Abstract
Purpose
To evaluate the clinical outcomes of vitrectomy with induction of posterior vitreous detachment for the treatment of optic disc pit maculopathy.
Methods
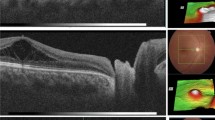
We retrospectively evaluated medical records and imaging studies of 11 consecutive patients with optic disc pit maculopathy who underwent vitrectomy at Sacco University Hospital, Milan, Italy, between October 2008 and December 2015. Induction of a posterior vitreous detachment (PVD) was the aim of our surgery. Intravitreal injection of ocriplasmin (Jetrea, Thrombogenics USA, Alcon/Novartis EU) was performed before surgery in three eyes of very young patients. Gas tamponade (sulfur hexafluoride (SF6) 20%) was used only in the first five cases. Main outcome measures were anatomic results as determined by optical coherence tomography and postoperative best-corrected visual acuity (BCVA).
Results
Before surgery, a macular detachment was present in 10 eyes and a lamellar hole of the outer retina was detected in 9 eyes. Intraoperatively, two iatrogenic paramacular holes developed in two patients during posterior hyaloid dissection. Time to PVD induction appeared to be greatly reduced in the three patients injected with ocriplasmin before surgery. Patients were followed up for a mean of 38 months (range, 18–84) after surgery. Postoperatively, one patient (9%) developed a retinal detachment that was repaired with one additional vitrectomy. Complete resolution of fluid in and under the fovea was achieved in 8 of the remaining 10 eyes (80%) without additional treatment. Reduction of the inner retinal fluid always preceded the decrease of outer retinal fluid, which in turn anticipated the absorption of macular detachment. The macular detachment resolved in a mean of 14 months after surgery. Postoperative BCVA (mean, 0.63) improved significantly compared with preoperative BCVA (mean, 0.27) (P = 0.005). Nine eyes (82%) had a postoperative BCVA of 0.5 or better.
Conclusion
Vitrectomy with induction of PVD is a safe and successful therapeutic option for the treatment of optic disc pit maculopathy. The adjunct of ocriplasmin might facilitate the induction of PVD and reduce the risk of iatrogenic retinal holes.




Similar content being viewed by others
References
Irvine AR, Crawford JB, Sullivan JH (1986) The pathogenesis of retinal detachment with morning glory disc and optic pit. Retina 6:146–150
Ohno-Matsui K, Hirakata A, Inoue M, Akiba M, Ishibashi T (2013) Evaluation of congenital optic disc pits and optic disc colobomas by swept-source optical coherence tomography. Invest Ophthalmol Vis Sci 54:7769–7778
Lincoff H, Schiff W, Krivoy D, Ritch R (1996) Optic coherence tomography of optic disk pit maculopathy. Am J Ophthalmol 122:264–266
Moon SJ, Kim JE, Spaide RF (2006) Optic pit maculopathy without inner retinal schisis cavity. Retina 26:113–116
Imamura Y, Zweifel SA, Fujiwara T et al (2010) High-resolution optical coherence tomography findings in optic pit maculopathy. Retina 30:1104–1112
Kranenburg EW (1960) Crater-like holes in the optic disc and central serous retinopathy. Arch Ophthalmol 64:912–924
Brown GC, Shields JA, Goldberg RE (1980) Congenital pits of the nerve head: II. Clinical studies in humans. Ophthalmology 87:51–65
Apple DJ, Rabb MF, Walsh PM (1982) Congenital anomalies of the optic disc. Surv Ophthalmol 27:3–41
Sobol WM, Blodi CF, Folk JC, Weingeist TA (1990) Long-term visual outcome in patients with optic nerve pit and serous retinal detachment of the macula. Ophthalmology 97:1539–1542
Theodossiadis PG, Grigoropoulos VG, Emfietzoglou J, Theodossiadis GP (2007) Vitreous findings in optic disc pit maculopathy based on optical coherence tomography. Graefes Arch Clin Exp Ophthalmol 245:1311–1318
Hirakata A, Inoue M, Hiraoka T, McCuen BW II (2012) Vitrectomy without laser treatment or gas tamponade for macular detachment associated with an optic disc pit. Ophthalmology 119:810–818
Johnson TM, Johnson MW (2004) Pathogenic implications of subretinal gas migration through pits and atypical colobomas of the optic nerve. Arch Ophthalmol 122:1793–1800
Jain N, Johnson MW (2014) Pathogenesis and treatment of maculopathy associated with cavitary optic disc anomalies. Am J Ophthalmol 158:423–435
Gass JD (1987) Stereoscopic atlas of macular diseases: diagnosis and treatment, vol II, 3rd edn. Mosby, St. Louis, pp 728–733
Cox MS, Witherspoon CD, Morris RE, Flynn HW (1988) Evolving techniques in the treatment of macular detachment caused by optic nerve pits. Ophthalmology 95:889–896
