Abstract
Metabolic dysregulation in the hypoxic tumor microenvironment (TME) is considered as a hallmark of solid tumors, leading to changes in biosynthetic pathways favoring onset, survival and proliferation of malignant cells. Within the TME, hypoxic milieu favors metabolic reprogramming of tumor cells, which subsequently affects biological properties of tumor-infiltrating immune cells. T regulatory cells (Tregs), including both circulating and tissue-resident cells, are particularly susceptible to hypoxic metabolic signaling that can reprogram their biological and physicochemical properties. Furthermore, metabolic reprogramming modifies Tregs to utilize alternative substrates and undergo a plethora of metabolic events to meet their energy demands. Major impact of this metabolic reprogramming can result in differentiation, survival, excessive secretion of immunosuppressive cytokines and proliferation of Tregs within the TME, which in turn dampen anti-tumor immune responses. Studies on fine-tuning of Treg metabolism are challenging due to heterogenicity of tissue-resident Tregs and their dynamic functions. In this review, we highlight tumor intrinsic and extrinsic factors, which can influence Treg metabolism in the hypoxic TME. Moreover, we focus on metabolic reprogramming of Tregs that could unveil potential regulatory networks favoring tumorigenesis/progression, and provide novel insights, including inhibitors against acetyl-coA carboxylase 1 and transforming growth factor beta into targeting Treg metabolism for therapeutic benefits.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
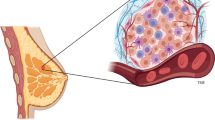
Cancers are polygenic diseases initiated by multiple oncogenic factors that dysregulate the expression of tumor suppressor genes and/or proto-oncogenes leading to malignant progression [1]. The neoplastic tissue is comprised of heterogeneous population of tumor cells, in a milieu of immune (e.g., myeloid cells, lymphocytes, and natural-killer cells), and non-immune cells (e.g., fibroblasts and endothelial cells) embedded in the extracellular matrix with a plethora of cytokines and chemokines, known as tumor microenvironment (TME) [2,3,4]. TME has dynamic attributes with pro- and anti-tumorigenic properties, which can also influence drug responses [5]. Tumor cells evade host-immunosurveillance by recruiting surplus of immunosuppressive cells including T regulatory cells (Tregs) [6, 7] and myeloid-derived suppressive cells (MDSCs) [6], which suppress the proliferation of cytotoxic T cells (CTLs) and favor malignant progression [8]. Amongst these suppressive cells, Tregs are considered as the master-regulatory cells, which not only secrete cytokines that promote onset and proliferation of malignancies, but also play indispensable roles in the induction of neo-angiogenesis and metastasis [9,10,11,12]. Accumulating evidence suggest that Treg infiltration was evident in vast majority of solid tumors including breast [7], colon [6], pancreatic [13] and ovarian cancer [9]. Tumors samples from advanced stages of cancer exhibit higher infiltration of Tregs, compared with samples obtained from early stages of cancer [14]. Moreover, meta-data analyses showed that higher Treg infiltration is negatively correlated with cytotoxic CD8+ T cell infiltration and that is associated with poor-disease prognosis [15]. Currently, it is believed that Treg infiltration favors tumor progression and dampens anti-tumor immune responses; thus, it is essential to understand the progression and functions of Tregs in the TME [16, 17].
Tumor cells adapt to multiple metabolic processes including glycolysis, oxidative phosphorylation (OXPHOS) and fatty acid metabolism to obtain energy for their survival and progression in adverse tumor milieu [18]. Moreover, the differentiation of T cells within the TME is indirectly regulated by tumor-mediated metabolites and favors tumor progression [19]. Within the TME, metabolic reprogramming of T cells is initiated by the activation of T cell receptor (TCR) signaling along with various costimulatory molecules, resulting in the production of sufficient ATP to meet energy requirements for T cell proliferation and effector functions [20]. Interestingly, T cells isolated from the TME frequently exhibit exhaustive T cell markers and possess distinct metabolic signatures including reduction in the uptake of glucose and upregulation of reactive oxygen species (ROS) [21]. These metabolic defects could be circumvented and partially restored the activation of tumor-infiltrating CD8+ T cells (TILs) through the adequate supplementation of pyruvate and neutralization of ROS [21]. These reports suggest that tumor metabolic environment could alter the regulation, function and tumor-antigen recognition of T cells, leading to inadequate anti-tumor responses.
It has been reported that accumulation of lactate and carbon dioxide could efficiently reprogram the metabolic potentials of tumor cells, including elevated nutrient uptake and glucose metabolism and favor the differentiation of Tregs by inhibiting the infiltration of effector T cells within the TME [22, 23]. Moreover, hypoxic conditions as a result of increased tumor growth and oxygen deprivation stabilize the expression of hypoxia‐inducible factor 1‐α (HIF1‐α), which in turn mediates the induction of FoxP3 expression and favors Treg stability [24, 25]. Therefore, comprehensive analyses of malignancy-induced metabolic/hypoxic regulation of T cells can improve current immunotherapeutic modalities. Numerous studies have focused on the metabolic reprogramming of tumor cells and their influence over T cell function within the TME; however, limited data are available on the metabolic-induced alterations in Tregs in the TME. This review highlights the metabolic reprogramming of physicochemical characteristics of Tregs, their function, differentiation and crosstalk within the TME. Additionally, we focus on the potential metabolic pathways of Tregs within the TME, which may be targeted for improvement of prognosis and development of novel therapeutic strategies.
Metabolism in the tumor microenvironment
Tumor cells are characterized by their competence to adapt with altering environmental cues by exploiting various nutrients to uphold their necessitating anabolic requirements [3]. This sustained energy demand is accomplished by adequate supply of nutrients and oxygen via tumor vasculature [26]. Consequently, these extracellular nutrients are indispensable for cancer cells to meet their high-energy demand during rapid, uncontrolled proliferation [26]. Unlike normal cells, malignant cells have higher metabolic plasticity, which could reshape the environment even in nutrient-deprived conditions per se [27]. This plasticity has profound influence on tumor differentiation and gene expression within the TME [27]. In this context, Pavlova and colleagues classified tumor-associated metabolic modifications into six groups: (1) deregulation in glucose and amino acid metabolism, (2) altered nutrient uptake, (3) utilization of intermediates from citric acid cycle (TCA cycle)/glycolysis for the biosynthesis of nicotinamide adenine dinucleotide phosphate (NADPH), (4) increased nitrogen requirement, (5) variations in the regulation of metabolite-dependent gene expression and (6) interactions between metabolic pathways within the TME [27].
It has been reported that the highly proliferating cancer cells modify the metabolic components of the TME. For instance, malignant cells take up higher amount of glucose leading to the biosynthesis of large amount of lactate, which could influence many cell populations within the TME [28]. Higher accumulation of lactate creates an immune-subversive milieu by reducing dendritic and T cell activation and migration of tumor-associated macrophages/monocytes [28, 29]. Moreover, the excess accumulation of lactate polarizes resident macrophages to highly activated/ immunosuppressive M2 state and promotes angiogenesis [30, 31]. Excess levels of lactate also favor the biosynthesis of hyaluronic acid by fibroblasts, contributing to higher tumor invasiveness [32].
