT. J Clin Endocrinol Metab 98:1508–1518
Authors’ contributions
Study conception and design: MDM, IGS. Acquisition of data: MDM, CMC. Analysis and interpretation of data: MDM, JMdN, LDG. Drafting of manuscript: MDM, LDG, MMM. Critical revision of manuscript: IGS.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical approval
This study was merely observational and it does not contain any studies with human participants or animals performed by any of the authors.
Funding
None.
Conflict of interest
The authors declare that they have no conflict of interest.
Human and animal rights and informed consent
Informed consent was obtained from all individual participants included in the study.
Rights and permissions
About this article
Cite this article
Di Martino, M., García Sanz, I., Muñoz de Nova, J.L. et al. NP-59 test for preoperative localization of primary hyperaldosteronism. Langenbecks Arch Surg 402, 303–308 (2017). https://doi.org/10.1007/s00423-017-1561-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00423-017-1561-1