Abstract
Objective
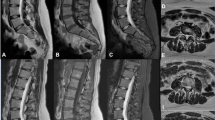
To compare the image quality and diagnostic performance between standard turbo spin-echo MRI and accelerated MRI with deep learning (DL)–based image reconstruction for degenerative lumbar spine diseases.
Materials and methods
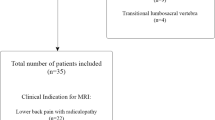
Fifty patients who underwent both the standard and accelerated lumbar MRIs at a 1.5-T scanner for degenerative lumbar spine diseases were prospectively enrolled. DL reconstruction algorithm generated coarse (DL_coarse) and fine (DL_fine) images from the accelerated protocol. Image quality was quantitatively assessed in terms of signal-to-noise ratio (SNR) and contrast-to-noise ratio (CNR) and qualitatively assessed using five-point visual scoring systems. The sensitivity and specificity of four radiologists for the diagnosis of degenerative diseases in both protocols were compared.
Results
The accelerated protocol reduced the average MRI acquisition time by 32.3% as compared to the standard protocol. As compared with standard images, DL_coarse and DL_fine showed significantly higher SNRs on T1-weighted images (T1WI; both p < .001) and T2-weighted images (T2WI; p = .002 and p < 0.001), higher CNRs on T1WI (both p < 0.001), and similar CNRs on T2WI (p = .49 and p = .27). The average radiologist assessment of overall image quality for DL_coarse and DL_fine was higher on sagittal T1WI (p = .04 and p < .001) and axial T2WI (p = .006 and p = .01) and similar on sagittal T2WI (p = .90 and p = .91). Both DL_coarse and DL_fine had better image quality of cauda equina and paraspinal muscles on axial T2WI (both p = .04 for cauda equina; p = .008 and p = .002 for paraspinal muscles). Differences in sensitivity and specificity for the detection of central canal stenosis and neural foraminal stenosis between standard and DL-reconstructed images were all statistically nonsignificant (p ≥ 0.05).
Conclusion
DL-based protocol reduced MRI acquisition time without degrading image quality and diagnostic performance of readers for degenerative lumbar spine diseases.
Clinical relevance statement
The deep learning (DL)–based reconstruction algorithm may be used to further accelerate spine MRI imaging to reduce patient discomfort and increase the cost efficiency of spine MRI imaging.
Key Points
• By using deep learning (DL)–based reconstruction algorithm in combination with the accelerated MRI protocol, the average acquisition time was reduced by 32.3% as compared with the standard protocol.
• DL-reconstructed images had similar or better quantitative/qualitative overall image quality and similar or better image quality for the delineation of most individual anatomical structures.
• The average radiologist’s sensitivity and specificity for the detection of major degenerative lumbar spine diseases, including central canal stenosis, neural foraminal stenosis, and disc herniation, on standard and DL-reconstructed images, were similar.




Similar content being viewed by others
Abbreviations
- CNN:
-
Convolutional neural network
- CNR:
-
Contrast-to-noise ratio
- CSF:
-
Cerebrospinal fluid
- DL:
-
Deep learning
- SNR:
-
Signal-to-noise ratio
- SSIM:
-
Structural similarity index
- T1WI:
-
T1-weighted images
- T2WI:
-
T2-weighted images
- TSE:
-
Turbo spin-echo
References
Ravindra V, Senglaub S, Rattani A et al (2018) Degenerative lumbar spine disease: estimating global incidence and worldwide volume. Global Spine J 8:219256821877076. https://doi.org/10.1177/2192568218770769
Hoy D, Bain C, Williams G et al (2012) A systematic review of the global prevalence of low back pain. Arthritis Rheum 64:2028–2037. https://doi.org/10.1002/art.34347
Lurie J, Tomkins-Lane C (2016) Management of lumbar spinal stenosis. BMJ 352:h6234. https://doi.org/10.1136/bmj.h6234
Balagué F, Mannion AF, Pellisé F, Cedraschi C (2012) Non-specific low back pain. Lancet 379:482–491. https://doi.org/10.1016/S0140-6736(11)60610-7
Humphreys S, Eck J, Hodges S (2002) Neuroimaging in low back pain. Am Fam Physician 65:2299–2306
Sayah A, Jay AK, Toaff JS et al (2016) Effectiveness of a rapid lumbar spine MRI protocol using 3D T2-weighted SPACE imaging versus a standard protocol for evaluation of degenerative changes of the lumbar spine. AJR Am J Roentgenol 207:614–620. https://doi.org/10.2214/AJR.15.15764
