Abstract
Objectives
This study was conducted in order to establish the joint Society of Abdominal Radiology (SAR) and European Society of Urogenital Radiology (ESUR) guidelines on placenta accreta spectrum (PAS) disorders and propose strategies to standardize image acquisition, interpretation, and reporting for this condition with MRI.
Methods
The published evidence-based data and the opinion of experts were combined using the RAND–UCLA Appropriateness Method and formed the basis for these consensus guidelines. The responses of the experts to questions regarding the details of patient preparation, MRI protocol, image interpretation, and reporting were collected, analyzed, and classified as “recommended” versus “not recommended” (if at least 80% consensus among experts) or uncertain (if less than 80% consensus among experts).
Results
Consensus regarding image acquisition, interpretation, and reporting was determined using the RAND–UCLA Appropriateness Method. The use of a tailored MRI protocol and standardized report was recommended.
Conclusions
A standardized imaging protocol and reporting system ensures recognition of the salient features of PAS disorders. These consensus recommendations should be used as a guide for the evaluation of PAS disorders with MRI.
Key Points
• MRI is a powerful adjunct to ultrasound and provides valuable information on the topography and depth of placental invasion.
• Consensus statement proposed a common lexicon to allow for uniformity in MRI acquisition, interpretation, and reporting of PAS disorders.
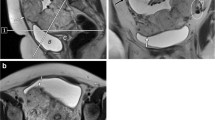
• Seven MRI features, namely intraplacental dark T2 bands, uterine/placental bulge, loss of low T2 retroplacental line, myometrial thinning/disruption, bladder wall interruption, focal exophytic placental mass, and abnormal vasculature of the placental bed, reached consensus and are categorized as “recommended” for diagnosing PAS disorders.




Similar content being viewed by others
Abbreviations
- ACR:
-
American College of Radiology
- BGE:
-
Balanced gradient echo
- DOR:
-
Diagnostic odds ratio
- DWI:
-
Diffusion-weighted imaging
- ECR:
-
European Congress of Radiology
- ESGAR:
-
European Society of Gastrointestinal and Abdominal Radiology
- ESUR:
-
European Society of Urogenital Radiology
- FIGO:
-
International Federation of Gynecology and Obstetrics
- HASTE:
-
Half Fourier single-shot turbo spin echo
- IVF:
-
In vitro fertilization
- NLR:
-
Negative likelihood ratio
- NPV:
-
Negative predictive value
- PAS:
-
Placenta accreta spectrum
- PIWG:
-
Placental Imaging Working Group
- PLR:
-
Positive likelihood ratio
- PPV:
-
Positive predictive value
- SAR:
-
Society of Abdominal Radiology
- SSFSE:
-
Single-shot fast spin echo
- SSH-TSE:
-
Single-shot turbo spin echo
- UFSE:
-
Ultra-fast spin echo
- UOC DFP:
-
Uterine and Ovarian Cancer Disease-Focused Panel
References
Solheim KN, Esakoff TF, Little SE, Cheng YW, Sparks TN, Caughey AB (2011) The effect of cesarean delivery rates on the future incidence of placenta previa, placenta accreta, and maternal mortality. J Matern Fetal Neonatal Med 24:1341–1346
Chen T, Xu XQ, Shi HB, Yang ZQ, Zhou X, Pan Y (2017) Conventional MRI features for predicting the clinical outcome of patients with invasive placenta. Diagn Interv Radiol 23:173–179
Miller DA, Chollet JA, Goodwin TM (1997) Clinical risk factors for placenta previa-placenta accreta. Am J Obstet Gynecol 177:210–214
Clark SL, Koonings PP, Phelan JP (1985) Placenta previa/accreta and prior cesarean section. Obstet Gynecol 66:89–92
Bodelon C, Bernabe-Ortiz A, Schiff MA, Reed SD (2009) Factors associated with peripartum hysterectomy. Obstet Gynecol 114:115–123
** R, Guo Y, Chen Y (2014) Risk factors associated with emergency peripartum hysterectomy. Chin Med J (Engl) 127:900–904
Gielchinsky Y, Rojansky N, Fasouliotis SJ, Ezra Y (2002) Placenta accreta—summary of 10 years: a survey of 310 cases. Placenta 23:210–214
Committee on Obstetric Practice (2012) Committee opinion no. 529: placenta accreta. Obstet Gynecol 120:207–211
Shamshirsaz AA, Fox KA, Salmanian B et al (2015) Maternal morbidity in patients with morbidly adherent placenta treated with and without a standardized multidisciplinary approach. Am J Obstet Gynecol 212(218):e211–e219
Sentilhes L, Kayem G, Chandraharan E et al (2018) FIGO consensus guidelines on placenta accreta spectrum disorders: conservative management. Int J Gynaecol Obstet 140:291–298