Hypoxia-inducible factor 1-alpha (HIF-1α) is the key transcriptional factor of hypoxic cells, a hallmark of the TME, and is a downstream target of glucose transporter-1 (GLUT-1) [33]. During hypoxic conditions, the higher glucose uptake by cancer cells could upregulate the stability of HIF-1α, which in turn leads to the attenuation of anti-tumor immune responses [34]. In HIF-1α-knocked-out murine models, the anti-tumor immune responses of CD8+ TILs improve through the activation of peroxisome-activated receptor α (PPARα) signaling and also elevated metabolism of fatty acids [ A Correction to this paper has been published: https://doi.org/10.1007/s00262-021-02999-0 Bredberg A (2011) Cancer: more of polygenic disease and less of multiple mutations? A quantitative viewpoint. Cancer 117(3):440–445. https://doi.org/10.1002/cncr.25440 Du G, Liu Y, Li J, Liu W, Wang Y, Li H (2013) Hypothermic microenvironment plays a key role in tumor immune subversion. Int Immunopharmacol 17(2):245–253. https://doi.org/10.1016/j.intimp.2013.06.018 Hanahan D, Weinberg RA (2011) Hallmarks of cancer: the next generation. Cell 144(5):646–674. https://doi.org/10.1016/j.cell.2011.02.013 Whiteside TL (2008) The tumor microenvironment and its role in promoting tumor growth. Oncogene 27(45):5904–5912. https://doi.org/10.1038/onc.2008.271 Tredan O, Galmarini CM, Patel K, Tannock IF (2007) Drug resistance and the solid tumor microenvironment. J Natl Cancer Inst 99(19):1441–1454. https://doi.org/10.1093/jnci/djm135 Syed Khaja AS, Toor SM, El Salhat H, Ali BR, Elkord E (2017) Intratumoral FoxP3(+)Helios(+) regulatory T cells upregulating immunosuppressive molecules are expanded in human colorectal cancer. Front Immunol 8:619. https://doi.org/10.3389/fimmu.2017.00619 Syed Khaja AS, Toor SM, El Salhat H, Faour I, Ul Haq N, Ali BR, Elkord E (2017) Preferential accumulation of regulatory T cells with highly immunosuppressive characteristics in breast tumor microenvironment. Oncotarget 8(20):33159–33171. https://doi.org/10.18632/oncotarget.16565 Chaudhary B, Elkord E (2016) Regulatory T cells in the tumor microenvironment and cancer progression: role and therapeutic targeting. Vaccines Basel. https://doi.org/10.3390/vaccines4030028 Curiel TJ, Coukos G, Zou L, Alvarez X, Cheng P, Mottram P, Evdemon-Hogan M, Conejo-Garcia JR, Zhang L, Burow M, Zhu Y, Wei S, Kryczek I, Daniel B, Gordon A, Myers L, Lackner A, Disis ML, Knutson KL, Chen L, Zou W (2004) Specific recruitment of regulatory T cells in ovarian carcinoma fosters immune privilege and predicts reduced survival. Nat Med 10(9):942–949. https://doi.org/10.1038/nm1093 Facciabene A, Peng X, Hagemann IS, Balint K, Barchetti A, Wang LP, Gimotty PA, Gilks CB, Lal P, Zhang L, Coukos G (2011) Tumour hypoxia promotes tolerance and angiogenesis via CCL28 and T(reg) cells. Nature 475(7355):226–230. https://doi.org/10.1038/nature10169 Tan W, Zhang W, Strasner A, Grivennikov S, Cheng JQ, Hoffman RM, Karin M (2011) Tumour-infiltrating regulatory T cells stimulate mammary cancer metastasis through RANKL-RANK signalling. Nature 470(7335):548–553. https://doi.org/10.1038/nature09707 Wei S, Kryczek I, Edwards RP, Zou L, Szeliga W, Banerjee M, Cost M, Cheng P, Chang A, Redman B, Herberman RB, Zou W (2007) Interleukin-2 administration alters the CD4+FOXP3+ T-cell pool and tumor trafficking in patients with ovarian carcinoma. Cancer Res 67(15):7487–7494. https://doi.org/10.1158/0008-5472.CAN-07-0565 Liyanage UK, Moore TT, Joo HG, Tanaka Y, Herrmann V, Doherty G, Drebin JA, Strasberg SM, Eberlein TJ, Goedegebuure PS, Linehan DC (2002) Prevalence of regulatory T cells is increased in peripheral blood and tumor microenvironment of patients with pancreas or breast adenocarcinoma. J Immunol 169(5):2756–2761. https://doi.org/10.4049/jimmunol.169.5.2756 Bates GJ, Fox SB, Han C, Leek RD, Garcia JF, Harris AL, Banham AH (2006) Quantification of regulatory T cells enables the identification of high-risk breast cancer patients and those at risk of late relapse. J Clin Oncol 24(34):5373–5380. https://doi.org/10.1200/JCO.2006.05.9584 Shang B, Liu Y, Jiang SJ, Liu Y (2015) Prognostic value of tumor-infiltrating FoxP3+ regulatory T cells in cancers: a systematic review and meta-analysis. Sci Rep 5:15179. https://doi.org/10.1038/srep15179 Bauer CA, Kim EY, Marangoni F, Carrizosa E, Claudio NM, Mempel TR (2014) Dynamic Treg interactions with intratumoral APCs promote local CTL dysfunction. J Clin Invest 124(6):2425–2440. https://doi.org/10.1172/JCI66375 Tada Y, Togashi Y, Kotani D, Kuwata T, Sato E, Kawazoe A, Doi T, Wada H, Nishikawa H, Shitara K (2018) Targeting VEGFR2 with Ramucirumab strongly impacts effector/ activated regulatory T cells and CD8(+) T cells in the tumor microenvironment. J Immunother Cancer 6(1):106. https://doi.org/10.1186/s40425-018-0403-1 Phan LM, Yeung SC, Lee MH (2014) Cancer metabolic reprogramming: importance, main features, and potentials for precise targeted anti-cancer therapies. Cancer Biol Med 11(1):1–19. https://doi.org/10.7497/j.issn.2095-3941.2014.01.001 Hope HC, Salmond RJ (2019) Targeting the tumor microenvironment and T cell metabolism for effective cancer immunotherapy. Eur J Immunol 49(8):1147–1152. https://doi.org/10.1002/eji.201848058 Chang CH, Curtis JD, Maggi LB Jr, Faubert B, Villarino AV, O’Sullivan D, Huang SC, van der Windt GJ, Blagih J, Qiu J, Weber JD, Pearce EJ, Jones RG, Pearce EL (2013) Posttranscriptional control of T cell effector function by aerobic glycolysis. Cell 153(6):1239–1251. https://doi.org/10.1016/j.cell.2013.05.016 Siska PJ, Beckermann KE, Mason FM, Andrejeva G, Greenplate AR, Sendor AB, Chiang YJ, Corona AL, Gemta LF, Vincent BG, Wang RC, Kim B, Hong J, Chen CL, Bullock TN, Irish JM, Rathmell WK, Rathmell JC (2017) Mitochondrial dysregulation and glycolytic insufficiency functionally impair CD8 T cells infiltrating human renal cell carcinoma. JCI Insight. https://doi.org/10.1172/jci.insight.93411 Kouidhi S, Elgaaied AB, Chouaib S (2017) Impact of metabolism on T-cell differentiation and function and cross talk with tumor microenvironment. Front Immunol 8:270. https://doi.org/10.3389/fimmu.2017.00270 Warburg O, Wind F, Negelein E (1927) The metabolism of tumors in the body. J Gen Physiol 8(6):519–530. https://doi.org/10.1085/jgp.8.6.519 Ben-Shoshan J, Maysel-Auslender S, Mor A, Keren G, George J (2008) Hypoxia controls CD4+CD25+ regulatory T-cell homeostasis via hypoxia-inducible factor-1alpha. Eur J Immunol 38(9):2412–2418. https://doi.org/10.1002/eji.200838318 Neildez-Nguyen TMA, Bigot J, Da Rocha S, Corre G, Boisgerault F, Paldi A, Galy A (2015) Hypoxic culture conditions enhance the generation of regulatory T cells. Immunology 144(3):431–443. https://doi.org/10.1111/imm.12388 Guillaumond F, Leca J, Olivares O, Lavaut MN, Vidal N, Berthezene P, Dusetti NJ, Loncle C, Calvo E, Turrini O, Iovanna JL, Tomasini R, Vasseur S (2013) Strengthened glycolysis under hypoxia supports tumor symbiosis and hexosamine biosynthesis in pancreatic adenocarcinoma. Proc Natl Acad Sci U S A 110(10):3919–3924. https://doi.org/10.1073/pnas.1219555110 Pavlova NN, Thompson CB (2016) The emerging hallmarks of cancer metabolism. Cell Metab 23(1):27–47. https://doi.org/10.1016/j.cmet.2015.12.006 Fischer K, Hoffmann P, Voelkl S, Meidenbauer N, Ammer J, Edinger M, Gottfried E, Schwarz S, Rothe G, Hoves S, Renner K, Timischl B, Mackensen A, Kunz-Schughart