Abstract
Objectives
Previous analyses of the impact of median lobe presence on Greenlight photoselective vaporization of the prostate (PVP) outcomes were limited by their small sample size and the ability to adjust for important confounders. As such, we sought to investigate the impact of prostate median lobe presence on the operative outcomes of 180 W XPS GreenLight PVP using a large international database.
Methods
Data were obtained from the Global GreenLight Group (GGG) database which pools data of eight high-volume, experienced surgeons, from a total of seven international centers. All men with established benign prostatic hyperplasia who underwent GreenLight PVP using the XPS-180 W system between 2011 and 2019 were eligible for the study. Patients were assigned to two groups based on presence or absence of median lobes. Analyses were adjusted for patient age, prostate volume, body mass index, and American Society of Anesthesia (ASA) score.
Results
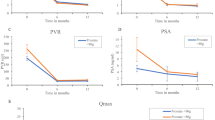
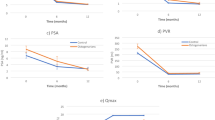
A total of 1650 men met the inclusion criteria. A median lobe was identified in 621 (37.6%) patients. Baseline prostate volume, patient age, and ASA score varied considerably between the two groups. In adjusted analyses, the operative and lasing time of patients with median lobes was 6.72 (95% CI 3.22–10.23; p < 0.01) minutes and 2.90 (95% CI 1.02–4.78; p < 0.01) minutes longer than the control group. Men with median lobes had similar postoperative functional outcomes to those without a median lobe except for a 1.59-point greater drop in the 12-month IPSS score compared to baseline (95% CI 0.11–3.08; p = 0.04) in the median lobe group, and a decrease in PVR after 6 months which was 46.51 ml (95% CI 4.65–88.36; p = 0.03) greater in patients with median lobes compared to men without median lobes.
Conclusions
Our findings suggest that the presence of a median lobe has no clinically significant impact on procedural or postoperative outcomes for patients undergoing Greenlight PVP using the XPS-180 W system.


Similar content being viewed by others
References
Bachmann A, Tubaro A, Barber N et al (2014) 180-W XPSgreenlight laser vaporisation versus transurethral resection of the prostate for the treatment of benign prostatic obstruction: 6-month safety and efficacy results of a European multicentre randomised trial—The GOLIATH study. EurUrol 65:931–942. https://doi.org/10.1016/j.eururo.2013.10.040
Foster HE, Barry MJ, Dahm P et al (2019) Re: Surgical management of lower urinary tract symptoms attributed to benign prostatic hyperplasia: AUA Guideline. J Urol 203:1219. https://doi.org/10.1016/j.juro.2018.09.058
Brunken C, Seitz C, Woo HH (2015) A systematic review of experience of 180-W XPSGreenLight laser vaporisation of the prostate in 1640 men. BJU Int 116:531–537. https://doi.org/10.1111/bju.12955
Ghobrial FK, Shoma A, Elshal AM et al (2020) A randomized trial comparing bipolar transurethral vaporization of the prostate with GreenLight laser (xps-180watt) photoselective vaporization of the prostate for treatment of small to moderate benign prostatic obstruction: outcomes after 2 years. BJU Int 125:144–152. https://doi.org/10.1111/bju.14926
Hueber PA, Bienz MN, Valdivieso R et al (2015) Photoselective vaporization of the prostate for benign prostatic hyperplasia using the 180 watt system: multicenter study of the impact of prostate size on safety and outcomes. J Urol 194:462–469. https://doi.org/10.1016/j.juro.2015.03.113
Valdivieso R, Hueber PA, Meskawi M et al (2018) Multicentre international experience of 532-nm laser photoselective vaporization with GreenLightXPS in men with very large prostates. BJU Int 122:873–878. https://doi.org/10.1111/bju.14208
Stone BV, Chughtai B, Kaplan SA et al (2015) GreenLight laser for prostates over 100 ml: what is the evidence? CurrOpinUrol 26:28–34. https://doi.org/10.1097/MOU.0000000000000237