Allen L, Jauniaux E, Hobson S, Papillon-Smith J, Belfort MA (2018) FIGO consensus guidelines on placenta accreta spectrum disorders: nonconservative surgical management. Int J Gynaecol Obstet 140:281–290
Jauniaux E, Bhide A, Kennedy A et al (2018) FIGO consensus guidelines on placenta accreta spectrum disorders: prenatal diagnosis and screening. Int J Gynaecol Obstet 140:274–280
Jauniaux E, Chantraine F, Silver RM, Langhoff-Roos J, Diagnosis FPA, Management Expert Consensus Panel (2018) FIGO consensus guidelines on placenta accreta spectrum disorders: epidemiology. Int J Gynaecol Obstet 140:265–273
Jauniaux E, Ayres-de-Campos D, Diagnosis FPA, Management Expert Consensus P (2018) FIGO consensus guidelines on placenta accreta spectrum disorders: introduction. Int J Gynaecol Obstet 140:261–264
Matsubara S, Jauniaux E (2018) Placenta accreta spectrum disorders: a new standardized terminology better defining the condition. J Obstet Gynaecol Res 44:1338–1339
Morel O, Collins SL, Uzan-Augui J et al (2019) A proposal for standardized magnetic resonance imaging (MRI) descriptors of abnormally invasive placenta (AIP)—from the International Society for AIP. Diagn Interv Imaging. https://doi.org/10.1016/j.diii.2019.02.004
Jauniaux E, Collins S, Burton GJ (2018) Placenta accreta spectrum: pathophysiology and evidence-based anatomy for prenatal ultrasound imaging. Am J Obstet Gynecol 218:75–87
Beets-Tan RGH, Lambregts DMJ, Maas M et al (2018) Magnetic resonance imaging for clinical management of rectal cancer: updated recommendations from the 2016 European Society of Gastrointestinal and Abdominal Radiology (ESGAR) consensus meeting. Eur Radiol 28:1465–1475
Nougaret S, Horta M, Sala E et al (2019) Endometrial cancer MRI staging: updated guidelines of the European Society of Urogenital Radiology. Eur Radiol 29:792–805
Expert Panel on MR Safety, Kanal E, Barkovich AJ et al (2013) ACR guidance document on MR safe practices: 2013. J Magn Reson Imaging 37:501–530
Ray JG, Vermeulen MJ, Bharatha A, Montanera WJ, Park AL (2016) Association between MRI exposure during pregnancy and fetal and childhood outcomes. JAMA 316:952–961
Horowitz JM, Berggruen S, McCarthy RJ et al (2015) When timing is everything: are placental MRI examinations performed before 24 weeks’ gestational age reliable? AJR Am J Roentgenol 205:685–692
Derman AY, Nikac V, Haberman S, Zelenko N, Opsha O, Flyer M (2011) MRI of placenta accreta: a new imaging perspective. AJR Am J Roentgenol 197:1514–1521
Lax A, Prince MR, Mennitt KW, Schwebach JR, Budorick NE (2007) The value of specific MRI features in the evaluation of suspected placental invasion. Magn Reson Imaging 25:87–93
D’Antonio F, Iacovella C, Palacios-Jaraquemada J, Bruno CH, Manzoli L, Bhide A (2014) Prenatal identification of invasive placentation using magnetic resonance imaging: systematic review and meta-analysis. Ultrasound Obstet Gynecol 44:8–16
Ueno Y, Kitajima K, Kawakami F et al (2014) Novel MRI finding for diagnosis of invasive placenta praevia: evaluation of findings for 65 patients using clinical and histopathological correlations. Eur Radiol 24:881–888
Goergen SK, Posma E, Wrede D et al (2018) Interobserver agreement and diagnostic performance of individual MRI criteria for diagnosis of placental adhesion disorders. Clin Radiol 73:908 e901–908 e909
Lim PS, Greenberg M, Edelson MI, Bell KA, Edmonds PR, Mackey AM (2011) Utility of ultrasound and MRI in prenatal diagnosis of placenta accreta: a pilot study. AJR Am J Roentgenol 197:1506–1513
Familiari A, Liberati M, Lim P et al (2018) Diagnostic accuracy of magnetic resonance imaging in detecting the severity of abnormal invasive placenta: a systematic review and meta-analysis. Acta Obstet Gynecol Scand 97:507–520
Azour L, Besa C, Lewis S, Kamath A, Oliver ER, Taouli B (2016) The gravid uterus: MR imaging and reporting of abnormal placentation. Abdom Radiol (NY) 41:2411–2423
Leyendecker JR, DuBose M, Hosseinzadeh K et al (2012) MRI of pregnancy-related issues: abnormal placentation. AJR Am J Roentgenol 198:311–320
Alamo L, Anaye A, Rey J et al (2013) Detection of suspected placental invasion by MRI: do the results depend on observer’ experience? Eur J Radiol 82:e51–e57
Baughman WC, Corteville JE, Shah RR (2008) Placenta accreta: spectrum of US and MR imaging findings. Radiographics 28:1905–1916
Masselli G, Gualdi G (2013) MR imaging of the placenta: what a radiologist should know. Abdom Imaging 38:573–587
Jha P, Rabban J, Chen LM et al (2019) Placenta accreta spectrum: value of placental bulge as a sign of myometrial invasion on MR imaging. Abdom Radiol (NY). https://doi.org/10.1007/s00261-019-02008-0