L, Andreesen R, Krause SW, Kreutz M (2007) Inhibitory effect of tumor cell-derived lactic acid on human T cells. Blood 109(9):3812–3819. https://doi.org/10.1182/blood-2006-07-035972 Goetze K, Walenta S, Ksiazkiewicz M, Kunz-Schughart LA, Mueller-Klieser W (2011) Lactate enhances motility of tumor cells and inhibits monocyte migration and cytokine release. Int J Oncol 39(2):453–463. https://doi.org/10.3892/ijo.2011.1055 Colegio OR, Chu NQ, Szabo AL, Chu T, Rhebergen AM, Jairam V, Cyrus N, Brokowski CE, Eisenbarth SC, Phillips GM, Cline GW, Phillips AJ, Medzhitov R (2014) Functional polarization of tumour-associated macrophages by tumour-derived lactic acid. Nature 513(7519):559–563. https://doi.org/10.1038/nature13490 Constant JS, Feng JJ, Zabel DD, Yuan H, Suh DY, Scheuenstuhl H, Hunt TK, Hussain MZ (2000) Lactate elicits vascular endothelial growth factor from macrophages: a possible alternative to hypoxia. Wound Repair Regen 8(5):353–360. https://doi.org/10.1111/j.1524-475x.2000.00353.x Stern R, Shuster S, Neudecker BA, Formby B (2002) Lactate stimulates fibroblast expression of hyaluronan and CD44: the Warburg effect revisited. Exp Cell Res 276(1):24–31. https://doi.org/10.1006/excr.2002.5508 Zhang JZ, Behrooz A, Ismail-Beigi F (1999) Regulation of glucose transport by hypoxia. Am J Kidney Dis 34(1):189–202. https://doi.org/10.1016/s0272-6386(99)70131-9 Nagao A, Kobayashi M, Koyasu S, Chow CCT, Harada H (2019) HIF-1-dependent reprogramming of glucose metabolic pathway of cancer cells and its therapeutic significance. Int J Mol Sci. https://doi.org/10.3390/ijms20020238 Zhang Y, Kurupati R, Liu L, Zhou XY, Zhang G, Hudaihed A, Filisio F, Giles-Davis W, Xu X, Karakousis GC, Schuchter LM, Xu W, Amaravadi R, **ao M, Sadek N, Krepler C, Herlyn M, Freeman GJ, Rabinowitz JD, Ertl HCJ (2017) Enhancing CD8(+) T cell fatty acid catabolism within a metabolically challenging tumor microenvironment increases the efficacy of melanoma immunotherapy. Cancer Cell 32(3):377–391 e379. https://doi.org/10.1016/j.ccell.2017.08.004 Miska J, Lee-Chang C, Rashidi A, Muroski ME, Chang AL, Lopez-Rosas A, Zhang P, Panek WK, Cordero A, Han Y, Ahmed AU, Chandel NS, Lesniak MS (2019) HIF-1alpha is a metabolic switch between glycolytic-driven migration and oxidative phosphorylation-driven immunosuppression of tregs in glioblastoma. Cell Rep 27(1):226–237 e224. https://doi.org/10.1016/j.celrep.2019.03.029 Michalek RD, Gerriets VA, Jacobs SR, Macintyre AN, MacIver NJ, Mason EF, Sullivan SA, Nichols AG, Rathmell JC (2011) Cutting edge: distinct glycolytic and lipid oxidative metabolic programs are essential for effector and regulatory CD4+ T cell subsets. J Immunol 186(6):3299–3303. https://doi.org/10.4049/jimmunol.1003613 Munn DH, Mellor AL (2007) Indoleamine 2,3-dioxygenase and tumor-induced tolerance. J Clin Invest 117(5):1147–1154. https://doi.org/10.1172/JCI31178 Fallarino F, Grohmann U, Vacca C, Bianchi R, Orabona C, Spreca A, Fioretti MC, Puccetti P (2002) T cell apoptosis by tryptophan catabolism. Cell Death Differ 9(10):1069–1077. https://doi.org/10.1038/sj.cdd.4401073 Fallarino F, Grohmann U, You S, McGrath BC, Cavener DR, Vacca C, Orabona C, Bianchi R, Belladonna ML, Volpi C, Santamaria P, Fioretti MC, Puccetti P (2006) The combined effects of tryptophan starvation and tryptophan catabolites down-regulate T cell receptor zeta-chain and induce a regulatory phenotype in naive T cells. J Immunol 176(11):6752–6761. https://doi.org/10.4049/jimmunol.176.11.6752 Sakaguchi S, Mikami N, Wing JB, Tanaka A, Ichiyama K, Ohkura N (2020) Regulatory T cells and human disease. Annu Rev Immunol 38:541–566. https://doi.org/10.1146/annurev-immunol-042718-041717 Nishikawa H, Sakaguchi S (2014) Regulatory T cells in cancer immunotherapy. Curr Opin Immunol 27:1–7. https://doi.org/10.1016/j.coi.2013.12.005 Fridman WH, Pages F, Sautes-Fridman C, Galon J (2012) The immune contexture in human tumours: impact on clinical outcome. Nat Rev Cancer 12(4):298–306. https://doi.org/10.1038/nrc3245 Miyara M, Yoshioka Y, Kitoh A, Shima T, Wing K, Niwa A, Parizot C, Taflin C, Heike T, Valeyre D, Mathian A, Nakahata T, Yamaguchi T, Nomura T, Ono M, Amoura Z, Gorochov G, Sakaguchi S (2009) Functional delineation and differentiation dynamics of human CD4+ T cells expressing the FoxP3 transcription factor. Immunity 30(6):899–911. https://doi.org/10.1016/j.immuni.2009.03.019 Saito T, Nishikawa H, Wada H, Nagano Y, Sugiyama D, Atarashi K, Maeda Y, Hamaguchi M, Ohkura N, Sato E, Nagase H, Nishimura J, Yamamoto H, Takiguchi S, Tanoue T, Suda W, Morita H, Hattori M, Honda K, Mori M, Doki Y, Sakaguchi S (2016) Two FOXP3(+)CD4(+) T cell subpopulations distinctly control the prognosis of colorectal cancers. Nat Med 22(6):679–684. https://doi.org/10.1038/nm.4086 Ohue Y, Nishikawa H (2019) Regulatory T (Treg) cells in cancer: can Treg cells be a new therapeutic target? Cancer Sci 110(7):2080–2089. https://doi.org/10.1111/cas.14069 Seo N, Hayakawa S, Takigawa M, Tokura Y (2001) Interleukin-10 expressed at early tumour sites induces subsequent generation of CD4(+) T-regulatory cells and systemic collapse of antitumour immunity. Immunology 103(4):449–457. https://doi.org/10.1046/j.1365-2567.2001.01279.x Zarek PE, Huang CT, Lutz ER, Kowalski J, Horton MR, Linden J, Drake CG, Powell JD (2008) A2A receptor signaling promotes peripheral tolerance by inducing T-cell anergy and the generation of adaptive regulatory T cells. Blood 111(1):251–259. https://doi.org/10.1182/blood-2007-03-081646 Curotto de Lafaille MA, Lafaille JJ (2009) Natural and adaptive foxp3+ regulatory T cells: more of the same or a division of labor? Immunity 30(5):626–635. https://doi.org/10.1016/j.immuni.2009.05.002 Zhang Y, Lazarus J, Steele NG, Yan W, Lee HJ, Nwosu ZC, Halbrook CJ, Menjivar RE, Kemp SB, Sirihorachai VR, Velez-Delgado A, Donahue K, Carpenter ES, Brown KL, Irizarry-Negron V, Nevison AC, Vinta A, Anderson MA, Crawford HC, Lyssiotis CA, Frankel TL, Bednar F, Pasca di Magliano M (2020) Regulatory T-cell depletion alters the tumor microenvironment and accelerates pancreatic carcinogenesis. Cancer Discov 10(3):422–439. https://doi.org/10.1158/2159-8290.CD-19-0958 Plitas G, Konopacki C, Wu K, Bos PD, Morrow M, Putintseva EV, Chudakov DM, Rudensky AY (2016) Regulatory t cells exhibit distinct features in human breast cancer. Immunity 45(5):1122–1134. https://doi.org/10.1016/j.immuni.2016.10.032 Toor SM, Murshed K, Al-Dhaheri M, Khawar M, Abu Nada M, Elkord E (2019) Immune checkpoints in circulating and tumor-infiltrating CD4(+) T cell subsets in colorectal cancer patients. Front Immunol 10:2936. https://doi.org/10.3389/fimmu.2019.02936 Sanjabi S, Zenewicz LA, Kamanaka M, Flavell RA (2009) Anti-inflammatory and pro-inflammatory roles of TGF-beta, IL-10, and IL-22 in immunity and autoimmunity. Curr Opin Pharmacol 9(4):447–453. https://doi.org/10.1016/j.coph.2009.04.008 Wrzesinski SH, Wan YY, Flavell RA (2007) Transforming growth factor-beta and the immune response: implications for anticancer therapy. Clin Cancer Res 13(18 Pt 1):5262–5270. https://doi.org/10.1158/1078-0432.CCR-07-1157 Mirlekar B, Michaud D, Searcy R, Greene K, Pylayeva-Gupta Y (2018) IL35 hinders endogenous antitumor T-cell immunity and responsiveness to immunotherapy in pancreatic cancer. Cancer Immunol Res 6(9):1014–1024. https://doi.org/10.1158/2326-6066.CIR-17-0710 Takahashi T, Tagami T, Yamazaki S, Uede