Meskawi M, Hueber PA, Valdivieso R et al (2019) Complications and functional outcomes of high-risk patient with cardiovascular disease on antithrombotic medication treated with the 532-nm-laser photo-vaporization GreenlightXPS-180 W for benign prostate hyperplasia. World J Urol 37:1671–1678. https://doi.org/10.1007/s00345-018-2560-8
Nguyen DD, Misraï V, Bach T et al (2020) Operative time comparison of aquablation, greenlightPVP, ThuLEP, GreenLEP, and HoLEP. World J Urol. https://doi.org/10.1007/s00345-020-03137-8
Audouin M, Girshovich A, Cussenot O, Renard-Penna R (2018) Typology of intravesical prostatic protrusions, or so-called median lobes, in middle-aged and older men. SurgRadiolAnat 40:389–393. https://doi.org/10.1007/s00276-018-1999-z
Lieber MM, Jacobson DJ, McGree ME et al (2009) Intravesical prostatic protrusion in men in Olmsted County, Minnesota. J Urol 182:2819–2824. https://doi.org/10.1016/j.juro.2009.08.086
Bodokh Y, Treacy PJ, Imbert de la Phalecque L, Durand M (2018) Does prostate median lobe really matter for GreenLightHPS laser photovaporization of the prostate. J Endourol Case Rep 4:169–172. https://doi.org/10.1089/cren.2018.0053
Zorn KC, Liberman D (2011) GreenLight180WXPSphotovaporization of the prostate: how I do it. Can J Urol 18:5918–5926
Law KW, Elterman DS, Cash H et al (2019) Anatomic GreenLight laser vaporization-incision technique for benign prostatic hyperplasia using the XPSLBO-180W system: how I do it. Can J Urol 26:9963–9972
Wee JH, Choi YS, Bae WJ et al (2012) Influence of intravesical prostatic protrusion on preoperative lower urinary tract symptoms and outcomes after 120 W high performance system laser treatment in men with benign prostatic hyperplasia. Korean J Urol 53:472–477. https://doi.org/10.4111/kju.2012.53.7.472
Kim KS, Choi SW, Bae WJ et al (2015) Efficacy of a vaporization–resection of the prostate median lobe enlargement and vaporization of the prostate lateral lobe for benign prostatic hyperplasia using a 120-W GreenLight high-performance system laser: the effect on storage symptoms. Lasers Med Sci 30:1387–1393. https://doi.org/10.1007/s10103-015-1740-7
Hojgaard M, Mikines KJ (2010) Ureteral injuries during photoselective vaporization of the prostate. Scand J UrolNephrol 44:265–268. https://doi.org/10.3109/00365591003645712
Gu X, Strom K, Spaliviero M, Wong C (2013) Does prostate configuration affect the efficacy and safety of GreenLightHPSTM laser photoselective vaporization prostatectomy (PVP)? Lasers Med Sci 28:473–478. https://doi.org/10.1007/s10103-012-1085-4
Kim MS, Park KK, Chung BH, Lee SH (2013) Effect of photoselective vaporization prostatectomy on lower urinary tract symptoms in benign prostatic hyperplasia with or without intravesical prostatic protrusion. Korean J Urol 54:36–41. https://doi.org/10.4111/kju.2013.54.1.36
Law K, Tholomier C, Couture F et al (2020) PD61-07 Global Greenlight Group. J Urol. https://doi.org/10.1097/ju.0000000000000978.07
Gratzke C, Bachmann A, Descazeaud A et al (2015) EAU guidelines on the assessment of non-neurogenic male lower urinary tract symptoms including benign prostatic obstruction. EurUrol 67:1099–1109. https://doi.org/10.1016/j.eururo.2014.12.038
Nickel JC, Aaron L, Barkin J et al (2018) Canadian Urological Association guideline on male lower urinary tract symptoms/benign prostatic hyperplasia (MLUTS/BPH): 2018 update. Can UrolAssoc J 12:303–312. https://doi.org/10.5489/cuaj.5616
Eri LM, Thomassen H, Brennhovd B, Håheim LL (2002) Accuracy and repeatability of prostate volume measurements by transrectal ultrasound. Prostate Cancer Prostatic Dis 5:273–278. https://doi.org/10.1038/sj.pcan.4500568
Wang X (2014) Firth logistic regression for rare variant association tests. Front Genet 5:187. https://doi.org/10.3389/fgene.2014.00187