Zanchi F, Richard R, Hussami M et al (2020) MRI of non-specific low back pain and/or lumbar radiculopathy: do we need T1 when using a sagittal T2-weighted Dixon sequence? Eur Radiol 30:2583–2593. https://doi.org/10.1007/s00330-019-06626-6
Bratke G, Rau R, Weiss K et al (2019) Accelerated MRI of the lumbar spine using compressed sensing: quality and efficiency. J Magn Reson Imaging 49:e164–e175. https://doi.org/10.1002/jmri.26526
Muckley MJ, Riemenschneider B, Radmanesh A et al (2021) Results of the 2020 fastMRI challenge for machine learning MR image reconstruction. IEEE Trans Med Imaging 40:2306–2317. https://doi.org/10.1109/TMI.2021.3075856
Yoon JH, Nickel MD, Peeters JM, Lee JM (2019) Rapid imaging: recent advances in abdominal MRI for reducing acquisition time and its clinical applications. Korean J Radiol 20:1597–1615
Ye JC (2019) Compressed sensing MRI: a review from signal processing perspective. BMC Biomed Eng 1:8. https://doi.org/10.1186/s42490-019-0006-z
Jaspan O, Fleysher R, Lipton M (2015) Compressed sensing MRI: a review of the clinical literature. Br J Radiol 88:20150487. https://doi.org/10.1259/bjr.20150487
Liang D, Liu B, Wang J, Ying L (2009) Accelerating SENSE using compressed sensing. Magn Reson Med 62:1574–1584. https://doi.org/10.1002/mrm.22161
Sriram A, Zbontar J, Murrell T et al (2020) End-to-End Variational Networks for Accelerated MRI Reconstruction. In: Martel AL, Abolmaesumi P, Stoyanov D et al (eds) Medical image computing and computer assisted intervention – MICCAI 2020. Springer International Publishing, Cham, pp 64–73
Ronneberger O, Fischer P, Brox T (2015) U-Net: convolutional networks for biomedical image segmentation. In: Navab N, Hornegger J, Wells WM, Frangi AF (eds) Medical Image Computing and Computer-Assisted Intervention – MICCAI 2015. Springer International Publishing, Cham, pp 234–241
Jung W, Kim J, Ko J et al (2022) Highly accelerated 3D MPRAGE using deep neural network–based reconstruction for brain imaging in children and young adults. Eur Radiol 32:5468–5479. https://doi.org/10.1007/s00330-022-08687-6
Zeng G, Guo Y, Zhan J et al (2021) A review on deep learning MRI reconstruction without fully sampled k-space. BMC Med Imaging 21:195. https://doi.org/10.1186/s12880-021-00727-9
Kingma D, Ba J (2015) Adam: a method for stochastic optimization. International Conference on Learning Representations, San Diego, CA, USA. https://arxiv.org/abs/1412.6980
Maeder Y, Dunet V, Richard R et al (2017) Bone marrow metastases: T2-weighted Dixon spin-echo fat images can replace T1-weighted spin-echo images. Radiology 286:948–959. https://doi.org/10.1148/radiol.2017170325
Jang S, Song H, Shin YJ et al (2020) Deep learning–based automatic detection algorithm for reducing overlooked lung cancers on chest radiographs. Radiology 296:652–661. https://doi.org/10.1148/radiol.2020200165
Yoo H, Lee SH, Arru CD et al (2021) AI-based improvement in lung cancer detection on chest radiographs: results of a multi-reader study in NLST dataset. Eur Radiol 31:9664–9674. https://doi.org/10.1007/s00330-021-08074-7
Nölte I, Gerigk L, Brockmann MA et al (2008) MRI of degenerative lumbar spine disease: comparison of non-accelerated and parallel imaging. Neuroradiology 50:403–409. https://doi.org/10.1007/s00234-008-0363-0
Hallinan JTPD, Zhu L, Yang K et al (2021) Deep learning model for automated detection and classification of central canal, lateral recess, and neural foraminal stenosis at lumbar spine MRI. Radiology 300:130–138. https://doi.org/10.1148/radiol.2021204289
Fujiwara A, Tamai K, Yamato M et al (1999) The relationship between facet joint osteoarthritis and disc degeneration of the lumbar spine: an MRI study. Eur Spine J 8:396–401. https://doi.org/10.1007/s005860050193
Lee S, Lee JW, Yeom JS et al (2010) A practical MRI grading system for lumbar foraminal stenosis. AJR Am J Roentgenol 194:1095–1098. https://doi.org/10.2214/AJR.09.2772
Li Y, Fredrickson V, Resnick DK (2015) How should we grade lumbar disc herniation and nerve root compression? A systematic review. Clin Orthop Relat Res 473:1896–1902. https://doi.org/10.1007/s11999-014-3674-y