T, Shimizu J, Sakaguchi N, Mak TW, Sakaguchi S (2000) Immunologic self-tolerance maintained by CD25(+)CD4(+) regulatory T cells constitutively expressing cytotoxic T lymphocyte-associated antigen 4. J Exp Med 192(2):303–310. https://doi.org/10.1084/jem.192.2.303 Buchbinder EI, Desai A (2016) CTLA-4 and PD-1 pathways: similarities, differences, and implications of their inhibition. Am J Clin Oncol 39(1):98–106. https://doi.org/10.1097/COC.0000000000000239 Huang CT, Workman CJ, Flies D, Pan X, Marson AL, Zhou G, Hipkiss EL, Ravi S, Kowalski J, Levitsky HI, Powell JD, Pardoll DM, Drake CG, Vignali DA (2004) Role of LAG-3 in regulatory T cells. Immunity 21(4):503–513. https://doi.org/10.1016/j.immuni.2004.08.010 Campos-Mora M, Morales RA, Gajardo T, Catalan D, Pino-Lagos K (2013) Neuropilin-1 in transplantation tolerance. Front Immunol 4:405. https://doi.org/10.3389/fimmu.2013.00405 Chaudhary B, Khaled YS, Ammori BJ, Elkord E (2014) Neuropilin 1: function and therapeutic potential in cancer. Cancer Immunol Immunother 63(2):81–99. https://doi.org/10.1007/s00262-013-1500-0 Cao X, Cai SF, Fehniger TA, Song J, Collins LI, Piwnica-Worms DR, Ley TJ (2007) Granzyme B and perforin are important for regulatory T cell-mediated suppression of tumor clearance. Immunity 27(4):635–646. https://doi.org/10.1016/j.immuni.2007.08.014 Facciabene A, Motz GT, Coukos G (2012) T-regulatory cells: key players in tumor immune escape and angiogenesis. Cancer Res 72(9):2162–2171. https://doi.org/10.1158/0008-5472.CAN-11-3687 Katsuno Y, Lamouille S, Derynck R (2013) TGF-beta signaling and epithelial-mesenchymal transition in cancer progression. Curr Opin Oncol 25(1):76–84. https://doi.org/10.1097/CCO.0b013e32835b6371 Nickerson NK, Mill CP, Wu HJ, Riese DJ 2nd, Foley J (2013) Autocrine-derived epidermal growth factor receptor ligands contribute to recruitment of tumor-associated macrophage and growth of basal breast cancer cells in vivo. Oncol Res 20(7):303–317. https://doi.org/10.3727/096504013x13639794277761 Paluskievicz CM, Cao X, Abdi R, Zheng P, Liu Y, Bromberg JS (2019) T regulatory cells and priming the suppressive tumor microenvironment. Front Immunol 10:2453. https://doi.org/10.3389/fimmu.2019.02453 Gupta S, Joshi K, Wig JD, Arora SK (2007) Intratumoral FOXP3 expression in infiltrating breast carcinoma: its association with clinicopathologic parameters and angiogenesis. Acta Oncol 46(6):792–797. https://doi.org/10.1080/02841860701233443 Shimizu J, Yamazaki S, Sakaguchi S (1999) Induction of tumor immunity by removing CD25+CD4+ T cells: a common basis between tumor immunity and autoimmunity. J Immunol 163(10):5211–5218 Shi C, Chen Y, Chen Y, Yang Y, Bing W, Qi J (2019) CD4(+) CD25(+) regulatory T cells promote hepatocellular carcinoma invasion via TGF-beta1-induced epithelial-mesenchymal transition. Onco Targets Ther 12:279–289. https://doi.org/10.2147/OTT.S172417 Angelin A, Gil-de-Gomez L, Dahiya S, Jiao J, Guo L, Levine MH, Wang Z, Quinn WJ, 3rd, Kopinski PK, Wang L, Akimova T, Liu Y, Bhatti TR, Han R, Laskin BL, Baur JA, Blair IA, Wallace DC, Hancock WW, Beier UH (2017) Foxp3 reprograms T cell metabolism to function in low-glucose, high-lactate environments. Cell Metab 25(6):1282–1293 e1287. https://doi.org/10.1016/j.cmet.2016.12.018 Kishore M, Cheung KCP, Fu H, Bonacina F, Wang G, Coe D, Ward EJ, Colamatteo A, Jangani M, Baragetti A, Matarese G, Smith DM, Haas R, Mauro C, Wraith DC, Okkenhaug K, Catapano AL, De Rosa V, Norata GD, Marelli-Berg FM (2017) Regulatory T cell migration is dependent on glucokinase-mediated glycolysis. Immunity 47(5):875–889 e810. https://doi.org/10.1016/j.immuni.2017.10.017 Jordan JT, Sun W, Hussain SF, DeAngulo G, Prabhu SS, Heimberger AB (2008) Preferential migration of regulatory T cells mediated by glioma-secreted chemokines can be blocked with chemotherapy. Cancer Immunol Immunother 57(1):123–131. https://doi.org/10.1007/s00262-007-0336-x Brandacher G, Perathoner A, Ladurner R, Schneeberger S, Obrist P, Winkler C, Werner ER, Werner-Felmayer G, Weiss HG, Gobel G, Margreiter R, Konigsrainer A, Fuchs D, Amberger A (2006) Prognostic value of indoleamine 2,3-dioxygenase expression in colorectal cancer: effect on tumor-infiltrating T cells. Clin Cancer Res 12(4):1144–1151. https://doi.org/10.1158/1078-0432.CCR-05-1966 Ino K, Yamamoto E, Shibata K, Kajiyama H, Yoshida N, Terauchi M, Nawa A, Nagasaka T, Takikawa O, Kikkawa F (2008) Inverse correlation between tumoral indoleamine 2,3-dioxygenase expression and tumor-infiltrating lymphocytes in endometrial cancer: its association with disease progression and survival. Clin Cancer Res 14(8):2310–2317. https://doi.org/10.1158/1078-0432.CCR-07-4144 Nakamura T, Shima T, Saeki A, Hidaka T, Nakashima A, Takikawa O, Saito S (2007) Expression of indoleamine 2, 3-dioxygenase and the recruitment of Foxp3-expressing regulatory T cells in the development and progression of uterine cervical cancer. Cancer Sci 98(6):874–881. https://doi.org/10.1111/j.1349-7006.2007.00470.x Folgiero V, Miele E, Carai A, Ferretti E, Alfano V, Po A, Bertaina V, Goffredo BM, Benedetti MC, Camassei FD, Cacchione A, Locatelli F, Mastronuzzi A (2016) IDO1 involvement in mTOR pathway: a molecular mechanism of resistance to mTOR targeting in medulloblastoma. Oncotarget 7(33):52900–52911. https://doi.org/10.18632/oncotarget.9284 Pacella I, Procaccini C, Focaccetti C, Miacci S, Timperi E, Faicchia D, Severa M, Rizzo F, Coccia EM, Bonacina F, Mitro N, Norata GD, Rossetti G, Ranzani V, Pagani M, Giorda E, Wei Y, Matarese G, Barnaba V, Piconese S (2018) Fatty acid metabolism complements glycolysis in the selective regulatory T cell expansion during tumor growth. Proc Natl Acad Sci U S A 115(28):E6546-e6555. https://doi.org/10.1073/pnas.1720113115 Li L, Liu X, Sanders KL, Edwards JL, Ye J, Si F, Gao A, Huang L, Hsueh EC, Ford DA, Hoft DF, Peng G (2019) TLR8-mediated metabolic control of human treg function: a mechanistic target for cancer immunotherapy. Cell Metab 29(1):103–123 e105. https://doi.org/10.1016/j.cmet.2018.09.020 Sun IH, Oh MH, Zhao L, Patel CH, Arwood ML, Xu W, Tam AJ, Blosser RL, Wen J, Powell JD (2018) mTOR complex 1 signaling regulates the generation and function of central and effector Foxp3(+) regulatory T Cells. J Immunol 201(2):481–492. https://doi.org/10.4049/jimmunol.1701477 Lowe MM, Boothby I, Clancy S, Ahn RS, Liao W, Nguyen DN, Schumann K, Marson A, Mahuron KM, Kingsbury GA, Liu Z, Munoz Sandoval P, Rodriguez RS, Pauli ML, Taravati K, Arron ST, Neuhaus IM, Harris HW, Kim EA, Shin US, Krummel MF, Daud A, Scharschmidt TC, Rosenblum MD (2019) Regulatory T cells use arginase 2 to enhance their metabolic fitness in tissues. JCI Insight. https://doi.org/10.1172/jci.insight.129756 Maj T, Wang W, Crespo J, Zhang H, Wang W, Wei S, Zhao L, Vatan L, Shao I, Szeliga W, Lyssiotis C, Liu JR, Kryczek I, Zou W (2017) Oxidative stress controls regulatory T cell apoptosis and suppressor activity and PD-L1-blockade resistance in tumor. Nat Immunol 18(12):1332–1341. https://doi.org/10.1038/ni.3868 Field CS, Baixauli F, Kyle RL, Puleston DJ, Cameron AM, Sanin DE, Hippen KL, Loschi M, Thangavelu G, Corrado M, Edwards-Hicks J, Grzes KM, Pearce EJ, Blazar BR, Pearce EL (2020) Mitochondrial integrity regulated by lipid metabolism is a cell-intrinsic checkpoint for treg suppressive function. Cell Metab 31(2):422–437 e425. https://doi.org/10.1016/j.cmet.2019.11.021 Weinberg