Doo CK, Uh HS (2009) Anatomic configuration of prostate obtained by noninvasive ultrasonography can predict clinical voiding parameters for determining BOO in men with LUTS. Urology 73:232–236. https://doi.org/10.1016/j.urology.2008.09.055
Zheng J, Pan J, Qin Y et al (2015) Role for intravesical prostatic protrusion in lower urinary tract symptom: a fluid structural interaction analysis study. BMC Urol 15:1–9. https://doi.org/10.1186/s12894-015-0081-y
Mariappan P, Brown DJG, McNeill AS (2007) Intravesical prostatic protrusion is better than prostate volume in predicting the outcome of trial without catheter in white men presenting with acute urinary retention: a prospective clinical study. J Urol 178:573–577. https://doi.org/10.1016/j.juro.2007.03.116
Park HY, Lee JY, Park SY et al (2012) Efficacy of alpha blocker treatment according to the degree of intravesical prostatic protrusion detected by transrectal ultrasonography in patients with benign prostatic hyperplasia. Korean J Urol 53:92–97. https://doi.org/10.4111/kju.2012.53.2.92
Yoshida T, Kinoshita H, Yoshida K et al (2016) Intravesical prostatic protrusion as a predicting factor for the adverse clinical outcome in patients with symptomatic benign prostatic enlargement treated with dutasteride. Urology 91:154–157. https://doi.org/10.1016/j.urology.2016.01.009
Funding
None.
Author information
Authors and Affiliations
Contributions
DDN protocol/project development, data collection or management, data analysis, manuscript writing/editing. IS protocol/project development, data collection or management, data analysis, manuscript writing/editing. KL protocol/project development, data collection or management, manuscript writing/editing. NB protocol/project development, manuscript writing/editing. DSE: Protocol/project development, manuscript writing/editing. ASZ protocol/project development, manuscript writing/editing. AA protocol/project development, manuscript writing/editing. FB Protocol/project development, manuscript writing/editing. LC protocol/project development, manuscript writing/editing. GF protocol/project development, manuscript writing/editing. CVL protocol/project development, manuscript writing/editing. TBB protocol/project development, manuscript writing/editing. EFB protocol/project development, manuscript writing/editing. HC protocol/project development, manuscript writing/editing. MR protocol/project development, manuscript writing/editing. ER protocol/project development, manuscript writing/editing. VM protocol/project development, manuscript writing/editing. KCZ protocol/project development, data collection or management, data analysis, manuscript writing/editing.
Corresponding author
Ethics declarations
Conflict of interest
Consultants and proctors for Boston Scientific for greenlight: KZ, DSE, VM, ER, HC. Investigators and consultants for PROCEPT BioRobotics: VM, TB, NB, KZ. Surgical tutors for Greenlight Xcelerated Performance System (American Medical System-AMS, Minnetonka, MN) and received honoraria for their tutorship: GF, LC. All other authors do not report any relevant conflicts of interest.
Ethics approval
All procedures performed in this study were in accordance with the ethical standards of the institutional research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
For this type of study, formal consent is not required (retrospective study).
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Nguyen, DD., Sadri, I., Law, K. et al. Impact of the presence of a median lobe on functional outcomes of greenlight photovaporization of the prostate (PVP): an analysis of the Global Greenlight Group (GGG) Database. World J Urol 39, 3881–3889 (2021). https://doi.org/10.1007/s00345-020-03529-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00345-020-03529-w