Abstract
Background
Bilateral idiopathic hyperaldosteronism (IHA) is responsible for 60% of primary aldosteronism (PA) cases. Medical management is standard of care for IHA. Unilateral adrenalectomy (UA) with the intent of debulking total aldosterone production as a palliative measure remains controversial.
Methods
Single-center retrospective review (2010–2020) of patients undergoing UA with a diagnosis of PA due to IHA (lateralization index [LI] on adrenal venous sampling [AVS] < 4). Demographic, pre-operative, intra-operative, and post-operative variables were assessed. Hypertensive regimens were converted to the WHO Defined Daily Dose (DDD).
Results
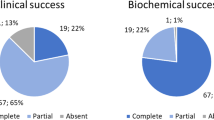
Twenty-four patients were identified, 14, 58% male and mean age 52 ± 10 years. Preoperative hypokalemia was present in 22, 92% of patients. Median number of antihypertensives taken was 3 (interquartile range [IQR], 2–4) and median DDD was 4 (IQR, 3–5.3). Median lateralization index on AVS was 3.52 (range, 1.19–3.88). All operations were performed in minimally invasive fashion. There were no conversions to open procedure, ICU admissions, or post-operative complications. Median follow-up was 10.5 months (range, 1–145 months). Hypokalemia resolved in 17, 76% of patients at last follow-up. Post-operative median number of antihypertensives taken was 1 (IQR, 1–3) and median DDD was 2 (IQR, 0.5–2.75) from 4, P = 0.003. Three (%) patients required continuation of mineralocorticoid receptor antagonists post-operatively. Blood pressure control improved in 65% of patients.
Conclusion
Unilateral adrenalectomy in the setting of bilateral hyperaldosteronism can improve blood pressure control and stabilize potassium levels in selected patients. Further prospective studies in larger cohorts will be necessary to further define the role of unilateral adrenalectomy in the setting of PA due to bilateral adrenal disease.
Similar content being viewed by others
References
Reincke M, Bancos I, Mulatero P, Scholl UI, Stowasser M, Williams TA (2021) Diagnosis and treatment of primary aldosteronism. Lancet Diabetes Endocrinol 9(12):876–892. https://doi.org/10.1016/S2213-8587(21)00210-2
Käyser SC, Dekkers T, Groenewoud HJ et al (2016) Study heterogeneity and estimation of prevalence of primary aldosteronism: a systematic review and meta-regression analysis. J Clin Endocrinol Metab 101(7):2826–2835. https://doi.org/10.1210/jc.2016-1472
Williams TA, Lenders JWM, Mulatero P et al (2017) Outcomes after adrenalectomy for unilateral primary aldosteronism: an international consensus on outcome measures and analysis of remission rates in an international cohort. Lancet Diabetes Endocrinol 5(9):689–699. https://doi.org/10.1016/S2213-8587(17)30135-3
Lim V, Guo Q, Grant CS et al (2014) Accuracy of adrenal imaging and adrenal venous sampling in predicting surgical cure of primary aldosteronism. J Clin Endocrinol Metab 99(8):2712–2719. https://doi.org/10.1210/jc.2013-4146
Adolf C, Heinrich DA, Holler F et al (2020) Patients with primary aldosteronism respond to unilateral adrenalectomy with long-term reduction in salt intake. J Clin Endocrinol Metab 105(3):e484–e493. https://doi.org/10.1210/clinem/dgz051
Muth A, Ragnarsson O, Johannsson G, Wängberg B (2015) Systematic review of surgery and outcomes in patients with primary aldosteronism. Br J Surg 102(4):307–317. https://doi.org/10.1002/bjs.9744
Monticone S, D’Ascenzo F, Moretti C et al (2018) Cardiovascular events and target organ damage in primary aldosteronism compared with essential hypertension: a systematic review and meta-analysis. Lancet Diabetes Endocrinol 6(1):41–50. https://doi.org/10.1016/S2213-8587(17)30319-4
Catena C, Colussi G, Di Fabio A et al (2010) Mineralocorticoid antagonists treatment versus surgery in primary aldosteronism. Horm Metab Res 42(06):440–445. https://doi.org/10.1055/s-0029-1246185
Young WF (2019) Diagnosis and treatment of primary aldosteronism: practical clinical perspectives. J Intern Med 285(2):126–148. https://doi.org/10.1111/joim.12831
Funder JW, Carey RM, Mantero F et al (2016) The management of primary aldosteronism: case detection, diagnosis, and treatment: an endocrine society clinical practice guideline. J Clin Endocrinol Metab 101(5):1889–1916. https://doi.org/10.1210/jc.2015-4061
Osswald A, Quinkler M, Di Dalmazi G et al (2019) Long-term outcome of primary bilateral macronodular adrenocortical hyperplasia after unilateral adrenalectomy. J Clin Endocrinol Metab 104(7):2985–2993. https://doi.org/10.1210/jc.2018-02204
Debillon E, Velayoudom-Cephise FL, Salenave S et al (2015) Unilateral adrenalectomy as a first-line treatment of cushing’s syndrome in patients with primary bilateral macronodular adrenal hyperplasia. J Clin Endocrinol Metab 100(12):4417–4424. https://doi.org/10.1210/jc.2015-2662
Young WF, Stanson AW (2009) What are the keys to successful adrenal venous sampling (AVS) in patients with primary aldosteronism? Clin Endocrinol (Oxf) 70(1):14–17. https://doi.org/10.1111/j.1365-2265.2008.03450.x
Min L, Ha JK, Aubert CE et al (2021) A method to quantify mean hypertension treatment daily dose intensity using health care system data. JAMA Netw Open 4(1):e2034059. https://doi.org/10.1001/jamanetworkopen.2020.34059
Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG (2009) Research electronic data capture (REDCap)—a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform 42(2):377–381. https://doi.org/10.1016/j.jbi.2008.08.010
Shariq OA, Bews KA, McKenna NP et al (2021) Is same-day discharge associated with increased 30-day postoperative complications and readmissions in patients undergoing laparoscopic adrenalectomy? Surgery 169(2):289–297. https://doi.org/10.1016/j.surg.2020.08.018
Sukor N, Gordon RD, Ku YK, Jones M, Stowasser M (2009) Role of unilateral adrenalectomy in bilateral primary aldosteronism: a 22-year single center experience. J Clin Endocrinol Metab 94(7):2437–2445. https://doi.org/10.1210/jc.2008-2803
Ahmed AH, Gordon RD, Sukor N, Pimenta E, Stowasser M (2011) Quality of life in patients with bilateral primary aldosteronism before and during treatment with spironolactone and/or amiloride, including a comparison with our previously published results in those with unilateral disease treated surgically. J Clin Endocrinol Metab 96(9):2904–2911. https://doi.org/10.1210/jc.2011-0138
Acknowledgements
Authors report no proprietary or commercial interest in any product mentioned or concept discussed in this article. All research was produced at Mayo Clinic Rochester, MN. This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
No authors report any proprietary or commercial interest in any product mentioned or concept discussed in this article.
Ethical approval
This single-center retrospective review was approved by the Mayo Foundation Institutional Review Board and complies with all ethical requirements.
Informed consent
Informed consent was obtained from all individuals included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Szabo Yamashita, T., Shariq, O.A., Foster, T.R. et al. Unilateral Adrenalectomy for Primary Aldosteronism Due to Bilateral Adrenal Disease Can Result in Resolution of Hypokalemia and Amelioration of Hypertension. World J Surg 47, 314–318 (2023). https://doi.org/10.1007/s00268-022-06780-x
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-022-06780-x