SE, Singer BD, Steinert EM, Martinez CA, Mehta MM, Martinez-Reyes I, Gao P, Helmin KA, Abdala-Valencia H, Sena LA, Schumacker PT, Turka LA, Chandel NS (2019) Mitochondrial complex III is essential for suppressive function of regulatory T cells. Nature 565(7740):495–499. https://doi.org/10.1038/s41586-018-0846-z Chang WH, Lai AG (2019) The pan-cancer mutational landscape of the PPAR pathway reveals universal patterns of dysregulated metabolism and interactions with tumor immunity and hypoxia. Ann N Y Acad Sci 1448(1):65–82. https://doi.org/10.1111/nyas.14170 Muroski ME, Miska J, Chang AL, Zhang P, Rashidi A, Moore H, Lopez-Rosas A, Han Y, Lesniak MS (2017) Fatty acid uptake in T cell subsets using a quantum dot fatty acid conjugate. Sci Rep 7(1):5790. https://doi.org/10.1038/s41598-017-05556-x Delgoffe GM, Woo SR, Turnis ME, Gravano DM, Guy C, Overacre AE, Bettini ML, Vogel P, Finkelstein D, Bonnevier J, Workman CJ, Vignali DA (2013) Stability and function of regulatory T cells is maintained by a neuropilin-1-semaphorin-4a axis. Nature 501(7466):252–256. https://doi.org/10.1038/nature12428 Magnuson AM, Kiner E, Ergun A, Park JS, Asinovski N, Ortiz-Lopez A, Kilcoyne A, Paoluzzi-Tomada E, Weissleder R, Mathis D, Benoist C (2018) Identification and validation of a tumor-infiltrating Treg transcriptional signature conserved across species and tumor types. Proc Natl Acad Sci U S A 115(45):E10672–E10681. https://doi.org/10.1073/pnas.1810580115 Chapman NM, Zeng H, Nguyen TM, Wang Y, Vogel P, Dhungana Y, Liu X, Neale G, Locasale JW, Chi H (2018) mTOR coordinates transcriptional programs and mitochondrial metabolism of activated Treg subsets to protect tissue homeostasis. Nat Commun 9(1):2095. https://doi.org/10.1038/s41467-018-04392-5 Donninelli G, Del Corno M, Pierdominici M, Scazzocchio B, Vari R, Varano B, Pacella I, Piconese S, Barnaba V, D’Archivio M, Masella R, Conti L, Gessani S (2017) Distinct blood and visceral adipose tissue regulatory T cell and innate lymphocyte profiles characterize obesity and colorectal cancer. Front Immunol 8:643. https://doi.org/10.3389/fimmu.2017.00643 Raychaudhuri D, Bhattacharya R, Sinha BP, Liu CSC, Ghosh AR, Rahaman O, Bandopadhyay P, Sarif J, D’Rozario R, Paul S, Das A, Sarkar DK, Chattopadhyay S, Ganguly D (2019) Lactate induces pro-tumor reprogramming in intratumoral plasmacytoid dendritic cells. Front Immunol 10:1878. https://doi.org/10.3389/fimmu.2019.01878 Kryczek I, Wu K, Zhao E, Wei S, Vatan L, Szeliga W, Huang E, Greenson J, Chang A, Rolinski J, Radwan P, Fang J, Wang G, Zou W (2011) IL-17+ regulatory T cells in the microenvironments of chronic inflammation and cancer. J Immunol 186(7):4388–4395. https://doi.org/10.4049/jimmunol.1003251 Rizzo A, Di Giovangiulio M, Stolfi C, Franze E, Fehling HJ, Carsetti R, Giorda E, Colantoni A, Ortenzi A, Rugge M, Mescoli C, Monteleone G, Fantini MC (2018) RORgammat-expressing tregs drive the growth of colitis-associated colorectal cancer by controlling IL6 in dendritic cells. Cancer Immunol Res 6(9):1082–1092. https://doi.org/10.1158/2326-6066.CIR-17-0698 Jetten AM, Takeda Y, Slominski A, Kang HS (2018) Retinoic acid-related orphan receptor gamma (RORgamma): connecting sterol metabolism to regulation of the immune system and autoimmune disease. Curr Opin Toxicol 8:66–80. https://doi.org/10.1016/j.cotox.2018.01.005 Pan Y, Tian T, Park CO, Lofftus SY, Mei S, Liu X, Luo C, O’Malley JT, Gehad A, Teague JE, Divito SJ, Fuhlbrigge R, Puigserver P, Krueger JG, Hotamisligil GS, Clark RA, Kupper TS (2017) Survival of tissue-resident memory T cells requires exogenous lipid uptake and metabolism. Nature 543(7644):252–256. https://doi.org/10.1038/nature21379 Kabelitz D, Wesch D, He W (2007) Perspectives of gammadelta T cells in tumor immunology. Cancer Res 67(1):5–8. https://doi.org/10.1158/0008-5472.CAN-06-3069 Peng G, Wang HY, Peng W, Kiniwa Y, Seo KH, Wang RF (2007) Tumor-infiltrating gammadelta T cells suppress T and dendritic cell function via mechanisms controlled by a unique toll-like receptor signaling pathway. Immunity 27(2):334–348. https://doi.org/10.1016/j.immuni.2007.05.020 Wesch D, Peters C, Siegers GM (2014) Human gamma delta T regulatory cells in cancer: fact or fiction? Front Immunol 5:598. https://doi.org/10.3389/fimmu.2014.00598 Kang N, Tang L, Li X, Wu D, Li W, Chen X, Cui L, Ba D, He W (2009) Identification and characterization of Foxp3(+) gammadelta T cells in mouse and human. Immunol Lett 125(2):105–113. https://doi.org/10.1016/j.imlet.2009.06.005 Ma C, Zhang Q, Ye J, Wang F, Zhang Y, Wevers E, Schwartz T, Hunborg P, Varvares MA, Hoft DF, Hsueh EC, Peng G (2012) Tumor-infiltrating gammadelta T lymphocytes predict clinical outcome in human breast cancer. J Immunol 189(10):5029–5036. https://doi.org/10.4049/jimmunol.1201892 Gober HJ, Kistowska M, Angman L, Jeno P, Mori L, De Libero G (2003) Human T cell receptor gammadelta cells recognize endogenous mevalonate metabolites in tumor cells. J Exp Med 197(2):163–168. https://doi.org/10.1084/jem.20021500 Raverdeau M, Cunningham SP, Harmon C, Lynch L (2019) gammadelta T cells in cancer: a small population of lymphocytes with big implications. Clin Transl Immunol 8(10):e01080. https://doi.org/10.1002/cti2.1080 Wang H, Henry O, Distefano MD, Wang YC, Raikkonen J, Monkkonen J, Tanaka Y, Morita CT (2013) Butyrophilin 3A1 plays an essential role in prenyl pyrophosphate stimulation of human Vgamma2Vdelta2 T cells. J Immunol 191(3):1029–1042. https://doi.org/10.4049/jimmunol.1300658 Casetti R, Agrati C, Wallace M, Sacchi A, Martini F, Martino A, Rinaldi A, Malkovsky M (2009) Cutting edge: TGF-beta1 and IL-15 Induce FOXP3+ gammadelta regulatory T cells in the presence of antigen stimulation. J Immunol 183(6):3574–3577. https://doi.org/10.4049/jimmunol.0901334 Schreiber TH, Wolf D, Bodero M, Podack E (2012) Tumor antigen specific iTreg accumulate in the tumor microenvironment and suppress therapeutic vaccination. Oncoimmunology 1(5):642–648. https://doi.org/10.4161/onci.20298 Zhou G, Drake CG, Levitsky HI (2006) Amplification of tumor-specific regulatory T cells following therapeutic cancer vaccines. Blood 107(2):628–636. https://doi.org/10.1182/blood-2005-07-2737 Clambey ET, McNamee EN, Westrich JA, Glover LE, Campbell EL, Jedlicka P, de Zoeten EF, Cambier JC, Stenmark KR, Colgan SP, Eltzschig HK (2012) Hypoxia-inducible factor-1 alpha-dependent induction of FoxP3 drives regulatory T-cell abundance and function during inflammatory hypoxia of the mucosa. Proc Natl Acad Sci U S A 109(41):E2784-2793. https://doi.org/10.1073/pnas.1202366109 Fong GH, Takeda K (2008) Role and regulation of prolyl hydroxylase domain proteins. Cell Death Differ 15(4):635–641. https://doi.org/10.1038/cdd.2008.10 Deng B, Zhu JM, Wang Y, Liu TT, Ding YB, **ao WM, Lu GT, Bo P, Shen XZ (2013) Intratumor hypoxia promotes immune tolerance by inducing regulatory T cells via TGF-beta1 in gastric cancer. PLoS ONE 8(5):e63777. https://doi.org/10.1371/journal.pone.0063777 Chen J, Jiang CC, ** L, Zhang XD (2016) Regulation of PD-L1: a novel role of pro-survival signalling in cancer. Ann Oncol 27(3):409–416. https://doi.org/10.1093/annonc/mdv615 Ruf M, Moch H, Schraml P (2016) PD-L1 expression is regulated by hypoxia inducible factor in clear cell renal cell carcinoma. Int J Cancer 139(2):396–403. https://doi.org/10.1002/ijc.30077 Szajnik M, Czystowska M, Szczepanski MJ, Mandapathil M, Whiteside