Abstract
Objective
This study aims to observe the mechanical weak point and histological features of tendon–bone interface after anterior cruciate ligament reconstructive surgery and to explore the tendon–bone healing effects of the platelet-rich gel (PRG) + deproteinized bone (DPB) compound.
Methods
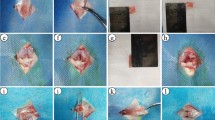
A total of 48 New Zealand white rabbits were randomly divided into normal group, model (without embedding), experimental (embedded with the PRG + DPB compound), and control (embedded with DPB) groups. The rabbits were executed at 2, 4, 8, and 12 weeks after the operation. Then, micro-computed tomography scan and uniaxial tensile test were conducted. The fractured specimens were subjected to histological observation.
Results
At 4, 8, and 12 weeks after the operation, the bone density of the tendon–bone bound section of the experimental group was higher than that of the other groups (P < 0.05). At 4 and 8 weeks, the maximum tensile load of the experimental group was obviously higher than that of the control and model groups (P < 0.05). Histological observation indicated that the tendon–bone interface in the experimental group had more cartilage and bone tissue growing toward the internal tendon, but the fracture layer mainly occurred in the non-ankylosed part.
Conclusion
The mechanical weak point of the early tendon–bone interface was in the immature fibrous tissue. The PRG + DPB compound can effectively trigger tendon–bone healing by promoting the maturation and ossification of the tendon–bone tissue. This compound improved the tensile strength of the healing interface and reduced bone tunnel enlargement.






Similar content being viewed by others
References
Park MJ, Lee MC, Seong SC (2001) A comparative study of the healing of tendon autograft and tendon–bone autograft using patellar tendon in rabbits. Int Orthop 25:35–39
Weiler A, Hoffmann RF, Bail HJ, Rehm O, Südkamp NP (2002) Tendon healing in a bone tunnel. Part II: histologic analysis after biodegradable interference fit fixation in a model of anterior cruciate ligament reconstruction in sheep. Arthroscopy 18:124–135
Murray MM, Spindler KP, Abreu E et al (2007) Collagen-platelet rich plasma hydrogel enhances primary repair of the porcine anterior cruciate ligament. J Orthop Res 25:81–91
Anderson K, Seneviratne AM, Izawa K, Atkinson BL, Potter HG, Rodeo SA (2001) Augmentation of tendon healing in an intraarticular bone tunnel with use of a bone growth factor. Am J Sports Med 29:689–698
Ozkan K, Eralp L, Kocaoglu M et al (2007) The effect of transforming growth factor β1 (TGF-β1) on the regenerate bone in distraction osteogenesis. Grow Fact 25:101–107
Anitua E, Andia I, Ardanza B, Nurden P, Nurden AT (2004) Autologous platelets as a source of proteins for healing and tissue regeneration. Thromb Haemost 91:4–15
Everts PA, Knape JT, Weibrich G et al (2006) Platelet-rich plasma and platelet gel: a review. J Ext Corpor Technol 38:174–187
Camargo PM, Lekovic V, Weinlaender M, Vasilic N, Madzarevic M, Kenney EB (2002) Platelet-rich plasma and bovine porous bone mineral combined with guided tissue regeneration in the treatment of intrabony defects in humans. J Periodon Res 37:300–306
Thorwarth M, Wehrhan F, Schultze-Mosgau S, Wiltfang J, Schlegel KA (2006) PRP modulates expression of bone matrix proteins in vivo without long-term effects on bone formation. Bone 38:30–40
Rodriguez A, Anastassov GE, Lee H, Buchbinder D, Wettan H (2003) Maxillary sinus augmentation with deproteinated bovine bone and platelet rich plasma with simultaneous insertion of endosseous implants. J Oral Maxillofac Surg 61:157–163
Hutmacher DW (2000) Scaffolds in tissue engineering bone and cartilage. Biomaterials 21:2529–2543
Landesberg R, Roy M, Glickman RS (2000) Quantification of growth factor levels using a simplified method of platelet-rich plasma gel preparation. J Oral Maxillofac Surg 58:297–301
Zhao Y, Zhai W (2010) Histological observation of tendon–bone healing after anterior cruciate ligament reconstruction by platelet-rich plasma combined with deproteinized bone of calf. Zhongguo **u Fu Chong Jian Wai Ke Za Zhi 24:1323–1329
Martinek V, Latterman C, Usas A et al (2002) Enhancement of tendon–bone integration of anterior cruciate ligament grafts with bone morphogenetic protein-2 gene transfer: a histological and biomechanical study. J B Jt Surg Am 84-A:1123–1131
Tomita F, Yasuda K, Mikami S, Sakai T, Yamazaki S, Tohyama H (2001) Comparisons of intraosseous graft healing between the doubled flexor tendon graft and the bone-patellar tendon–bone graft in anterior cruciate ligament reconstruction. Arthroscopy 17:461–476
Anitua E, Sanchez M, Nurden AT et al (2007) Reciprocal actions of platelet-secreted TGF-β1 on the production of VEGF and HGF by human tendon cells. Plast Reconstr Surg 119:950–959
Ma CB, Kawamura S, Deng XH et al (2007) Bone morphogenetic proteins-signaling plays a role in tendon-to-bone healing: a study of rhBMP-2 and noggin. Am J Spor Med 35:597–604
Bosch G, van Schie HT, de Groot MW et al (2010) Effects of platelet-rich plasma on the quality of repair of mechanically induced core lesions in equine superficial digital flexor tendons: a placebo-controlled experimental study. J Orthop Res 28:211–217
Yamakado K, Kitaoka K, Yamada H, Hashiba K, Nakamura R, Tomita K (2002) The influence of mechanical stress on graft healing in a bone tunnel. Arthroscopy 18:82–90
Berg EE, Pollard ME, Kang Q (2001) Interarticular bone tunnel healing. Arthroscopy 17:189–195
Acknowledgments
We extremely appreciate the patient guidance and substantial support in the material preparation in the aspect of mechanics, microanatomy and imaging, respectively, from teacher Weidong Zhao in biomechanical experiment of Nan**g Medical University, teacher Yihe Guo in pathology department of the 175th Military Hospital of PLA, teacher Lin Ouyang in Southeast Imaging Center of Southeast Hospital Affiliated to **amen University. Thanks for the hard work of all the workers in Animal Experiment Center of Southeast Hospital Affiliated to **amen University.
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Zhai, W., Lv, C., Zheng, Y. et al. Weak link of tendon–bone healing and a control experiment to promote healing. Arch Orthop Trauma Surg 133, 1533–1541 (2013). https://doi.org/10.1007/s00402-013-1802-x
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00402-013-1802-x