Ko Y, Lee E, Lee JW et al (2020) Clinical validity of two different grading systems for lumbar central canal stenosis: Schizas and Lee classification systems. PLoS One 15:e0233633
Fardon DF, Williams AL, Dohring EJ et al (2014) Lumbar disc nomenclature: version 2.0: Recommendations of the combined task forces of the North American Spine Society, the American Society of Spine Radiology and the American Society of Neuroradiology. Spine J 14:2525–2545. https://doi.org/10.1016/j.spinee.2014.04.022
Ueda T, Ohno Y, Yamamoto K et al (2022) Deep learning reconstruction of diffusion-weighted MRI improves image quality for prostatic imaging. Radiology 303:373–381. https://doi.org/10.1148/radiol.204097
Sun S, Tan ET, Mintz DN et al (2022) Evaluation of deep learning reconstructed high-resolution 3D lumbar spine MRI. Eur Radiol 32:6167–6177. https://doi.org/10.1007/s00330-022-08708-4
Recht MP, Zbontar J, Sodickson DK et al (2020) Using deep learning to accelerate knee MRI at 3 T: results of an interchangeability study. AJR Am J Roentgenol 215:1421–1429. https://doi.org/10.2214/AJR.20.23313
Yeoh H, Hong SH, Ahn C et al (2021) Deep learning algorithm for simultaneous noise reduction and edge sharpening in low-dose CT images: a pilot study using lumbar spine CT. Korean J Radiol 22:1850–1857
Mohammadinejad P, Mileto A, Yu L et al (2021) CT noise-reduction methods for lower-dose scanning: strengths and weaknesses of iterative reconstruction algorithms and new techniques. Radiographics 41:1493–1508. https://doi.org/10.1148/rg.2021200196
Shan H, Padole A, Homayounieh F et al (2019) Competitive performance of a modularized deep neural network compared to commercial algorithms for low-dose CT image reconstruction. Nat Mach Intell 1:269–276. https://doi.org/10.1038/s42256-019-0057-9
Jung W, Kim EH, Ko J et al (2022) Convolutional neural network-based reconstruction for acceleration of prostate T2 weighted MR imaging: a retro- and prospective study. Br J Radiol 95:20211378. https://doi.org/10.1259/bjr.20211378
Yi X, Walia E, Babyn P (2019) Generative adversarial network in medical imaging: a review. Med Image Anal 58:101552. https://doi.org/10.1016/j.media.2019.101552
Acknowledgements
We thank Yunhee Choi at the Division of Medical Statistics, Medical Research Collaborating Center, Seoul National University Hospital for providing advice on statistical interpretation of the data.
Funding
This work was supported by the National Research Foundation of Korea (NRF) grant funded by the Korean government (MSIT) (NRF-2021R1A4A1028713 and NRF-2023R1A2C3003250) and the Korea Medical Device Development Fund grant funded by the Korean government (the Ministry of Science and ICT, South Korea; the Ministry of Trade, Industry and Energy; the Ministry of Health and Welfare, Republic of Korea; and the Ministry of Food and Drug Safety) (project no. 9991007218, KMDF_PR_20200901_0086). This study received technical support and a research grant (grant number 06- 2021–2210) from AIRS Medical Inc.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Guarantor
The scientific guarantor of this publication is Roh-Eul Yoo, Seoul National University Hospital.
Conflict of interest
The authors of this manuscript declare no relationships with any companies, whose products or services may be related to the subject matter of the article.
Roh-Eul Yoo is a Junior Deputy Editor of European Radiology. She has not taken part in the review or selection process of this article.
Statistics and biometry
Yunhee Choi at the Division of Medical Statistics, Medical Research Collaborating Center, Seoul National University Hospital, kindly provided statistical advice for this manuscript.
Informed consent
Written informed consent was obtained from all subjects in this study.
Ethical approval
This study was approved by the institutional review board of Seoul National University Hospital (IRB No.2103-174-1207).
Study subjects or cohorts overlap
None
Methodology
• prospective
• diagnostic study
• performed at one institution
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Yoo, H., Yoo, RE., Choi, S.H. et al. Deep learning–based reconstruction for acceleration of lumbar spine MRI: a prospective comparison with standard MRI. Eur Radiol 33, 8656–8668 (2023). https://doi.org/10.1007/s00330-023-09918-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-023-09918-0