TL (2010) Tumor-derived microvesicles induce, expand and up-regulate biological activities of human regulatory T cells (Treg). PLoS ONE 5(7):e11469. https://doi.org/10.1371/journal.pone.0011469 Yin Y, Cai X, Chen X, Liang H, Zhang Y, Li J, Wang Z, Chen X, Zhang W, Yokoyama S, Wang C, Li L, Li L, Hou D, Dong L, Xu T, Hiroi T, Yang F, Ji H, Zhang J, Zen K, Zhang CY (2014) Tumor-secreted miR-214 induces regulatory T cells: a major link between immune evasion and tumor growth. Cell Res 24(10):1164–1180. https://doi.org/10.1038/cr.2014.121 Brennan P, Babbage JW, Burgering BM, Groner B, Reif K, Cantrell DA (1997) Phosphatidylinositol 3-kinase couples the interleukin-2 receptor to the cell cycle regulator E2F. Immunity 7(5):679–689. https://doi.org/10.1016/s1074-7613(00)80388-x Huynh A, DuPage M, Priyadharshini B, Sage PT, Quiros J, Borges CM, Townamchai N, Gerriets VA, Rathmell JC, Sharpe AH, Bluestone JA, Turka LA (2015) Control of PI(3) kinase in Treg cells maintains homeostasis and lineage stability. Nat Immunol 16(2):188–196. https://doi.org/10.1038/ni.3077 Haxhinasto S, Mathis D, Benoist C (2008) The AKT-mTOR axis regulates de novo differentiation of CD4+Foxp3+ cells. J Exp Med 205(3):565–574. https://doi.org/10.1084/jem.20071477 Shi LZ, Wang R, Huang G, Vogel P, Neale G, Green DR, Chi H (2011) HIF1alpha-dependent glycolytic pathway orchestrates a metabolic checkpoint for the differentiation of TH17 and Treg cells. J Exp Med 208(7):1367–1376. https://doi.org/10.1084/jem.20110278 Berod L, Friedrich C, Nandan A, Freitag J, Hagemann S, Harmrolfs K, Sandouk A, Hesse C, Castro CN, Bahre H, Tschirner SK, Gorinski N, Gohmert M, Mayer CT, Huehn J, Ponimaskin E, Abraham WR, Muller R, Lochner M, Sparwasser T (2014) De novo fatty acid synthesis controls the fate between regulatory T and T helper 17 cells. Nat Med 20(11):1327–1333. https://doi.org/10.1038/nm.3704 Svensson RU, Parker SJ, Eichner LJ, Kolar MJ, Wallace M, Brun SN, Lombardo PS, Van Nostrand JL, Hutchins A, Vera L, Gerken L, Greenwood J, Bhat S, Harriman G, Westlin WF, Harwood HJ Jr, Saghatelian A, Kapeller R, Metallo CM, Shaw RJ (2016) Inhibition of acetyl-CoA carboxylase suppresses fatty acid synthesis and tumor growth of non-small-cell lung cancer in preclinical models. Nat Med 22(10):1108–1119. https://doi.org/10.1038/nm.4181 Gerriets VA, Kishton RJ, Johnson MO, Cohen S, Siska PJ, Nichols AG, Warmoes MO, de Cubas AA, MacIver NJ, Locasale JW, Turka LA, Wells AD, Rathmell JC (2016) Foxp3 and Toll-like receptor signaling balance Treg cell anabolic metabolism for suppression. Nat Immunol 17(12):1459–1466. https://doi.org/10.1038/ni.3577 Procaccini C, De Rosa V, Galgani M, Abanni L, Cali G, Porcellini A, Carbone F, Fontana S, Horvath TL, La Cava A, Matarese G (2010) An oscillatory switch in mTOR kinase activity sets regulatory T cell responsiveness. Immunity 33(6):929–941. https://doi.org/10.1016/j.immuni.2010.11.024 Hosomi K, Kunisawa J (2017) The specific roles of vitamins in the regulation of immunosurveillance and maintenance of immunologic homeostasis in the gut. Immune Netw 17(1):13–19. https://doi.org/10.4110/in.2017.17.1.13 Lu L, Lan Q, Li Z, Zhou X, Gu J, Li Q, Wang J, Chen M, Liu Y, Shen Y, Brand DD, Ryffel B, Horwitz DA, Quismorio FP, Liu Z, Li B, Olsen NJ, Zheng SG (2014) Critical role of all-trans retinoic acid in stabilizing human natural regulatory T cells under inflammatory conditions. Proc Natl Acad Sci U S A 111(33):E3432-3440. https://doi.org/10.1073/pnas.1408780111 Lu L, Ma J, Li Z, Lan Q, Chen M, Liu Y, **a Z, Wang J, Han Y, Shi W, Quesniaux V, Ryffel B, Brand D, Li B, Liu Z, Zheng SG (2011) All-trans retinoic acid promotes TGF-β-induced Tregs via histone modification but not DNA demethylation on Foxp3 gene locus. PLoS ONE 6(9):e24590. https://doi.org/10.1371/journal.pone.0024590 Mucida D, Park Y, Kim G, Turovskaya O, Scott I, Kronenberg M, Cheroutre H (2007) Reciprocal TH17 and regulatory T cell differentiation mediated by retinoic acid. Sci NY 317(5835):256–260. https://doi.org/10.1126/science.1145697 Zheng SG, Wang J, Wang P, Gray JD, Horwitz DA (2007) IL-2 is essential for TGF-beta to convert naive CD4+CD25- cells to CD25+Foxp3+ regulatory T cells and for expansion of these cells. J Immunol 178(4):2018–2027. https://doi.org/10.4049/jimmunol.178.4.2018 Hill JA, Hall JA, Sun CM, Cai Q, Ghyselinck N, Chambon P, Belkaid Y, Mathis D, Benoist C (2008) Retinoic acid enhances Foxp3 induction indirectly by relieving inhibition from CD4+CD44hi Cells. Immunity 29(5):758–770. https://doi.org/10.1016/j.immuni.2008.09.018 Yue X, Trifari S, Äijö T, Tsagaratou A, Pastor WA, Zepeda-Martínez JA, Lio CW, Li X, Huang Y, Vijayanand P, Lähdesmäki H, Rao A (2016) Control of Foxp3 stability through modulation of TET activity. J Exp Med 213(3):377–397. https://doi.org/10.1084/jem.20151438 Sasidharan Nair V, Song MH, Oh KI (2016) Vitamin C facilitates demethylation of the Foxp3 enhancer in a Tet-dependent manner. J Immunol 196(5):2119–2131. https://doi.org/10.4049/jimmunol.1502352 Rasmussen KD, Helin K (2016) Role of TET enzymes in DNA methylation, development, and cancer. Genes Dev 30(7):733–750. https://doi.org/10.1101/gad.276568.115 Yue X, Lio CJ, Samaniego-Castruita D, Li X, Rao A (2019) Loss of TET2 and TET3 in regulatory T cells unleashes effector function. Nat Commun 10(1):2011. https://doi.org/10.1038/s41467-019-09541-y Nikolouli E, Hardtke-Wolenski M, Hapke M, Beckstette M, Geffers R, Floess S, Jaeckel E, Huehn J (2017) Alloantigen-induced regulatory T cells generated in presence of vitamin C display enhanced stability of Foxp3 expression and promote skin allograft acceptance. Front Immunol 8:748. https://doi.org/10.3389/fimmu.2017.00748 Jeffery LE, Burke F, Mura M, Zheng Y, Qureshi OS, Hewison M, Walker LS, Lammas DA, Raza K, Sansom DM (2009) 1,25-Dihydroxyvitamin D3 and IL-2 combine to inhibit T cell production of inflammatory cytokines and promote development of regulatory T cells expressing CTLA-4 and FoxP3. J Immunol 183(9):5458–5467. https://doi.org/10.4049/jimmunol.0803217 Joshi S, Pantalena LC, Liu XK, Gaffen SL, Liu H, Rohowsky-Kochan C, Ichiyama K, Yoshimura A, Steinman L, Christakos S, Youssef S (2011) 1,25-dihydroxyvitamin D(3) ameliorates Th17 autoimmunity via transcriptional modulation of interleukin-17A. Mol Cell Biol 31(17):3653–3669. https://doi.org/10.1128/mcb.05020-11 Kang SW, Kim SH, Lee N, Lee WW, Hwang KA, Shin MS, Lee SH, Kim WU, Kang I (2012) 1,25-Dihyroxyvitamin D3 promotes FOXP3 expression via binding to vitamin D response elements in its conserved noncoding sequence region. J Immunol 188(11):5276–5282. https://doi.org/10.4049/jimmunol.1101211 Fisher SA, Rahimzadeh M, Brierley C, Gration B, Doree C, Kimber CE, Plaza Cajide A, Lamikanra AA, Roberts DJ (2019) The role of vitamin D in increasing circulating T regulatory cell numbers and modulating T regulatory cell phenotypes in patients with inflammatory disease or in healthy volunteers: a systematic review. PLoS ONE 14(9):e0222313. https://doi.org/10.1371/journal.pone.0222313 Singh N, Gurav A, Sivaprakasam S, Brady E, Padia R, Shi H, Thangaraju M, Prasad PD, Manicassamy S, Munn DH, Lee JR, Offermanns S, Ganapathy V (2014) Activation of Gpr109a, receptor for niacin and the commensal metabolite butyrate, suppresses colonic inflammation and carcinogenesis. Immunity 40(1):128–139. https://doi.org/10.1016/j.immuni.2013.12.007 Hegyi J, Schwartz