Postel EA, Pulido JS, McNamara JA, Johnson MW (1998) The etiology and treatment of macular detachment associated with optic nerve pits and related anomalies. Trans Am Ophthalmol Soc 96:73–88
Theodossiadis GP (1996) Treatment of maculopathy associated with optic disk pit by sponge explant. Am J Ophthalmol 121:630–637
Lincoff H, Yannuzzi L, Singerman L et al (1993) Improvement in visual function after displacement of the retinal elevations emanating from optic pits. Arch Ophthalmol 111:1071–1079
Lincoff H, Kreissig I (1998) Optical coherence tomography of pneumatic displacement of optic disc pit maculopathy. Br J Ophthalmol 82:367–372
Snead MP, James N, Jacobs PM (1991) Vitrectomy, argon laser, and gas tamponade for serous retinal detachment associated with an optic disc pit: a case report. Br J Ophthalmol 75:381–382
Dai S, Polkinghorne P (2003) Peeling the internal limiting membrane in serous macular detachment associated with congenital optic disc pit. Clin Exp Ophthalmol 31:272–275
Poulson AV, Snead DR, Jacobs PM et al (2004) Intraocular surgery for optic nerve disorders. Eye 18:1056–1065
Hirakata A, Okada AA, Hida T (2005) Long-term results of vitrectomy without laser treatment for macular detachment associated with an optic disc pit. Ophthalmology 112:1430–1435
Ishikawa K, Terasaki H, Mori M et al (2005) Optical coherence tomography before and after vitrectomy with internal limiting membrane removal in a child maculopathy. Jpn J Ophthalmol 49:411–413
Schaal KB, Wrede J, Dithmar S (2007) Internal drainage in optic pit maculopathy. Br J Ophthalmol 91:1093
Ghosh YK, Banerjee S, Konstantinidis A et al (2008) Surgical management of optic disc pit associated maculopathy. Eur J Ophthalmol 18:142–146
Georgalas I, Petrou P, Koutsandrea C et al (2009) Optic disc pit maculopathy treated with vitrectomy, internal limiting membrane peeling, and gas tamponade: a report of two cases. Eur J Ophthalmol 19:324–326
Theodossiadis GP, Grigoropoulos VG, Liarakos VS et al (2012) Restoration of the photoreceptor layer and improvement of visual acuity in successfully treated optic disc pit maculopathy: a long follow-up study by optical coherence tomography. Graefes Arch Clin Exp Ophthalmol 250:971–979
Shukla D, Kalliath J, Tandon M, Vijayakumar B (2012) Vitrectomy for optic disk pit with macular schisis and outer retinal dehiscence. Retina 32:1337–1342
Kiang L, Johnson M (2017) Formation of an intraretinal fluid barrier in cavitary optic disc maculopathy. Am J Ophthalmol 173:34–44
Spaide RF, Fisher Y, Ober M, Stoller G (2006) Surgical hypothesis: inner retinal fenestration as a treatment for optic disc pit maculopathy. Retina 26:89–91
Ooto S, Mittra R, Ridley M, Spaide R (2014) Vitrectomy with inner retinal fenestrations for optic disc pit maculopathy. Ophthalmology 121:1727–1733
Bottoni F, Secondi R, Giani A, Cereda M, Staurenghi G (2013) Maculopathy resolution after surgery for an optic disc pit. Ophthalmology 120:877–878 (Correspondence)
Lee JH, HL PK, Baek J, Ki Lee W (2016) Alterations of the lamina cribrosa are associated with peripapillary retinoschisis in glaucoma and pachychoroid spectrum disease. Ophthalmology 123:2066–2076
Slocumb RW, Johnson MW (2010) Premature closure of inner retinal fenestration in the treatment of optic disk pit maculopathy. Retin Cases Brief Rep 4(1):37–39
Spaide R (2008) Autofluorescence from the outer retina and subretinal space: hypothesis and review. Retina 28:5–35
Kon Y, Iida T, Maruko I, Saito M (2008) The optical coherence tomography-ophthalmoscope for examination of central serous chorioretinopathy with precipitates. Retina 28:864–869
Secondi R, Kong J, Blonska A, Staurenghi G, Sparrow JR (2012) Fundus autofluorescence findings in a mouse model of retinal detachment. Invest Ophthalmol Vis Sci 53:5190–5197
Funding
This research received no specific grant from any funding agency in the public, commercial or not-for-profit sectors.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All authors declare that they have no competing interests.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. For this type of study, formal consent is not required.
Rights and permissions
About this article
Cite this article
Bottoni, F., Cereda, M., Secondi, R. et al. Vitrectomy for optic disc pit maculopathy: a long-term follow-up study. Graefes Arch Clin Exp Ophthalmol 256, 675–682 (2018). https://doi.org/10.1007/s00417-018-3925-9
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00417-018-3925-9