Allen BC, Leyendecker JR (2013) Placental evaluation with magnetic resonance. Radiol Clin North Am 51:955–966
Bour L, Place V, Bendavid S et al (2014) Suspected invasive placenta: evaluation with magnetic resonance imaging. Eur Radiol 24:3150–3160
Twickler DM, Lucas MJ, Balis AB et al (2000) Color flow map** for myometrial invasion in women with a prior cesarean delivery. J Matern Fetal Med 9:330–335
Maldjian C, Adam R, Pelosi M, Pelosi M 3rd, Rudelli RD, Maldjian J (1999) MRI appearance of placenta percreta and placenta accreta. Magn Reson Imaging 17:965–971
Kim JA, Narra VR (2004) Magnetic resonance imaging with true fast imaging with steady-state precession and half-Fourier acquisition single-shot turbo spin-echo sequences in cases of suspected placenta accreta. Acta Radiol 45:692–698
Bourgioti C, Zafeiropoulou K, Fotopoulos S et al (2018) MRI features predictive of invasive placenta with extrauterine spread in high-risk gravid patients: a prospective evaluation. AJR Am J Roentgenol 211:701–711
Elsayes KM, Trout AT, Friedkin AM et al (2009) Imaging of the placenta: a multimodality pictorial review. Radiographics 29:1371–1391
Palacios Jaraquemada JM, Bruno CH (2005) Magnetic resonance imaging in 300 cases of placenta accreta: surgical correlation of new findings. Acta Obstet Gynecol Scand 84:716–724
Thiravit S, Lapatikarn S, Muangsomboon K, Suvannarerg V, Thiravit P, Korpraphong P (2017) MRI of placenta percreta: differentiation from other entities of placental adhesive disorder. Radiol Med 122:61–68
Valentini AL, Gui B, Ninivaggi V et al (2017) The morbidly adherent placenta: when and what association of signs can improve MRI diagnosis? Our experience. Diagn Interv Radiol 23:180–186
Kumar I, Verma A, Ojha R, Shukla RC, Jain M, Srivastava A (2017) Invasive placental disorders: a prospective US and MRI comparative analysis. Acta Radiol 58:121–128
Pijnenborg R, Brosens I, Romero R (2010) Placental bed disorders: basic science and its translation to obstetrics. Cambridge University Press
Chantraine F, Blacher S, Berndt S et al (2012) Abnormal vascular architecture at the placental-maternal interface in placenta increta. Am J Obstet Gynecol 207(188):e181–e189
Jauniaux E, Collins SL, Jurkovic D, Burton GJ (2016) Accreta placentation: a systematic review of prenatal ultrasound imaging and grading of villous invasiveness. Am J Obstet Gynecol 215:712–721
Chen X, Shan R, Zhao L et al (2018) Invasive placenta previa: placental bulge with distorted uterine outline and uterine serosal hypervascularity at 1.5T MRI—useful features for differentiating placenta percreta from placenta accreta. Eur Radiol 28:708–717
Bourgioti C, Zafeiropoulou K, Fotopoulos S et al (2018) MRI prognosticators for adverse maternal and neonatal clinical outcome in patients at high risk for placenta accreta spectrum (PAS) disorders. J Magn Reson Imaging. https://doi.org/10.1002/jmri.26592
Publications Committee, Society for Maternal-Fetal Medicine, Belfort MA (2010) Placenta accreta. Am J Obstet Gynecol 203:430–439
Palacios-Jaraquemada JMKM, Keith LG (2012) Uterovaginal blood supply: the S1 and S2 segmental concepts and their clinical relevance. Sapiens Publishing Ltd, Meadowbank
Palacios-Jaraquemada JM (2013) Caesarean section in cases of placenta praevia and accreta. Best Pract Res Clin Obstet Gynaecol 27:221–232
Funding
The authors state that this work has not received any funding.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Guarantor
The scientific guarantor of this publication is Gabriele Masseli.
Conflict of interest
The authors declare that they have no conflict of interest.
Statistics and biometry
One of the authors has significant statistical expertise.
Informed consent
Written informed consent was not required for this study because this is a consensus statement.
Ethical approval
Institutional Review Board approval was not required as no patient information was accessed for this study.
Study subjects or cohorts overlap
Some study subjects or cohorts have been previously reported in previous studies referenced in the manuscript.
Methodology
• Retrospective
• Observational
• Multicenter study
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Jha, P., Pōder, L., Bourgioti, C. et al. Society of Abdominal Radiology (SAR) and European Society of Urogenital Radiology (ESUR) joint consensus statement for MR imaging of placenta accreta spectrum disorders. Eur Radiol 30, 2604–2615 (2020). https://doi.org/10.1007/s00330-019-06617-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-019-06617-7