RA, Hegyi V (2004) Pellagra: dermatitis, dementia, and diarrhea. Int J Dermatol 43(1):1–5. https://doi.org/10.1111/j.1365-4632.2004.01959.x Moretti S, Menicali E, Voce P, Morelli S, Cantarelli S, Sponziello M, Colella R, Fallarino F, Orabona C, Alunno A, de Biase D, Bini V, Mameli MG, Filetti S, Gerli R, Macchiarulo A, Melillo RM, Tallini G, Santoro M, Puccetti P, Avenia N, Puxeddu E (2014) Indoleamine 2,3-dioxygenase 1 (IDO1) is up-regulated in thyroid carcinoma and drives the development of an immunosuppressant tumor microenvironment. J Clin Endocrinol Metabol 99(5):E832-840. https://doi.org/10.1210/jc.2013-3351 Baban B, Chandler PR, Sharma MD, Pihkala J, Koni PA, Munn DH, Mellor AL (2009) IDO activates regulatory T cells and blocks their conversion into Th17-like T cells. J Immunol 183(4):2475–2483. https://doi.org/10.4049/jimmunol.0900986 Sharma MD, Hou DY, Liu Y, Koni PA, Metz R, Chandler P, Mellor AL, He Y, Munn DH (2009) Indoleamine 2,3-dioxygenase controls conversion of Foxp3+ Tregs to TH17-like cells in tumor-draining lymph nodes. Blood 113(24):6102–6111. https://doi.org/10.1182/blood-2008-12-195354 Sharma MD, Baban B, Chandler P, Hou DY, Singh N, Yagita H, Azuma M, Blazar BR, Mellor AL, Munn DH (2007) Plasmacytoid dendritic cells from mouse tumor-draining lymph nodes directly activate mature Tregs via indoleamine 2,3-dioxygenase. J Clin Invest 117(9):2570–2582. https://doi.org/10.1172/jci31911 Opitz CA, Litzenburger UM, Sahm F, Ott M, Tritschler I, Trump S, Schumacher T, Jestaedt L, Schrenk D, Weller M, Jugold M, Guillemin GJ, Miller CL, Lutz C, Radlwimmer B, Lehmann I, von Deimling A, Wick W, Platten M (2011) An endogenous tumour-promoting ligand of the human aryl hydrocarbon receptor. Nature 478(7368):197–203. https://doi.org/10.1038/nature10491 Nguyen NT, Kimura A, Nakahama T, Chinen I, Masuda K, Nohara K, Fujii-Kuriyama Y, Kishimoto T (2010) Aryl hydrocarbon receptor negatively regulates dendritic cell immunogenicity via a kynurenine-dependent mechanism. Proc Natl Acad Sci U S A 107(46):19961–19966. https://doi.org/10.1073/pnas.1014465107 Munn DH, Sharma MD, Baban B, Harding HP, Zhang Y, Ron D, Mellor AL (2005) GCN2 kinase in T cells mediates proliferative arrest and anergy induction in response to indoleamine 2,3-dioxygenase. Immunity 22(5):633–642. https://doi.org/10.1016/j.immuni.2005.03.013 Sharma MD, Shinde R, McGaha TL, Huang L, Holmgaard RB, Wolchok JD, Mautino MR, Celis E, Sharpe AH, Francisco LM, Powell JD, Yagita H, Mellor AL, Blazar BR, Munn DH (2015) The PTEN pathway in Tregs is a critical driver of the suppressive tumor microenvironment. Sci Adv 1(10):e1500845. https://doi.org/10.1126/sciadv.1500845 Schenk U, Frascoli M, Proietti M, Geffers R, Traggiai E, Buer J, Ricordi C, Westendorf AM, Grassi F (2011) ATP inhibits the generation and function of regulatory T cells through the activation of purinergic P2X receptors. Sci Signal 4(162):ra12. https://doi.org/10.1126/scisignal.2001270 Borsellino G, Kleinewietfeld M, Di Mitri D, Sternjak A, Diamantini A, Giometto R, Höpner S, Centonze D, Bernardi G, Dell’Acqua ML, Rossini PM, Battistini L, Rötzschke O, Falk K (2007) Expression of ectonucleotidase CD39 by Foxp3+ Treg cells: hydrolysis of extracellular ATP and immune suppression. Blood 110(4):1225–1232. https://doi.org/10.1182/blood-2006-12-064527 Saleh R, Elkord E (2020) FoxP3(+) T regulatory cells in cancer: Prognostic biomarkers and therapeutic targets. Cancer Lett 490:174–185. https://doi.org/10.1016/j.canlet.2020.07.022 Deaglio S, Dwyer KM, Gao W, Friedman D, Usheva A, Erat A, Chen JF, Enjyoji K, Linden J, Oukka M, Kuchroo VK, Strom TB, Robson SC (2007) Adenosine generation catalyzed by CD39 and CD73 expressed on regulatory T cells mediates immune suppression. J Exp Med 204(6):1257–1265. https://doi.org/10.1084/jem.20062512 Saleh R, Elkord E (2019) Treg-mediated acquired resistance to immune checkpoint inhibitors. Cancer Lett 457:168–179. https://doi.org/10.1016/j.canlet.2019.05.003 Li JY, Duan XF, Wang LP, Xu YJ, Huang L, Zhang TF, Liu JY, Li F, Zhang Z, Yue DL, Wang F, Zhang B, Zhang Y (2014) Selective depletion of regulatory T cell subsets by docetaxel treatment in patients with nonsmall cell lung cancer. J Immunol Res 2014:286170. https://doi.org/10.1155/2014/286170 Lissoni P, Brivio F, Fumagalli L, Messina G, Meregalli S, Porro G, Rovelli F, Vigorè L, Tisi E, D’Amico G (2009) Effects of the conventional antitumor therapies surgery, chemotherapy, radiotherapy and immunotherapy on regulatory T lymphocytes in cancer patients. Anticancer Res 29(5):1847–1852 Verma A, Mathur R, Farooque A, Kaul V, Gupta S, Dwarakanath BS (2019) T-regulatory cells in tumor progression and therapy. Cancer Manag Res 11:10731–10747. https://doi.org/10.2147/CMAR.S228887 Cao M, Cabrera R, Xu Y, Liu C, Nelson D (2009) Gamma irradiation alters the phenotype and function of CD4+CD25+ regulatory T cells. Cell Biol Int 33(5):565–571. https://doi.org/10.1016/j.cellbi.2009.02.007 Greten TF, Ormandy LA, Fikuart A, Höchst B, Henschen S, Hörning M, Manns MP, Korangy F (2010) Low-dose cyclophosphamide treatment impairs regulatory T cells and unmasks AFP-specific CD4+ T-cell responses in patients with advanced HCC. J Immunother (Hagerstown, Md : 1997) 33(2):211–218. https://doi.org/10.1097/CJI.0b013e3181bb499f Generali D, Bates G, Berruti A, Brizzi MP, Campo L, Bonardi S, Bersiga A, Allevi G, Milani M, Aguggini S, Dogliotti L, Banham AH, Harris AL, Bottini A, Fox SB (2009) Immunomodulation of FOXP3+ regulatory T cells by the aromatase inhibitor letrozole in breast cancer patients. Clin Cancer Res 15(3):1046–1051. https://doi.org/10.1158/1078-0432.ccr-08-1507 Kareva I (2019) Metabolism and gut microbiota in cancer immunoediting, CD8/Treg ratios, immune cell homeostasis, and cancer (immuno)therapy: concise review. Stem Cells 37(10):1273–1280. https://doi.org/10.1002/stem.3051 Patel MA, Kim JE, Theodros D, Tam A, Velarde E, Kochel CM, Francica B, Nirschl TR, Ghasemzadeh A, Mathios D, Harris-Bookman S, Jackson CC, Jackson C, Ye X, Tran PT, Tyler B, Coric V, Selby M, Brem H, Drake CG, Pardoll DM, Lim M (2016) Agonist anti-GITR monoclonal antibody and stereotactic radiation induce immune-mediated survival advantage in murine intracranial glioma. J Immunother Cancer 4:28. https://doi.org/10.1186/s40425-016-0132-2 Muroyama Y, Nirschl TR, Kochel CM, Lopez-Bujanda Z, Theodros D, Mao W, Carrera-Haro MA, Ghasemzadeh A, Marciscano AE, Velarde E, Tam AJ, Thoburn CJ, Uddin M, Meeker AK, Anders RA, Pardoll DM, Drake CG (2017) Stereotactic radiotherapy increases functionally suppressive regulatory T cells in the tumor microenvironment. Cancer Immunol Res 5(11):992–1004. https://doi.org/10.1158/2326-6066.cir-17-0040 Schuler PJ, Harasymczuk M, Schilling B, Saze Z, Strauss L, Lang S, Johnson JT, Whiteside TL (2013) Effects of adjuvant chemoradiotherapy on the frequency and function of regulatory T cells in patients with head and neck cancer. Clin Cancer Res 19(23):6585–6596. https://doi.org/10.1158/1078-0432.CCR-13-0900 Oweida A, Darragh L, Bhatia S, Raben D, Heasley L, Nemenoff R, Clambey E, Karam S (2019) Regulatory T cells mediate resistance to radiotherapy in head and neck squamous cell carcinoma. J Clin Oncol 37(8_suppl):70–70. https://doi.org/10.1200/JCO.2019.37.8_suppl.70 Crellin NK, Garcia RV, Levings MK (2007) Altered activation of AKT is required for the suppressive function of human CD4+CD25+ T regulatory cells. Blood 109(5):2014–2022. https://doi.org/10.1182/blood-2006-07-035279 Sauer S, Bruno L, Hertweck A, Finlay D, Leleu M, Spivakov M, Knight ZA, Cobb BS, Cantrell D, O’Connor E, Shokat KM, Fisher AG, Merkenschlager M (2008) T cell receptor signaling controls Foxp3 expression via PI3K, Akt, and mTOR. Proc Natl Acad Sci U S A 105(22):7797–7802. https://doi.org/10.1073/pnas.0800928105 Zeng H, Yang K, Cloer C, Neale G, Vogel P, Chi H (2013) mTORC1 couples immune signals and metabolic programming to establish T(reg)-cell function. Nature 499(7459):485–490. https://doi.org/10.1038/nature12297 Kanamori M, Nakatsukasa H, Ito M, Chikuma S, Yoshimura A (2018) Reprogramming of Th1 cells into regulatory T cells through rewiring of the metabolic status. Int Immunol 30(8):357–373. https://doi.org/10.1093/intimm/dxy043 Basu S, Hubbard B, Shevach EM (2015) Foxp3-mediated inhibition of Akt inhibits Glut1 (glucose transporter 1) expression in human T regulatory cells. J Leukoc Biol 97(2):279–283. https://doi.org/10.1189/jlb.2AB0514-273RR Shrestha S, Yang K, Guy C, Vogel P, Neale G, Chi H (2015) Treg cells require the phosphatase PTEN to restrain TH1 and TFH cell responses. Nat Immunol 16(2):178–187. https://doi.org/10.1038/ni.3076 Francisco LM, Salinas VH, Brown KE, Vanguri VK, Freeman GJ, Kuchroo VK, Sharpe AH (2009) PD-L1 regulates the development, maintenance, and function of induced regulatory T cells. J Exp Med 206(13):3015–3029. https://doi.org/10.1084/jem.20090847 Patsoukis N, Brown J, Petkova V, Liu F, Li L, Boussiotis VA (2012) Selective effects of PD-1 on Akt and Ras pathways regulate molecular components of the cell cycle and inhibit T cell proliferation. Sci Signal 5(230):ra46. https://doi.org/10.1126/scisignal.2002796 Gottschalk RA, Corse E, Allison JP (2010) TCR ligand density and affinity determine peripheral induction of Foxp3 in vivo. J Exp Med 207(8):1701–1711. https://doi.org/10.1084/jem.20091999 Li MO, Rudensky AY (2016) T cell receptor signalling in the control of regulatory T cell differentiation and function. Nat Rev Immunol 16(4):220–233. https://doi.org/10.1038/nri.2016.26 O’Connor RS, Guo L, Ghassemi S, Snyder NW, Worth AJ, Weng L, Kam Y, Philipson B, Trefely S, Nunez-Cruz S, Blair IA, June CH, Milone MC (2018) The CPT1a inhibitor, etomoxir induces severe oxidative stress at commonly used concentrations. Sci Rep 8(1):6289. https://doi.org/10.1038/s41598-018-24676-6 Michalek RD, Gerriets VA, Nichols AG, Inoue M, Kazmin D, Chang CY, Dwyer MA, Nelson ER, Pollizzi KN, Ilkayeva O, Giguere V, Zuercher WJ, Powell JD, Shinohara ML, McDonnell DP, Rathmell JC (2011) Estrogen-related receptor-α is a metabolic regulator of effector T-cell activation and differentiation. Proc Natl Acad Sci U S A 108(45):18348–18353. https://doi.org/10.1073/pnas.1108856108 Dang EV, Barbi J, Yang HY, **asena D, Yu H, Zheng Y, Bordman Z, Fu J, Kim Y, Yen HR, Luo W, Zeller K, Shimoda L, Topalian SL, Semenza GL, Dang CV, Pardoll DM, Pan F (2011) Control of T(H)17/T(reg) balance by hypoxia-inducible factor 1. Cell 146(5):772–784. https://doi.org/10.1016/j.cell.2011.07.033 Feldhoff LM, Rueda CM, Moreno-Fernandez ME, Sauer J, Jackson CM, Chougnet CA, Rupp J (2017) IL-1β induced HIF-1α inhibits the differentiation of human FOXP3(+) T cells. Sci Rep 7(1):465. https://doi.org/10.1038/s41598-017-00508-x Clever D, Roychoudhuri R, Constantinides MG, Askenase MH, Sukumar M, Klebanoff CA, Eil RL, Hickman HD, Yu Z, Pan JH, Palmer DC, Phan AT, Goulding J, Gattinoni L, Goldrath AW, Belkaid Y, Restifo NP (2016) Oxygen sensing by T cells establishes an immunologically tolerant metastatic niche. Cell 166(5):1117-1131.e1114. https://doi.org/10.1016/j.cell.2016.07.032 Lee JH, Elly C, Park Y, Liu YC (2015) E3 ubiquitin ligase VHL regulates hypoxia-inducible factor-1α to maintain regulatory T Cell stability and suppressive capacity. Immunity 42(6):1062–1074. https://doi.org/10.1016/j.immuni.2015.05.016 Overacre-Delgoffe AE, Chikina M, Dadey RE, Yano H, Brunazzi EA, Shayan G, Horne W, Moskovitz JM, Kolls JK, Sander C, Shuai Y, Normolle DP, Kirkwood JM, Ferris RL, Delgoffe GM, Bruno TC, Workman CJ, Vignali DAA (2017) Interferon-γ drives T(reg) fragility to promote anti-tumor immunity. Cell 169(6):1130-1141.e1111. https://doi.org/10.1016/j.cell.2017.05.005 He N, Fan W, Henriquez B, Yu RT, Atkins AR, Liddle C, Zheng Y, Downes M, Evans RM (2017) Metabolic control of regulatory T cell (Treg) survival and function by Lkb1. Proc Natl Acad Sci U S A 114(47):12542–12547. https://doi.org/10.1073/pnas.1715363114 Rotin D, Robinson B, Tannock IF (1986) Influence of hypoxia and an acidic environment on the metabolism and viability of cultured cells: potential implications for cell death in tumors. Cancer Res 46(6):2821–2826 Spill F, Reynolds DS, Kamm RD, Zaman MH (2016) Impact of the physical microenvironment on tumor progression and metastasis. Curr Opin Biotechnol 40:41–48. https://doi.org/10.1016/j.copbio.2016.02.007 Chaudhuri O, Koshy ST, Branco da Cunha C, Shin JW, Verbeke CS, Allison KH, Mooney DJ (2014) Extracellular matrix stiffness and composition jointly regulate the induction of malignant phenotypes in mammary epithelium. Nat Mater 13(10):970–978. https://doi.org/10.1038/nmat4009 Bollyky PL, Falk BA, Wu RP, Buckner JH, Wight TN, Nepom GT (2009) Intact extracellular matrix and the maintenance of immune tolerance: high molecular weight hyaluronan promotes persistence of induced CD4+CD25+ regulatory T cells. J Leukoc Biol 86(3):567–572. https://doi.org/10.1189/jlb.0109001 Lim AR, Rathmell WK, Rathmell JC (2020) The tumor microenvironment as a metabolic barrier to effector T cells and immunotherapy. Elife. https://doi.org/10.7554/eLife.55185 Schurich A, Magalhaes I, Mattsson J (2019) Metabolic regulation of CAR T cell function by the hypoxic microenvironment in solid tumors. Immunotherapy 11(4):335–345. https://doi.org/10.2217/imt-2018-0141 Yadav UP, Singh T, Kumar P, Sharma P, Kaur H, Sharma S, Singh S, Kumar S, Mehta K (2020) Metabolic adaptations in cancer stem cells. Front Oncol 10:1010. https://doi.org/10.3389/fonc.2020.01010 Wang Y-A, Li X-L, Mo Y-Z, Fan C-M, Tang L, **ong F, Guo C, **ang B, Zhou M, Ma J, Huang X, Wu X, Li Y, Li G-Y, Zeng Z-Y, **ong W (2018) Effects of tumor metabolic microenvironment on regulatory T cells. Mol Cancer 17(1):168. https://doi.org/10.1186/s12943-018-0913-y VN, RS and ST wrote the article and prepared figures/table. FC assisted in writing-review and editing. EE conceived the concept, acquired funds, supervised and performed writing-review and editing. The authors declare no conflicts of interest. Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations. The original online version of this article was revised due to a retrospective Open Access order.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. Sasidharan Nair, V., Saleh, R., Toor, S.M. et al. Metabolic reprogramming of T regulatory cells in the hypoxic tumor microenvironment.
Cancer Immunol Immunother 70, 2103–2121 (2021). https://doi.org/10.1007/s00262-020-02842-y Received: Accepted: Published: Issue Date: DOI: https://doi.org/10.1007/s00262-020-02842-yChange history
07 July 2021
References
Author information
Authors and Affiliations
Contributions
Corresponding author
Ethics declarations
Conflict of interest
Additional information
Publisher's Note
Rights and permissions
About this article
Cite this article
Keywords