Abstract
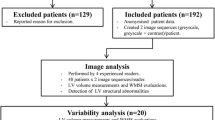
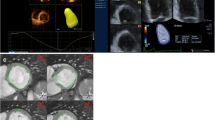
We retrospectively assessed the rest-phase images of 300 contrast stress- echocardiograms, during which very-low mechanical index (VLMI) imaging with ultrasound enhancing agents (UEAs) was routinely acquired in addition to greyscale echocardiography; intra- and inter-reader variability for left ventricle (LV) volumes and ejection fraction (LVEF) at rest was established in the overall cohort and normal values were calculated in the subset of subjects with no cardiac risk factors or cardiac disease and a normal stress-echocardiogram. Current recommendations for chamber quantification using echocardiography advise the use of UEAs in case of insufficient quality of endocardial visualization, but normal values for LV volumes and LVEF using UEAs have never been published using currently recommended VLMI method. Single-centre retrospective study, enrolling subjects referred to contrast stress- echocardiography for suspect coronary artery disease, including the acquisition of both standard 2D greyscale and bolus UEAs with VLMI, regardless of the image quality. This enables offline measurement of the LV volumes and LVEF for both greyscale and UEAs–VLMI images at rest in all subjects. Images were allocated to 3 readers in random order. Normal range for LV volumes and LVEF was also derived in a subset of apparently healthy subjects. In the 298 exams finally assessed, measurement variability among the three readers was lower with UEAs-VLMI, in particular for end-systolic volumes (intra-class correlation coefficient for concordance improved from 0.855 to 0.916, for LVEF from 0.68 to 0.783, p < 0.01), intra- observer variability reduced (Lin’s correlation coefficient for LVEF from 0.747 to 0.857, p < 0.01). Normal mean indexed LV end-diastolic volume with UEAs-VLMI, compared to greyscale imaging, was + 14 ml/m2, while LVEF was + 5 to + 6% points. This is the largest study specifically addressing UEAs–VLMI imaging and comparing data with standard greyscale imaging; it demonstrates a reduction in measurement variability of LV volumes and LVEF. Normal reference values for VLMI ultrasound are reported for the first time in comparison with greyscale values.







Similar content being viewed by others
Abbreviations
- LV:
-
Left ventricle
- UEAs:
-
Ultrasound enhancing agents
- LVEF:
-
Left ventricle ejection fraction
- VLMI:
-
Very low mechanical-index contrast-echocardiography
- EACVI:
-
European Association of Cardiovascular Imaging
- ASE:
-
American Society of Echocardiography
- EDV:
-
End-diastolic volume
- ESV:
-
End-systolic volume
- GLS:
-
Global longitudinal strain
- SD:
-
Standard deviation
- BSA:
-
Body surface index
- EDVi:
-
EDV indexed to BSA
- ESVi:
-
ESV indexed to BSA
- EDVc:
-
Contrast EDV
- EDVci:
-
Contrast EDV indexed to BSA
- ESVci:
-
Contrast ESV indexed to BSA
References
Lang RM, Badano LP, Mor-Avi V, Afilalo J, Armstrong A, Ernande L, Flachskampf FA, Foster E, Goldstein SA, Kuznetsova T, Lancellotti P, Muraru D, Picard MH, Rietzschel ER, Rudski L, Spencer KT, Tsang W, Voigt JU (2015) Recommendations for cardiac chamber quantification by echocardiography in adults: an update from the American Society of Echocardiography and the European Association of Cardiovascular Imaging. Eur Heart J Cardiovasc Imaging 16(3):233–270
Porter TR, Mulvagh SL, Abdelmoneim SS, Becher H, Belcik JT, Bierig M, Choy J, Gaibazzi N, Gillam LD, Janardhanan R, Kutty S, Leong-Poi H, Lindner JR, Main ML, Mathias W Jr, Park MM, Senior R, Villanueva F (2018) Clinical applications of ultrasonic enhancing agents in echocardiography: 2018 American Society of Echocardiography Guidelines Update. J Am Soc Echocardiogr 31(3):241–274
Senior R, Becher H, Monaghan M, Agati L, Zamorano J, Vanoverschelde JL, Nihoyannopoulos P, Edvardsen T, Lancellotti P; EACVI Scientific Documents Committee for 2014–16 and 2016–18; EACVI Scientific Documents Committee for 2014–16 and 2016–18 (2017) Clinical practice of contrast echocardiography: recommendation by the European Association of Cardiovascular Imaging (EACVI). Eur Heart J Cardiovasc Imaging 18(11):1205–1205af.
