Abstract
Purpose
Evaluation of orbital proptosis and sutural synostosis pattern along the coronal ring in craniofaciosynostosis patients with or without fibroblastic growth factor receptor 2 (FGFR2) mutation.
Methods
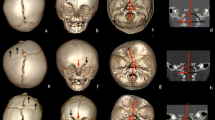
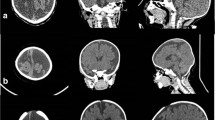
High-resolution computer tomography was used to assess, in children with or without FGFR2 mutation, the early synostotic involvement of the “major” and “minor” sutures/synchondroses of the coronal arch along with the following orbital parameters: interorbital angle, bone orbital cavity volume, globe volume, ventral globe volume, ventral globe index.
Results
Infants with FGFR2 mutation showed an increased number of closed minor sutures/synchondroses along the posterior coronal branch while both groups showed a comparable synostotic involvement of the minor sutures of the anterior coronal branch. FGFR2 infants with posterior coronal branch synostotic involvement showed a higher degree of proptosis due to both reduced bony cavity volume and increased globe volume (p<0.05).
Conclusions
Our data show that FGFR2 mutation together with posterior coronal branch synostotic involvement has a synergic effect in causing a more severe degree of orbital proptosis.




Similar content being viewed by others
References
Forte AJ, Steinbacher DM, Persing JA, Brooks ED, Andrew TW, Alonso N (2015) Orbital dysmorphology in untreated children with Crouzon and Apert syndromes. Plast Reconstr Surg 136:1054–1062. https://doi.org/10.1097/PRS.0000000000001693
Carr M, Posnick JC, Pron G, Armstrong D (1992) Cranio-orbito-zygomatic measurements from standard CT scans in unoperated Crouzon and Apert infants: comparison with normal controls. Cleft Palate Craniofac J 29:129–136. https://doi.org/10.1597/1545-1569_1992_029_0129_cozmfs_2.3.co_2
Batut C, Joly A, Travers N, Guichard B, Paré A, Laure B (2019) Surgical treatment of orbital hypertelorism: historical evolution and development prospects. J Craniomaxillofac Surg 47:1712–1719. https://doi.org/10.1016/j.jcms.2019.07.002
Oreroglu AR, Silav G, Ozkaya O, Orman C, Akan M (2013) Concurrent repair of orbital shallowness with craniosynostosis surgery: two late cases of simultaneous orbital decompression. Turk Neurosurg 23:395–400. https://doi.org/10.5137/1019-5149.JTN.5444-11.2
Newman SA (1991) Ophthalmic features of craniosynostosis. Neurosurg Clin N Am 2:587–610
Azoury SC, Reddy S, Shukla V, Deng CX (2017) Fibroblast growth factor receptor 2 (FGFR2) mutation related syndromic craniosynostosis. Int J Biol Sci 13:1479–1488. https://doi.org/10.7150/ijbs.22373
Festa F, Pagnoni M, Valerio R, Rodolfino D, Saccucci M, d’Attilio M, Caputi S, Iannetti G (2012) Orbital volume and surface after Le Fort III advancement in syndromic craniosynostosis. J Craniofac Surg 23:789–792. https://doi.org/10.1097/SCS.0b013e31824dbeec
Imai K, Fujimoto T, Takahashi M, Maruyama Y, Yamaguchi K (2013) Preoperative and postoperative orbital volume in patients with Crouzon and Apert syndrome. J Craniofac Surg 24:191–194. https://doi.org/10.1097/SCS.0b013e3182668581
Cohen MM (1993) Sutural biology and the correlates of craniosynostosis. Am J Med Genet 47:581–616. https://doi.org/10.1002/ajmg.1320470507
Cruz AA, Garcia DM, Akaishi PM et al (2015) Globe protrusion and interorbital divergence in syndromic faciocraniosynostoses. J Craniofac Surg 26:1163–1164. https://doi.org/10.1097/SCS.0000000000001553
Calandrelli R, D’Apolito G, Gaudino S, Sciandra MC, Caldarelli M, Colosimo C (2014) Identification of skull base sutures and craniofacial anomalies in children with craniosynostosis: utility of multidetector CT. Radiol Med 119:694–704. https://doi.org/10.1007/s11547-014-0387-y
Ganesh A, Edmond J, Forbes B, Katowitz WR, Nischal KK, Miller M, Levin AV (2019) An update of ophthalmic management in craniosynostosis. J AAPOS 23:66–76. https://doi.org/10.1016/j.jaapos.2018.10.016
Runyan CM, Xu W, Alperovich M et al (2017) Minor suture fusion in syndromic craniosynostosis. Plast Reconstr Surg 140:434e–445e. https://doi.org/10.1097/PRS.0000000000003586
Bentley RP, Sgouros S, Natarajan K, Dover MS, Hockley AD (2002) Changes in orbital volume during childhood in cases of craniosynostosis. J Neurosurg 96:747–754. https://doi.org/10.3171/jns.2002.96.4.0747
Bentley RP, Sgouros S, Natarajan K, Dover MS, Hockley AD (2002) Normal changes in orbital volume during childhood. J Neurosurg 96:742–746. https://doi.org/10.3171/jns.2002.96.4.0742
Calandrelli R, D’Apolito G, Gaudino S, Stefanetti M, Massimi L, di Rocco C, Colosimo C (2014) Radiological assessment of skull base changes in children with syndromic craniosynostosis: role of “minor” sutures. Neuroradiology 56:865–875. https://doi.org/10.1007/s00234-014-1392-5
Hill CA, Vaddi S, Moffitt A, Kane AA, Marsh JL, Panchal J, Richtsmeier JT, Aldridge K (2011) Intracranial volume and whole brain volume in infants with unicoronal craniosynostosis. Cleft Palate Craniofac J 48:394–398. https://doi.org/10.1597/10-051
Lo LJ, Marsh JL, Kane AA, Vannier MW (1996) Orbital dysmorphology in unilateral coronal synostosis. Cleft Palate Craniofac J 33:190–197. https://doi.org/10.1597/1545-1569_1996_033_0190_odiucs_2.3.co_2
Khonsari RH, Way B, Nysjo J et al (2016) Fronto-facial advancement and bipartition in Crouzon-Pfeiffer and Apert syndromes: impact of fronto-facial surgery upon orbital and airway parameters in FGFR2 syndromes. J Craniomaxillofac Surg 44:1567–1575. https://doi.org/10.1016/j.jcms.2016.08.015
Cruz AA, Akaishi PM, Arnaud E et al (2007) Exorbitism correction of faciocraniosynostoses by monobloc frontofacial advancement with distraction osteogenesis. J Craniofac Surg 18:355–360. https://doi.org/10.1097/scs.0b013e3180333b3c
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethics approval
We declare that all procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. For this type of study, formal consent is not required.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Conflict of interest
Rosalinda Calandrelli declares that she has no conflict of interest.
Fabio Pilato declares that he has no conflict of interest.
Antonio Marrazzo declares that he has no conflict of interest.
Luca Massimi declares that he has no conflict of interest.
Marco Panfili declares that he has no conflict of interest.
Cesare Colosimo declares that he is scientific consultant for Bracco Diagnostics Inc. and Bayer HealthCare.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Calandrelli, R., Pilato, F., Marrazzo, A. et al. Computer tomography–based quantitative analysis of the orbital proptosis severity in infants with syndromic craniosynostosis: case-control study. Childs Nerv Syst 37, 1659–1668 (2021). https://doi.org/10.1007/s00381-021-05062-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00381-021-05062-6