Hoffmann R, Barletta G, von Bardeleben S, Vanoverschelde JL, Kasprzak J, Greis C, Becher H (2014) Analysis of left ventricular volumes and function: a multicenter comparison of cineventriculography, cardiac magnetic resonance imaging, unenhanced and contrast enhanced 2D and 3D echocardiography. J Am Soc Echocardiogr 27(3):292–301
Hoffmann R, von Bardeleben S, ten Cate R, Borges AC, Kasprzak J, Firschke C, Lafitte S, Al-Saadi N, Kuntz-Hehner S, Engelhardt M, Becher H, Vanoverschelde JL (2005) Assessment of systolic left ventricular function: a multi-centre comparison of cineventriculography, cardiac magnetic resonance imaging, unenhanced and contrast- enhanced echocardiography. Eur Heart J 26(6):607–616
Hoffmann R, von Bardeleben S, Kasprzak JD, Borges AC, ten Cate F, Firschke C, Lafitte S, Al-Saadi N, Kuntz-Hehner S, Horstick G, Greis C, Engelhardt M, Vanoverschelde JL, Becher H (2006) Analysis of regional left ventricular function by cineventriculography, cardiac magnetic resonance imaging, and unenhanced and contrast-enhanced echocardiography: a multicenter comparison of methods. J Am Coll Cardiol 47(1):121–128
Jenkins C, Moir S, Chan J, Rakhit D, Haluska B, Marwick TH (2009) Left ventricular volume measurement with echocardiography: a comparison of left ventricular opacification, three- dimensional echocardiography, or both with magnetic resonance imaging. Eur Heart J 30(1):98–106
Larsson MK, Da Silva C, Gunyeli E, Ilami AA, Szummer K, Winter R, Bjällmark A (2016) The potential clinical value of contrast-enhanced echocardiography beyond current recommendations. Cardiovasc Ultrasound 14:2
Thavendiranathan P, Grant AD, Negishi T, Plana JC, Puporvic ZB, Marwick TM (2013) Reproducibility of echocardiographic techniques for the sequential assessment of left ventricular ejection fraction and volumes: application to patients undergoing cancer chemotherapy. J Am Colloid Cardiol 61(1):77–84
Ünlü S, Mirea O, Duchenne J, Pagourelias ED, Bézy S, Thomas JD, Badano LP, Voigt JU (2018) Comparison of feasibility, accuracy, and reproducibility of layer-specific global longitudinal strain measurements among five different vendors: a report from the EACVI-ASE Strain Standardization Task Force. J Am Soc Echocardiogr 31(3):374–380
Malm S, Frigstad S, Sagberg E, Larsson H, Skjaerpe T (2004) Accurate and reproducible measurement of left ventricular volume and ejection fraction by contrast echocardiography: a comparison with magnetic resonance imaging. J Am Coll Cardiol 44(5):1030–1035
Reilly JP, Tunick PA, Timmermans RJ, Stein B, Rosenzweig BP, Kronzon I (2000) Contrast echocardiography clarifies uninterpretable wall motion in intensive care unit patients. J Am Coll Cardiol 35(2):485–490
Kurt M, Shaikh KA, Peterson L, Kurrelmeyer KM, Shah G, Nagueh SF, Fromm R, Quinones MA, Zoghbi WA (2009) Impact of contrast echocardiography on evaluation of ventricular function and clinical management in a large prospective cohort. J Am Coll Cardiol 53(9):802–810
Mistry N, Halvorsen S, Hoffmann P, Müller C, Bøhmer E, Kjeldsen SE, Bjørnerheim R (2010) Assessment of left ventricular function with magnetic resonance imaging vs. echocardiography, contrast echocardiography, and single-photon emission computed tomography in patients with recent ST-elevation myocardial infarction. Eur J Echocardiogr 11(9):793–800
Lim TK, Burden L, Janardhanan R, ** C, Moon J, Pennell D, Senior R (2005) Improved accuracy of low-power contrast echocardiography for the assessment of left ventricular remodelling compared with unenhanced harmonic echocardiography after acute myocardial infarction: comparison with cardiovascular magnetic resonance imaging. J Am Soc Echocardiogr 18(11):1203–1207
Suwatanaviroj T, He W, Pituskin E, Paterson I, Choy J, Becher H (2018) What is the minimum change in left ventricular ejection fraction, which can be measured with contrast echocardiography? Echo Res Pract 5(2):71–77
Kawel-Boehm N, Maceira A, Valsangiacomo-Buechel ER, Vogel-Claussen J, Turkbey EB, Williams R, Plein S, Tee M, Eng J, Bluemke DA (2015) Normal values for cardiovascular magnetic resonance in adults and children. J Cardiovasc Magn Reson 17:29
Porter TR, **e F, Silver M, Kricsfeld D, Oleary E (2001) Real-time perfusion imaging with low mechanical index pulse inversion Doppler imaging. J Am Coll Cardiol 37(3):748–753
Senior R, Moreo A, Gaibazzi N, Agati L, Tiemann K, Shivalkar B, von Bardeleben S, Galiuto L, Lardoux H, Trocino G, Carrió I, Le Guludec D, Sambuceti G, Becher H, Colonna P, Ten Cate F, Bramucci E, Cohen A, Bezante G, Aggeli C, Kasprzak JD (2013) Comparison of sulfur hexafluoride microbubble (SonoVue)-enhanced myocardial echocardiography to gated single photon emission computerized tomography for the detection of significant coronary artery disease: a large European Multicenter Study. J Am Coll Cardiol 62(15):1353–1361
Gaibazzi N, Reverberi C, Lorenzoni V, Molinaro S, Porter TR (2012) Prognostic value of high-dose dipyridamole stress myocardial contrast perfusion echocardiography. Circulation 126(10):1217–1224
Acknowledgements
Not applicable.
Funding
No external funding declared.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All authors declare that they have no conflict of interests.
Ethics approval and consent to participate
The study has been approved by the appropriate ethics committees and have therefore been performed in accordance with the ethical standards laid down in the 1964 Declaration of Helsinki and its later amendments. All persons gave their informed consent prior to their inclusion in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Gaibazzi, N., Tuttolomondo, D., Rabia, G. et al. Standard echocardiography versus very-low mechanical index contrast-imaging: left ventricle volumes and ejection fraction multi-reader variability and reference values in a subgroup with no risk factors or cardiac disease. Heart Vessels 35, 544–554 (2020). https://doi.org/10.1007/s00380-019-01506-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00380-019-01506-x